Himanshu Soni1*, Manoj Bhaskar2, Joseph Lijo3, Arjun Shenoy3 and Yash Chadha4
1MDS, Fellow in Cranio-Maxillo-Facial Trauma, Fellow in Head and Neck Oncology,
Mahatma Gandhi Cancer Hospital Miraj, Maharashtra, India
2MDS, Head of the Unit of Oral and Maxillofacial Surgery, Director of Centre for
Excellence for Fellowship in Cranio-Maxillo-Facial Trauma, Elite Mission Hospital,
Thrissur, Kerala, India
3MDS, Consultant Maxillofacial Surgeon, Elite Mission Hospital, Thrissur, Kerala,
India
4MDS, Fellow in Cranio-Maxillo-Facial Trauma, BL Kapur Hospital, Delhi, India
*Corresponding Author: Himanshu Soni, MDS, Fellow in Cranio-Maxillo-Facial Trauma, Fellow in Head and Neck Oncology, Mahatma Gandhi Cancer Hospital Miraj, Maharashtra, India.
Received: January 25, 2021; Published: February 16, 2021
Zygomatico-coronoid ankylosis refers to fibrous or bony fusion between zygomatic arch and coronoid process of mandible which results from inadequate or delayed treatment caused by fractures of upper and lower facial fractures due to RTA, personal violence, sports injury and gunshots injury. ZCA is unprecedented kind of extra-articular ankylosis. We report a case of posttraumatic facial injury in 40year old male with untreated left midface fracture resulting in trismus at initial presentation. Radiographic evaluation shows mass of heterotrophic bone formation due to untreated left midface and lower face fracture resulting in bony fusion between zygomatic arch and coronoid process. Coronoidectomy was accomplished with an intraoral approach under general anesthesia followed by aggressive physiotherapy. Immediate and late postoperatively it produced good functional and esthetic outcome.
Keywords: Post Traumatic Deformity; Trismus; ZMC Fracture; Coronoid Fracture; Intraoral Coronoidectomy; Zygomatico Coronoid Ankylosis
Facial trauma is generally associated with road traffic accidents, falls, assaults, and sports related trauma. Facial bones most frequently involved in such accidents are Mid-face, mandible and TMJ region. The complicated nature of the temporomandibular joint area and its anatomical proximity to vital craniofacial systems makes analysis and remedy of any Tmj disorder, mainly difficult [1].
Trauma to TMJ region causes facial deformity, bony fusion, growth impairment and osteoarthritis [2]. This has an bad impact on the practical, esthetic further to social life of the man or woman.
Trismus is described as restricted mouth or jaw opening. There are two varieties of Temporomandibular joint (TMJ) ankylosis intra-articular or true ankylosis and extra-articular or false ankylosis. Fibrous or bony adhesion between the coronoid process and the zygomatic arch is a rare cause of extracapsular/extra-articular ankylosis [3]. In many cases while there is trouble of mouth opening coronoid system can be unnoticed, due to the fact that attention is generally focused at the TMJ [4]. Zygomatico-coronoid ankylosis may also arise due to upper facial fractures including ZMC complex fracture or mandibular fracture, inadequate or delayed treatment of zygomatic complex, or combination of upper and lower facial bone fracture [3,5].
Enlargement of the coronoid process of the mandible was first described by Langenbeck in 1853, and joint formation between the coronoid process and the zygoma was first described by Jacob in 1899. Zygomatico coronoid ankylosis was first described by Brown and Peterson. The authentic incidence of this circumstance may be even better. Zygomatico coronoid ankylosis might also have been encountered by way of many clinicians, and but may additionally have been misdiagnosed or not noted. The remedy consists of surgical excision of the coronoid manner observed via full of life jaw starting physical games [4].
A 40-year male presented to the maxillofacial and oral surgery outpatient department of the elite mission hospital with complain of inability to open his mouth in the form of trismus. He gave a history of being met with a road traffic accident 4 weeks back and had sustained trauma to the left side of the face.
Extra-oral examination revealed despair over the left zygomatic arch area. There was no substantiation of blurring of vision or numbness over the cheek. Inter-incisal mouth opening became less than 5mm and the patient couldn't perform any protrusive or lateral movements (Figure 1). Intra-orally stable occlusion with no other deformities was noted.

Figure 1: Pre-op mouth opening less than 5 mm.
Figure 2a and 2b: 3D CT reconstruction showing left zygomatic arch fracture and left coronoid process fracture ankylosis.
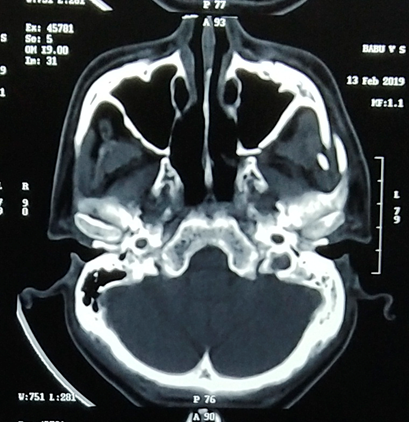
Figure 2c: Axial CT shows left zygomatic arch fracture and left coronoid process fracture.
After basic investigation and pre-anesthetic workup, due to relative contraindication of nasal intubation, tracheostomy was planned (Figure 3). Awake tracheostomy under local anesthesia was performed under aspetic condition. After standard preparation of the patient, local anesthesia with adrenaline was administered. Intraoral keens incision was placed in the region of 1st molar approximately 5 mm above mucogingival junction over left labial vestibule area. After careful dissection, Bristow’s elevator was placed and left zygoma elevation was attempted. But since the fracture was 4 weeks old we didn’t get the satisfactory elevation. Following which a prolonged C shaped incision was placed extending from external oblique ridge up to coronoid process along the anterior border of ramus was made which gave us adequate exposure to address ankylotic mass. Fractured Coronoid process is usually placed superiorly due action of temporalis muscle. The temporomandibular joint was not affected. For osteotomy a straight burr was used over the left side to separate coronoid process from the Mandibular ramus. Chisel and mallet have been used for dysfunction of coronoid and zygomatic bone through its internal aspect. Coronoid process along with temporalis muscle attached through a mass of bone to zygoma was excised (Figure 5). The site was irrigated with betadine and saline. Closure was done with interrupted vicyrl sutures (Figure 6). Immediate post-op the patient's interincisal opening was noted to be 35 mm (Figure 4).

Figure 3: Tracheostomy was performed due to relative contraindication to nasal intubation.
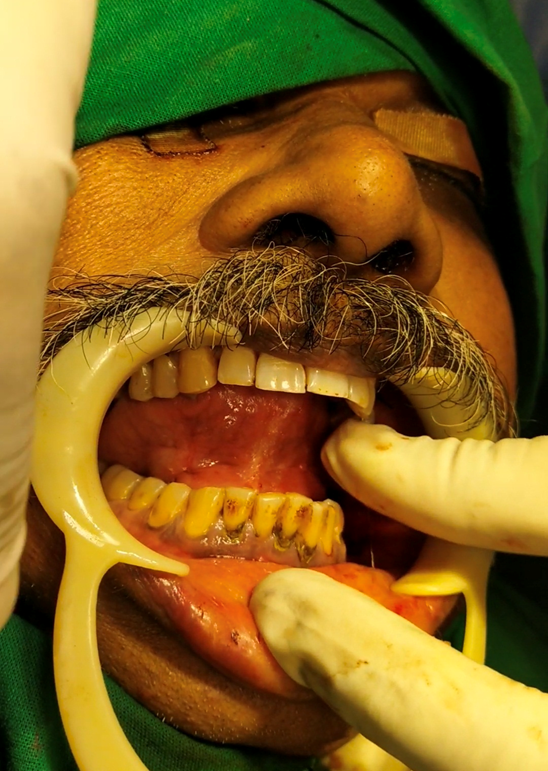
Figure 4: Mouth opening immediately following coronoidectomy.

Figure 5: Excised coronoid process along with stripped temporalis muscle.

Figure 6: Incision was closed with 3-0 vicryl with a watertight closure.
Sequence of events which leads to unusual condition of zygomatico- coronoid ankylosis is yet to be discovered. A pathological condition in which bone forms over non-skeletal tissues is defined as heterotopic bone formation. Most common causative factors involves trauma, infection and neurogenic but it can be multifactorial. In our case trauma was the etiological factor for ZCA. Stimulation of mesenchymal pluripotent cells to differentiate into osteoblastic and chondroblastic stem cells following trauma causing heterotopic bone formation was one of the theories put forward. Heterotopic bone formation can take place in any part of body mainly involving joints, but certainly it is rarely encountered in facial region. Examples of heterotopic bone formation in the facial region include ossification of the stylohyoid ligament [7], periosteal ossification following subperiosteal haemorrhage or infection, and myositis ossificans of the masseter muscles [8].
Coronoidectomy remains the single best surgical option for extra-auricular ankylosis. Depending upon the extent and location of ankylosis approached can be intra or extra-oral. One of the advantages of extra-oral approach is accessibility with scar and facial nerve injury as disadvantage. Intraoral approach may be tedious and access could be very difficult. Also, through intraoral approach, due to limited access surgeon should be very careful to stabilize the coronoid process before osteotomy. Coronoid process serves as an insertion for strong temporalis muscles. Muscle contracts and would pull the fragment in upward direction making it difficult for surgeons to trace it. We stabilized the coronoid process with towel clip and bone holding forceps before osteotomy.
Our patient complained of restricted mouth opening following trauma. Presence of ankylotic mass with other clinical finding and prevention of visible scar over the face by patient left us with no choice but to plan for intraoral approach to address the bony mass. Early mobilization of joint with jaw exercise, application of mouth gag under GA and regular long term follow-up are outmost necessary.
Aggressive physiotherapy with follow-up protocol was explained to the patient upon discharged. Patient was followed up every week for 1st month than 3rd and 6th month. Mouth opening of 35 mm was achieved at the end of 3rd month with adequate mandibular movements and stable occlusion.
Postoperatively patient was schedule for active physiotherapy from day 1 to day 5. At the time of discharge patients inter-incisal mouth opening was 32 mm. We could achieve a stable mouth opening of 30 mm after 6 weeks postoperatively. All mandibular jaw movements and function were restored.
The most common etiological factor for ZCA is inadequate treatment to previous trauma to upper and lower jaw. This is consistent with our case; patient gave history of previous trauma with restricted mouth opening at presentation. Intraoral resection of ankylotic mass with early mobilization of joint and physiotherapy produced good functional and esthetic results.
ZCA being not common entity, surgeons should have thorough knowledge for same. Clinical examination and CT scan remains the gold standard for diagnosis. Furthermore, it is advised that any trauma to upper or law jaw and TMJ joint space, coronoid ankylosis should be evaluated and considered in differential diagnosis. Physiotherapy in postoperative period with follow-up is mandatory to prevent reankylosis.
None.
Citation: Himanshu Soni., et al. “Coronoidectomy in Management of Post Traumatic Zygomatico-Coronoid Ankylosis - A Case Report". Acta Scientific Dental Sciences 5.3 (2021): 71-75.
Copyright: © 2021 Himanshu Soni., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.