Aissata Barry1,2*, Mamadou Moustapha Diop1,2, Kaba Bangoura1,2, Salématou Hassimiou Camara1,2, M’mah Aminata Bangoura2,3 and Moustapha Kouyaté1,2
1Donka National Hospital, Conakry, Guinea
2Gamal Abdel Nasser University, Conakry, Guinea
3Institute of Nutrition and Child Health, Conakry, Guinea
*Corresponding Author: Aissata Barry, Donka National Hospital, Conakry, Guinea.
Received: December 25, 2024; Published: January 07, 2025
Citation: Aissata Barry., et al. “Epidemiological, Clinical and Haematological Profile of Patients Transfused at the Paediatric Oncology Unit of Donka Hospital". Acta Scientific Paediatrics 8.1 (2025): 22-26.
Introduction: The aim of this study was to investigate the epidemiological, clinical and haematological profile of patients transfused at the paediatric oncology unit of the Donka National Hospital.
Methods: The paediatric ward of the Donka national hospital was used as the setting for this study. This was a prospective and descriptive study lasting 6 months from 1 March to 31 August 2021.
Results: We recorded 135 patients, 92 of whom were transfused (68.1%). 61 (66.3%) were boys and 31 were girls (33.7%). Children aged less than or equal to 5 years were more represented with 38.04% of cases, followed by the 11 to 15 age group with 29.35%. Pallor (91 cases) and physical asthenia (76) were the most frequent reasons for consultation. 40 patients had sickle cell disease, 26 had acute lymphoblastic leukaemia and 15 had acute myeloblastic leukaemia. Mean haemoglobin: 5.26 ± 1.47 g/dl.
Conclusion: Blood transfusion is a frequent therapeutic procedure in paediatrics. The results of our work could serve as a starting point for an analysis of labile blood product prescriptions, and thus contribute to improving practices.
Keywords: Anemia; Blood Transfusion; Paediatric Oncology
Blood transfusion is a medical treatment in which donated blood (collected and prepared from a healthy person - a donor) is administered to the patient being treated, (in the form of blood components, blood derivatives or in rare situations) [1]. Recourse to blood product transfusion is frequent in paediatrics, and constantly increasing [2]. It is an integral part of supportive therapy in oncology [3]. Transfusion remains a key element in the management of patients with haemopathies. The availability and quality of blood products have a considerable prognostic role. Red blood cell transfusions increase oxygen levels to limit the deleterious effects of oxygen deficiency [4]. A 2008 study showed that a prolonged haemoglobin level of less than 11g/dL was significantly associated with excess mortality. When an oncology patient is receiving treatment with the therapeutic objective of prolonged survival, it is legal and even appropriate to have recourse to transfusions of packed red blood cells (PRBCs) if this proves necessary [5]. In France, haematology-oncology is considered to be the pathological area most frequently inducing transfusion [3]. Like any therapeutic treatment, transfusion requires a careful assessment of the benefit/risk balance, which is taken into account in the development of regularly published recommendations on transfusion practice [6]. Despite the recommendations, there is still considerable diversity in transfusion practices [2]. In France, a study of palliative care decisions in haemato-oncology departments showed that 47% of children had received a blood transfusion [8].
Another study on the transfusion needs of paediatric services showed that out of 1607 labile blood products, 806 red blood cell concentrates (RBC), 670 platelet concentrates (PC) and 131 units of therapeutic plasma had been distributed to 233 children (5.3% of transfusions carried out over the year at the CHU). The paediatric departments with the highest blood consumption were: haemato-oncology (68.2%) compared with intensive care (15.4%) and surgery (10.2%) [8]. It therefore seems legitimate to ensure maximum transfusion safety, which implies logistical constraints (supply, processing, financial, etc.). This approach must not compromise the quality of labile blood products (LBS). To meet these constraints as satisfactorily as possible, we need to know the transfusion requirements and the profile of patients receiving transfusions. However, there is very little data on the epidemiology of blood transfusion in children. It was with this in mind that we undertook this study.
To study the epidemiological, clinical and haematological profile of patients transfused at the paediatric oncology unit of the Donka national hospital.
The paediatrics department of the Donka national hospital served as our setting for this study. It was a prospective and descriptive study lasting 6 months from 1 March to 31 August 2021. It focused on children admitted to the paediatric oncology unit and who received a blood transfusion during our study period.
We included in this study all children aged 0 to 15 years who received a transfusion at the paediatric oncology unit of the Donka national hospital.
We carried out an exhaustive recruitment of all the children, taking into account our inclusion criteria.
We studied the following variables
We recorded 135 patients hospitalised during the study period, 92 of whom were transfused (68.15%). Of the patients transfused, 61 (66.3%) were boys and 31 (33.7%) were girls. Children aged less than or equal to 5 years were more represented with 38.04% of cases, followed by the 11 to 15 age group with 29.35%.
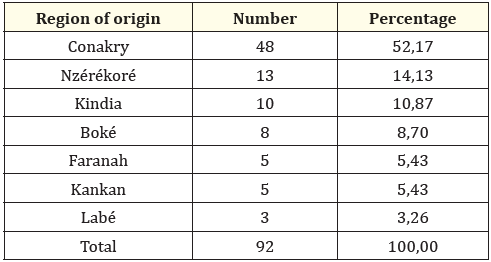
Table 1: Distribution of the 92 patients transfused at the paediatric haemato-oncology unit of the Donka national hospital according to region of origin.
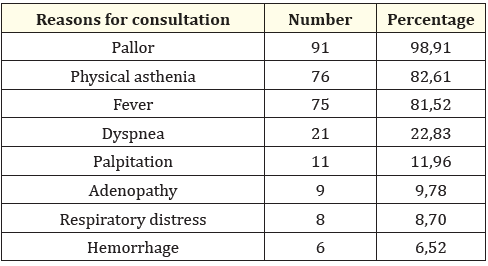
Table 2: Frequency of reasons for consultation for 92 patients transfused at Paediatric Haemato-Oncology Unit, Donka National Hospital.
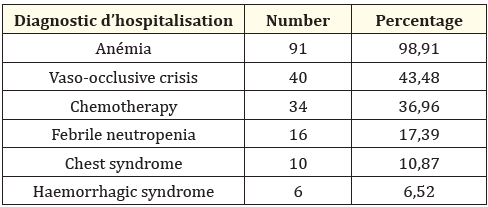
Table 3: Frequency of hospitalisation diagnosis of 92 patients transfused at the paediatric haematology-oncology unit of the Donka national hospital.
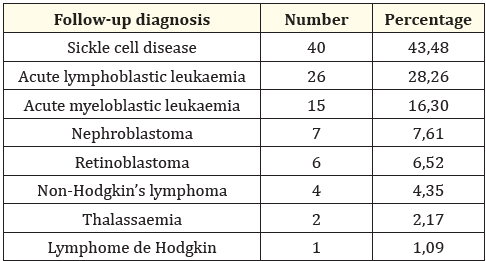
Table 4: Frequency of follow-up diagnosis of 92 patients transfused at the paediatric haematology-oncology unit of the Donka national hospital, by follow-up diagnosis
Of 70 patients with chronic renal failure initiated on haemodialysis, the main indication for initiation of haemodialysis was uraemic intoxication in 52 cases (74.29%).
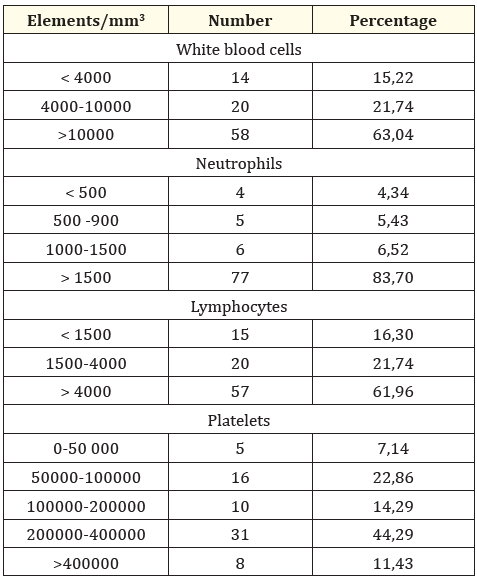
Table 5: Distribution of 92 patients transfused according to blood count results. Mean haemoglobin: 5,26 ± 1,47 g/dl Extremes : 1,47 et 9,7 g/dl.
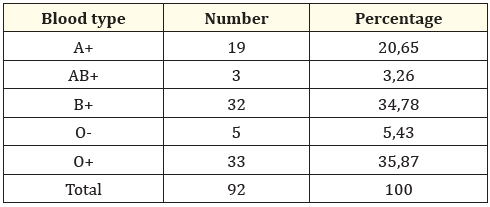
Table 6: Distribution of 92 cases of transfusion in the haematology oncology unit, by blood group.
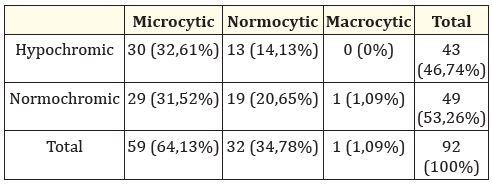
Table 7: Distribution of 92 patients transfused according to type of anaemia.
Blood transfusion is a frequent therapeutic procedure in paediatrics. This survey enabled us to describe transfusion modalities in paediatric haemato-oncology facilities at the CHU Donka. The rate of patients transfused was 68.15%. The result of our study is superior to that of Sun Y., et al. [7] in China in their study in 2016 found an average transfusion rate of 13.02% in neonates. According to the literature, children and pregnant women use 75% of the blood supply in sub-Saharan Africa but generally face blood shortages [8,9]. This result could be explained by the fact that, on the one hand, most of our patients were hospitalised for cancer and sickle cell disease and, on the other hand, the paediatric haematology and oncology unit is the only unit (national reference centre) for paediatric haemopathies. This difference could be explained by the context, the place of study and the size of the sample. The predominance of males was 66.3%. This was in contrast to Dokekias AE., et al. [10] who reported 59 female patients (52.7%) and 53 male patients (47.3%). We found no relationship between gender and transfusion requirements. The high rate of transfusion cases in children under 5 years of age could be justified by the fact that these children are most at risk. This age group is the prime target for anaemia-causing diseases such as acute lymphoblastic leukaemia and Burkitt's lymphoma. The frequency of transfusions decreases with age. Most of the patients lived in Conakry; this can be explained by the fact that the site of our study is in Conakry and is the only referral centre for the treatment of childhood cancer in Guinea, forcing patients from the interior of the country to come to Conakry for treatment, but also by the fact that these were patients to be followed up over a long period, obliging them to stay there during the treatment period. The relatively high cost of evacuation is a factor that limits compliance with the decision to evacuate from other towns. Pallor, physical asthenia, fever and dyspnoea were the main reasons for consultation. The high rate of pallor, physical asthenia, fever and dyspnoea would be due to the fact that these signs are symptoms of anaemia but also of vaso-occlusive crises. Sickle cell disease, acute lymphoblastic leukaemia and myeloblastic leukaemia were the main diagnoses that led patients to severe anaemia requiring transfusion. Fukiau GM., et al. [11] in Kinshasa noted malaria (87.1%), sickle cell disease (4.1%), pneumonia (3.4%) and malnutrition (0.8%) as pathologies associated with anaemia. This is justified by the fact that these pathologies cause anaemia, most often leading to blood transfusions. The majority of patients had a haemoglobin level of less than 7 g/dl, i.e. 90.22%, with a mean of 5.24 ± 1.48 g/dl and extremes of 1.47 and 9.7 g/dl. This result is comparable to that of Maitland K., et al. in 2019 who reported that 75.7% of children had a haemoglobin level of less than 4 g/dl [12]. Dokekias AE., et al. [10]. Mean initial Hb 6.1 g/dl (extremes: 3.2 and 8.6).
In our study, only 5.43% had Rh-. Hypochromic microcytic anaemia was the most common type (32.61%) followed by normochromic normocytic anaemia (31.52%). Daniel K.K., et al. [13] in Cameroon in 2013 found 48.5% microcytic hypochromic anaemia followed by normocytic normochromic anaemia 22%.
Blood transfusion is a frequent therapeutic procedure in paediatrics. The children were predominantly male, with a predominance in the under-five age group. Pallor, physical asthenia, fever and dyspnoea were the main reasons for consultation. Hypochromic microcytic anaemia was the most common type, followed by normochromic normocytic anaemia. Anemia, chemotherapy, thrombocytopenia, chest syndrome and haemorrhagic syndrome were the main transfusion indicators. The results of our work could serve as a starting point for an analysis of labile blood product prescriptions, and thus help to improve practices.
Copyright: © 2025 Aissata Barry., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.