Tesfaye Techane Kelali1* and Aklilu Bezu Dinkesa2
1 Saint Paul’s Hospital Millennium Medical College, Oncology Nursing, Addis Ababa, Ethiopia
2 Northern Command Referral Hospital, Maternal and Child Health department, Mekelle, Ethiopia
*Corresponding Author: Tesfaye Techane Kelali, Saint Paul’s Hospital Millennium Medical College, Oncology Nursing, Addis Ababa, Ethiopia.
Received: February 21, 2022; Published: September 26, 2022
Citation: Tesfaye Techane Kelali and Aklilu Bezu Dinkesa. “Time to Cessation of Breastfeeding and Its Determinants among Mothers Who Have Children Birth to Three Years of Age in Mekelle Town, North Ethiopia: Retrospective Study”. Acta Scientific Paediatrics 5.10 (2022): 04-12.
Background: Data on time to cessation of breast feeding and its associated factors are scarce in Ethiopia. Hence, the present study aimed to assess the time to cessation of breast feeding and its determinants among mothers with children from birth to three years of age at Mekele town, Tigray.
Methods: Community-based cross-sectional retrospective study was conducted on 554 women, who have children from birth to three years of age in the in Mekelle town from March to July 2019. Participants were selected using systematic random sampling technique. Data was collected using interview administered questionnaire. The collected data were entered into Epi Info version 7.2 and exported to statistical package for the social science version 20.0 and analyzed using descriptive statistics, Bivariate and Multivariate Cox regressions.
Results: The overall incidence rate of cessation of breast feeding before 2 years of age was 3.017 per 100 person-months (95% CI: .027- .033). Number of children [AHR 1.4; 95%, CI: 1.005, 2.04], intended breast feeding duration [AHR 0.72; 95%, CI: 0.77, 0.91], type of first feeding [AHR 3.93; 95%, CI: 2.09, 7. 39] and timing of complementary feeding started [AHR 0.44; 95%, CI: 0.40, 0.75] were factors significantly associated with time to cessation of breast feeding before two years of age at p < 0.05.
Conclusion: The incidence rate of cessation of breast feeding before 2 years of age was relatively better when compared with previous study. However several factors affecting time to cessation of breast feeding were identified. These factors should be targeted to achieve appropriate duration of breast feeding.
Keywords: Cessation of Breastfeeding; Mothers-Child Pairs; Ethiopia.
AHR: Adjusted Hazard Ratio; BF: Breast Feeding; CBF: Cessation of Breast Feeding; CHR: Crude, Hazard Ratio; EBF: Exclusive Breast Feeding; HIV: Human Immunodeficiency Virus; SPSS: Statistical Package for Social Science
Breast feeding is one of the major public health strategies for improving infant and child morbidity and mortality because of its wide range benefits for both child and mother [1,2]. It is recommended that mothers should breast fed for 6 months exclusively and at least for 24 months along with appropriate complementary foods [1,3-5]. Exclusive and complete breast feeding (EBF) has shown to be the single most effective preventive intervention for reducing child mortality, with the potential of saving 1.3 million lives worldwide each year [6]. It also used to improve cognitive development and increases bonding with the mother [7], decrease the incidence or severity of bacterial meningitis, diarrhoea and late onset sepsis in preterm babies [2,8]. Studies showed that infants who did not breast fed had nearly four folds of developing series and complicated medical conditions than their counter parts [9].
Evidences have confirmed that breastfeeding is also beneficial for mothers in decreasing the chance of developing chronic illnesses [2,10], reducing the incidences of postpartum bleeding, maternal obesity, earlier return to pregnancy, and developing breast and ovarian cancer [10-12]. It has also many health benefits other than maternal and infant including economic and social benefits to the family, the healthcare system, and the employer [13]. Despite these all benefits of breast feeding for mother and child health, the percentage of children who are breastfed completely for 24 months was very low [14, 15]. For instance, in America 60% [14] and Iran 57% [15], of the mothers ceased breastfeeding before the children were two years of age. In Pakistan more than half (54%) of the mothers ceased breastfeeding before the children were 6 months of age [16]. In united Arab the median breastfeeding duration was only 8.6 months [17].
In African breastfeeding is supposed to be universal in which breast feeding was reported by more than 90% of mothers [18]. However, a significant number of mothers stop breast feeding before two year in Africa [19,20]. The percentage of infants who had not been breastfed for 24 months was 31.5% in Ethiopia [21], 48.9% in Tanzania [22] and 34.2%in Iran [23]. Early BF termination leads to diseases which contribute to higher number of death records among children less 2 years [19]. Another study also showed that early Cessation of breast feeding had been related with raised risks of upper respiratory tract infections [24].
Several studies revealed that time to cessation of breast feeding (CBF) were affected by maternal age, religion, marital status, education level [21,25] and child sex and place of delivery [21,26,27]. The maternal and child illness [21], maternal prior breastfeeding experience [19], HIV status of the mother [19,21,28], birth interval [29] were also factors associated with the time to CBF. Mother’s breastfeeding knowledge and attitude were also reported as significant factors of the time to CBF [30].
Assessing the time to CBF and identifying its contributing factors is crucial to promote exclusive and complete breastfeeding through taking appropriate actions. However, data on time to CBF and its associated factors are scare in Ethiopia. Hence, there are strong needs to evaluate the time of breastfeeding cessation and its determinants among breast feeding mothers in the country. The present study was aimed to assess the time to cessation of breast feeding and its determinants among mothers with children from birth to three years of age at Mekelle town, North Ethiopia.
The study was conducted in Mekelle town which is located at the distance of about 780 km from Addis Ababa, capital city of Ethiopia. Mekelle is a mid-sized city with total population of around 400,000. The city is divided into seven local administrations sub cities including Hawelti, Adi-Haki, Kedamay Weyane, Hadnet, Ayder, Semien and Quiha. There are 8 health centers, one referral teaching hospital and three general hospitals owned by government and 4 general hospitals, 38 clinics owned by private organizations in the city. The study was conducted from March to July 2019.
Community-based cross-sectional retrospective study design was conducted.
Source population of the study was all women who have children from birth to three years of age in the in Mekelle town.
Study Population of the study was all women who have children from birth to three years of age in the three randomly selected kebele; namely: Adi-Haki, Ayder, Kedamay weyane kebele in the in Mekelle town.
Study unit of the study was all randomly selected women who have children from birth to three years of age in the in Mekelle town.
All mothers who have children from birth to three years of age in the in Mekelle town were included.
Sample size of this particular study was calculated using single population proportion formula by consideration assumption
Then, design effect of 1.5 was used resulting 503. Finally, 10% for possible non response was added resulting 554. In selecting study units, first, the total sample size was allocated proportionally to number of women who have children from birth to three years of age in each Kebele. Then, an individual participant was selected using the systematic random sampling technique with every 6th households.
The dependent variable of this study was Time to cessation of breastfeeding whereas independent variables were maternal age, maternal educational status, employment, ethnicity, religion, marital status, place of delivery, mode of delivery, Sex of children, number of children, ANC follow up, bottle feeding, breastfeeding counselling after delivery, HIV status of the mother, Knowledge and attitude of mothers about breastfeeding.
Data were collected using face to face interview by 5 trained BSc. nurses. The questionnaires were adapted from previous studies conducted in the same country [21]. Some literatures on breastfeeding were also used to adapted factors related questions. The questionnaire comprised socio-demographic related questions, health service related questions, and obstetric related questions. The time to CBF data were collected from mothers with index children aged two to three years. The mothers were asked the time on which they ceased breastfeeding. The date of birth of child was taken as the starting point of the retrospective study. The length of time was measured from birth to 3 years of age and was taken to be the survival time for those who had experienced the event of interest. Participants who ceased breastfeeding before 24 months was an event of interest, and those who were breastfed during data collection were considered as right censored.
Early cessation of breastfeeding - Mothers stops of breastfeeding before their children are two years of age.
Adequate knowledge- If a mother answered at least nine of the twelve knowledge assessment questions correctly.
Favorable attitude-If a mother responded positively to at least nine of the twelve attitudes assessment questions [21].
The collected data was checked, coded and entered using EPIdata version 3.1 and then transferred to statistical package for social science version 23 (SPSS). Frequency, percentage and mean were analysed using descriptive statistics and presented in text and tables. Breastfeeding failure probability was investigated using Life Table. Bivariate Cox proportional regression models were done to see the relation of factors with cessation of breast feeding, and multivariate Cox proportional regression was used to control the effect of cofounders. All variables with p-value less than 0.25 in the Bivariate Cox proportional regression analysis were fitted to the multivariate Cox proportional regression. Variables with P-value < 0.05 in the multivariate Cox regression analysis were considered as statistically significant factors for the cessation of breast feeding before 2 years.
In the present study, out of total 554 samples, 503 mother-child pairs were involved in the study making response rate 90.8%. The mean age of the study participants was 29.2 (sd = 5.26) years. Most of the mothers were married 464 (92.2%) and more than half of them were housewives 268 (53.3%). Regarding education level only 180 (35.8%) of participants were completed their secondary school (Table 1). Almost all of 500 (99.4%) participants had adequate knowledge, were as almost three fourth 361 (75.0%) of them had satisfactory attitude (Table 2).
In this study duration of breastfeeding in almost half of infants was less than 24 months. The overall person-time of CBF observation was 10969 person- months. The overall incidence rate of CBF before 2 years of age was 3.017 per 100 person-months (95% CI: .027-.033). The cumulative survival probability in life table indicated that the percentage of children who remained on breastfeeding for the first two years was 54.3% (Figure 1). The cumulative survival probability in life table indicated that the percentage of children who remained on breastfeeding for the first month to three years was 19.9%. The cumulative failure probability presented in life table was 40.36% with CI = 0.3622 - 0.4478 for children breast feeding failure before 24 months (Table 3).
Table 1: Socio-demographic characteristics of mothers who have children age from birth to three years, in Mekelle town northern, Ethiopia 2019 (n = 503).
Table 2: Health and health service-related characteristics of mothers who have children age from birth to three years at Mekelle town, northern Ethiopia, 2019 (n = 503).
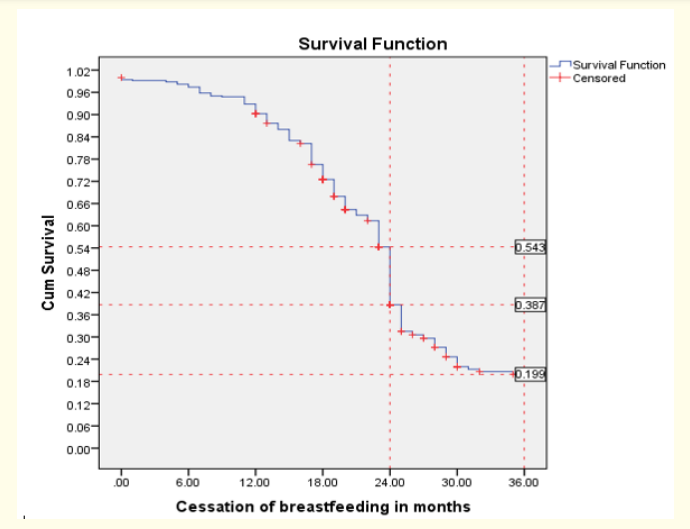
Figure 1: Survival of breastfeeding among mothers who have children from birth to three years of age at Mekelle, Northern Ethiopia in 2019.
In the Bivariate Cox regression analysis Education level, number of children, BF counselling during ANC, BF counselling after delivery, intended breast feeding duration, mothers’ HIV status, type of first feeding and timing of complimentary feeding started were factors associated with time to CBF before two years of age at p < 0.25. However, in multivariate Cox regression analysis number of children [AHR 1.4; 95%, CI: 1.005, 2.04], intended breast feeding duration [AHR 0.72; 95%, CI: 0.77, 0.91], type of first feeding [AHR 3.93; 95%, CI: 2.09, 7. 39] and timing of complimentary feeding started [AHR 0.44; 95%, CI: 0.40, 0.75] were factors significantly associated with time to CBF before two years of age at p < 0.05 (Table 4).
In the present study 503 mother-child pairs were followed retrospectively for a total of 10969 person-months. The overall incidence rate of CBF before 2 years of age was 3.017 person-months. In compare to other previous studies this finding better. The incidence rate of CBF before 24 months was 16.02 person-months in Iran [23] and 13.70 person-months in Ethiopia [21]. The possible explanation for better finding in the present study could be sociodemographic differences and difference in number of studied population. The study in Iran was conducted among urban and rural residents indicating that resident of lactating a mother is positive factors for appropriate time to CBF. In addition only 395 motherchild pairs were involved the study conducted in Iran which was lower than the current mother-child pairs (503). The difference might be also due difference in the attitude on breastfeeding. In the current study three fourth 377 (75.0%) of participants had favourable attitude which was better finding than the finding 252 (52.2%) of prior study [21].
Table 3: Life table of cumulative failure estimate of factors associated with time to cessation of breastfeeding among mothers who have children from birth to three years of age in Mekelle town, north Ethiopia, 2018/2019.
Table 4: Bivariate and multivariate cox regression of CBF among mothers who have children aged from birth to three years at Mekelle, northern Ethiopia 2019 (n = 503).
In agreement to studies conducted in Iran [23] and Tanzania [22], the present study revealed that more than half (54.3%) of women ceased breast feeding before 24 months. However, this finding is higher than study conducted in Debre Markos [21] and national average estimated prevalence [31]. The variation may be due to the fact that the present study considered only urban residents, while the national study considered both urban and rural residents.
In the prior studies HIV status of mothers were significantly associated with time to CBF [19,21]. However, this was not true for the present study in which HIV status of mothers was not significantly associated with time to CBF. The difference may be due to small number of HIV positive mothers in the present study. In line with previous studies conducted in Ethiopia [21] and Bangladesh [32], number of children was significantly associated with time to CBF. The possible explanation for this congruent finding could be the fact that mothers with small number of children have enough time breasts feed and continue breastfeeding till to recommended time or two years.
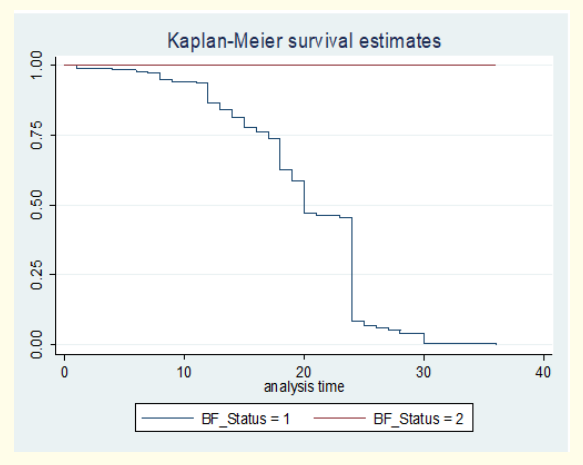
Figure 2: Kaplan-Meier estimate of survival on cessation of breastfeeding among mothers who have children from birth to three years of age in National reginal state of Tigray, Mekelle town, northern Ethiopia, 2019.
The potential limitations of this study that should be considered in the interpretation of the present findings are: First, the study was based on participants’ reports of data and therefore, there may be recall bias. Second, the cross-sectional design of the study limits the ability to draw conclusions about causality or directions of the relationships.
The overall incidence rate of CBF before 2 years of age was 3.017 person-months which was relatively better in compare with previous study. The proportion of children who remained on breastfeeding for the first two years was 54.3%. Number of children, intended breast feeding duration, first feeding and timing of complimentary feeding started were the identified factors associated with time to CBF. Hence, these factors should be targeted and health care providers should pay attentions to tackle the factors to promote appropriate duration of breast feeding.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical approval was obtained from Mekelle University, College of health sciences, and School of nursing. Informed consent was obtained from participants after they were informed about the objectives of the study. Confidentiality and privacy of participants was also ensured.
Our deepest gratitude goes to Mekelle University, College of Health sciences, School of nursing for giving us the opportunity to conduct this study. We would also like to extend our sincere gratitude to the data collectors and the study participants for being involved in the study.
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. All authors approved the final version for submission.
This study was conducted in collaboration with Mekelle University. Every step of the study was followed by Mekelle University, College of Health sciences, school of Nursing. The university has no role in designing, analysis and writing of the study.
The authors declare that they have no competing interests.
Copyright: © 2022 Tesfaye Techane Kelali and Aklilu Bezu Dinkesa. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.