Rajshree D Katke1*, Bhawana Kalwar2, Shubhangi Nawarange3, Sanchari Pal4, Pratiksha Khamkar2 and Vishal Waghmare2
1Professor and Head of Unit, Department of Obstetrics and Gynaecology, Grant Government Medical College and St. George’s Hospital, Mumbai, India
2Junior Resident, Department of Obstetrics and Gynaecology, Grant Government Medical College and St. George’s Hospital, Mumbai, India
3Assistant Professor, Department of Obstetrics and Gynaecology, Grant Government Medical College and St. George’s Hospital, Mumbai, India
4Senior Resident, Department of Obstetrics and Gynaecology, Grant Government Medical College and St. George’s Hospital, Mumbai, India
*Corresponding Author: Rajshree D Katke, Professor and Head of Unit, Department of Obstetrics and Gynaecology, Grant Government Medical College and St. George’s Hospital, Mumbai, India.
Received: December 11, 2024; Published: December 26, 2024
Citation: Rajshree D Katke., et al. “A Rare Case Report of a Giant Mucinous Cystadenoma in a Woman with Post Hysterectomy Status”. Acta Scientific Paediatrics 8.1 (2025): 02-08.
Epithelial ovarian neoplasms are common and account for 60% of all ovarian tumours and almost 40% of them are benign. Mucinous cystadenomas are a common benign neoplasm of the ovaries that can grow much larger than other adnexal masses and are recognised as precursors of ovarian cancer and that may slowly transform into borderline tumours and invasive ovarian cancer. Prompt and accurate treatment is essential as these tumours can grow to massive sizes and be potentially lethal if left untreated. These tumours occur most commonly in women in their twenties to forties, but occurrences in adolescent and even premenarchal girls, as well as postmenopausal patients, have been documented as seen in our case report [1]. Here we describe a rare case of Giant Ovarian Mucinous Cystadenoma in a post Hysterectomised elderly woman managed promptly by surgical intervention keeping in mind the malignant potential of such ovarian tumours in post hysterectomised women.
Keywords: Bleeding; Urinary Bladder
A 57-year-old female, para 3, living 3 reported to the Gynaecology outpatient at St. George’s Hospital, Mumbai with complaints of bloating, constipation and a gradual increase in abdominal girth over 6 months associated with pain in the abdomen which was insidious in onset, and was gradually progressive causing discomfort to the patient. Patient is Hysterectomised 15 years back for Abnormal Uterine Bleeding and was a known case of Hypertension for 10 years controlled on triple antihypertensives. On general physical examination, the patient was moderately built and well nourished with no h/o loss of appetite or significant weight loss. On examination, she was vitally stable. On per abdominal examination, the abdomen was distended and soft with no signs of acute abdomen: 20-24 weeks Size mass felt, occupying majorly the left inguinal region extending to hypogastric and a part of right inguinal region reaching up to mid umbilical region above having a smooth surface, irregular ill-defined margins, cystic in consistency. The mass was mobile and was not adherent to the pelvic wall. A per speculum examination showed a healthy vault while on a bimanual per vaginal examination, a mass approximately of size around 14 x 12 cm palpated through the anterior wall of the vaginal wall. Ultrasonography of abdomen and pelvis was done which was s/o large pelvic space-occupying lesion with multi septations present within, situated just above urinary bladder in the left paramedian plane of size 12.8 x 11.7cm x 7cm (ovarian neoplasm).
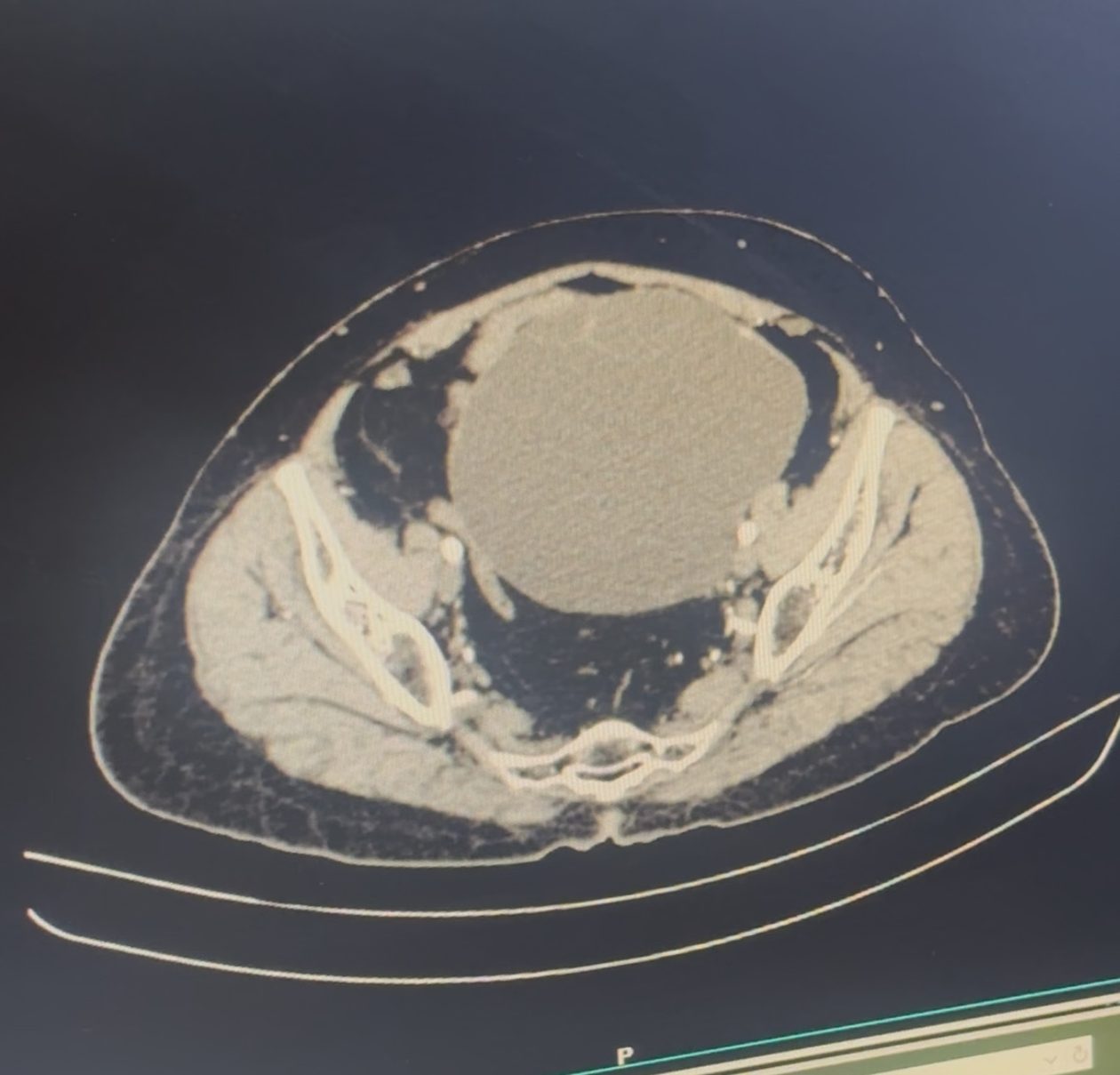
Figure 1: Contrast enhanced computed tomography scan showing ovarian mass of probable neoplastic etiology.
All routine investigations were sent and were within normal limits. Amongst the Tumor markers CA125 was 12.7 and rest were all within the normal limits. After correlating the age of the patient, history with clinical findings, imaging and the level of tumour markers the diagnosis was suspected to be left-sided ovarian mucinous cystadenoma probably benign in nature, Considering the size of the tumour and postmenopausal age group and the possibility of malignancy, the decision was taken to take patient for exploratory laprotomy with left ovarectomy with SOS any other extension of the procedure with an intra-operative Frozen section Biopsy to confirm the nature of the tumor. All routine pre-anaesthetic workups were done. The patient was taken for the surgery.

Figure 2: Intraoperative tumour densely adherent to adjacent structures.
Intraoperative findings showed no e/o any Ascites. A large left ovarian cystic multiloculated mass measuring 13x 14 cm with a smooth surface and intact capsule was seen.

Figure 3: Intraoperative huge tumour adherent to the bladder.
The uterus was not seen in situ (post hysterectomised status) and the right ovary and fallopian tube were normal. The left fallopian tube was stretched along with the tumour. The cystic tumour was found to be in a torsion state with around two and half turns and was adherent to the underlying bowel and bladder.

Figure 4: Ovarian cyst after adhesiolysis and freeing from adjacent structures.
Careful dissection was done to separate the cyst from the viscera and the specimen was removed in toto. The specimen was sent for intraoperative Frozen section Biopsy which showed Benign Ovarian Mucinous Cystadenoma which confirmed the diagnosis. She had a left Ovarectomy with left salpingectomy with Right-sided Salpingoopherectomy. The peritoneum and visceras along with the appendix were traced to look for any e/o Pesudomyxoma Peritonei and SOS Appendicectomy if needed. No evidence of other abnormalities were noted. The patient withstood the procedure well. Post-operative recovery was uneventful. She was discharged on day 10 of post-op with no complaints. On follow up the patient is doing well.
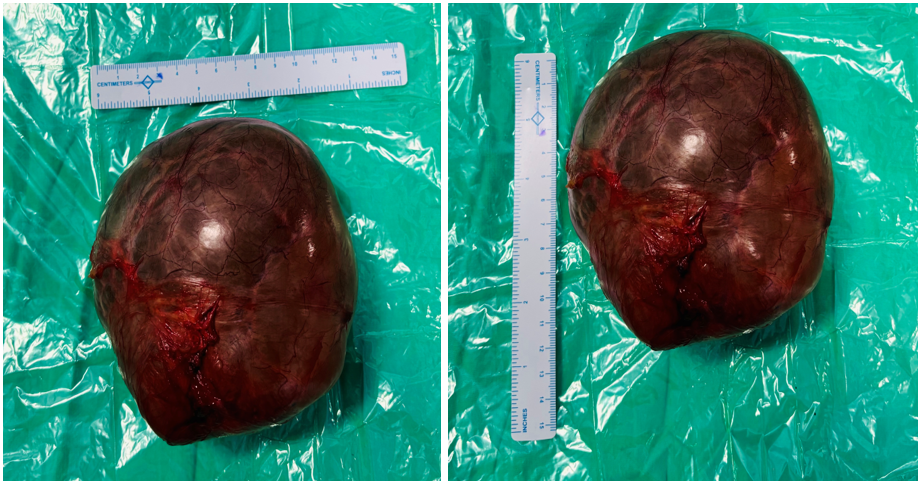
Figure 5: Post operative huge ovarian mucinous cystadenoma.
Of all the ovarian tumours, mucinous cystadenomas account for 15%-20% and are among the most common benign ovarian neoplasms [2]. These tumours arise from the ovarian surface epithelium and have smooth inner and outer thin walls. Specifically, benign mucinous cystadenomas comprise 80% forming the majority of ovarian mucinous tumors; 10% of these tumors are found to be malignant and the remaining 10% are borderline [3]. A striking feature of these benign mucinous cystadenomas is that they can become massive in size ranging from 5 to 28 cm with larger sizes causing compressive effects ranging from pressure, pain, bloating, and urinary symptoms to further increasing the risk of malignancy [4]. When cysts begin to enlarge and invade surrounding structures, a patient may begin to present with varying symptoms of a mass effect as described to severe life-threatening complications, such as ovarian torsion, cystic rupture, and haemorrhage [5].
In the modern era of medicine, such huge mucinous ovarian tumours have become rare in the current medical practice, as most of the cases are diagnosed early during routine gynaecological examinations or incidental finding on the ultrasound examination of the pelvis and abdomen. One such rare case of a 40 year female P1L1, postmenopausal female presented with complaint of abdominal distension and pain since 6 months. Her tumor markers showed slightly raised CEA with rest all within normal limit. On per abdomen examination - abdomen was found to be markedly overdistended all over with the skin overstretched with prominent veins on it. On palpation there is a large palpable mass arising from the pelvis extending to the epigastrium and extended diffusely in both the flanks and all over the abdomen with firm to cystic Consistency was cystic. Imaging showed predominantly cystic large lesion 18.4 cm x 30 cm x 32 cm in abdominopelvic region with minimal thickened septae, probably serous/mucinous cystadenocarcinoma. On opening the abdomen with the midline vertical incision. The in situ thinned out peritoneum completely fused with the wall of the cyst all over and at some places the posterior rectus sheath, peritoneum and cyst wall fused completely and formed like one layer of the cyst wall. Decompression of the tumor was done by taking out the mucinous jelly like material of 10 liters drained. After reaching the peritoneal cavity, there was a huge tumour extended to all over the abdomen 60 cm x 40 cm x 35 cm. It is soft, cystic, yellowish tumour spreading all over. another extension of the tumour which is cystic mucinous tumour of size 25 cm x 30 cm x 28 cm from the left ovary adherent to the left ureter and below to urinary bladder. The tumor was surprisingly taken out successfully with The total weight of 20 kg. Total abdominal hysterectomy with right sided salpingo-oophorectomy with removal of huge ovarian tumour done [6].
A rare case of a 75 years female postmenopausal multiparous women with a massive third degree uterovaginal prolapse with painless lump in abdomen. The mass was corresponding to 36 weeks size of uterus, hard, irregular, immobile, non-tender felt with ascites. Her tumor markers were normal with mildly raised CA125. Ultrasound showed (Abdomen + Pelvis) and Contrast Enhanced Computed Tomography s/o The cystic mass with multiple septae in lower abdomen is of size 21.1 cm x 14.5 cm x 11.6 cm. Exploratory laparotomy with excision of large ovarian tumour with frozen section followed by total abdominal hysterectomy with removal of other side Fallopian tubes were done. Intraoperative in situ findings were suggestive of a mass arising from ovaries 26 cm x 25 cm x 24 cm in size - irregular surface, solid cystic with increased vascularity. While operating on such tumours care has to be taken to manage these complications as well as the problems associated with sudden decompensation of such large tumours [7].
The uniqueness of our case lies in that Ovarian cysts occur commonly in women of childbearing ages however can be rarely seen in elderly post-menopausal or post-hysterectomised patients as seen in our case. Pelvic examinations and imaging studies can be used to further diagnose symptomatic patients and aid physicians in developing an appropriate course of treatment. Tumor markers also play a crucial role in the management of ovarian tumours, particularly in ovarian cancer and hence should always be assessed in any suspected case. In our patient, CA125 and other tumor markers were all within normal limit which favoured the provisional diagnosis. Further the Frozen section Biopsy sent intraoperatively confirmed the nature of tumor to be Benign Ovarian Mucinous Cystadenoma.
Mucinous tumours of the ovary represent a spectrum of neoplastic disorders which includes benign mucinous cystadenoma, pseudomyxoma peritonei, mucinous tumours of low malignant potential (borderline), and invasive mucinous ovarian carcinoma. These tumours are related closely to each other and are distinct from other histologic subtypes of epithelial ovarian neoplasms from a clinical, histologic, and molecular standpoint. A continuum appears to be present from benign to borderline to malignant, which is different from other types of epithelial ovarian cancer. Mucinous cystadenomas usually occur as a large, multiloculated cystic mass with mucus-containing fluid [8].
When determining the primary or metastatic nature of the mucinous neoplasm, size and laterality can suggest the tumour origin, as primary tumours tend to be larger and unilateral as confirmed in our patient as compared to metastatic lesions. The mean size of primary Mucinous Ovarian carcinoma has been documented as 16-20 cm (range, 5-48 cm), compared with 11-12 cm (range, 2-24 cm) for metastatic cancers. The size of the tumor in our patient when correlated with age and post hysterectomy status raised high suspicion of malignancy in contrast to the level of tumor markers and imaging findings. However, this is not pathognomonic, as 32-48% of metastatic tumours are over 10 cm [9].
According to the literature, The gold standard for the treatment of any suspected ovarian mass includes intact removal of the involved adnexa with intraoperative pathology evaluation as was done in our patient [10-12]. This has historically implied laparotomy, total hysterectomy, bilateral salpingo-oophorectomy, and staging procedure including lymphadenectomy as per the extension of the tumor. There are many nuances to the appropriate surgical management of the patient with a mucinous ovarian tumour, and complete tracing of large and small intestines should always be performed in suspected primary ovarian carcinomas, as primary tumours are relatively rare [12]. Hence Every patient with either borderline or invasive components identified, should undergo a staging procedure to exclude the possibility of occult extra ovarian disease, as this would change the prognosis and recommended adjuvant therapy. Staging in patients with mucinous tumours includes a thorough evaluation of the peritoneal cavity with a sampling of any suspicious areas, pelvic washings, peritoneal biopsies, and infracolic omentectomy [12]. However When the surgeon enters the abdomen, care should be taken to remove the involved ovary intact without spillage of the mucinous contents, as rupture of a stage I Ovarian carcinomas may increase its potential for recurrence [13]. In light of this, Our patient was carefully managed surgically by exploratory laparotomy with left Ovarectomy and right-sided saplingoopherectomy along with thorough evaluation of other intraabdominal visceras including peritoneum and appendix to look for suspicious of any other primary origin of the tumour. Benign ovarian cystadenomas are by definition confined to the ovary. While appendicectomy was previously performed for any ovarian tumour with mucinous histology, including benign lesions, current data support not performing an appendectomy as long as the appendix appears normal and there is no evidence of pseudomyxoma peritonei as followed in our case after the frozen section biopsy report confirmed the diagnosis as benign mucinous cystadenoma of ovary [13].
The novelty of the discussed case here is the post-hysterectomised status of the patient. Ovarian tumours can occasionally be diagnosed after a hysterectomy, particularly if the ovaries were not removed during the procedure. Of women aged 50-54 years who underwent a hysterectomy, 78% of them also had a synchronous bilateral salpingo-oophorectomy (BSO). The decision for women to undergo a bilateral salpingo-oophorectomy during a hysterectomy is particularly difficult in light of the data from the Women’s Health Initiative randomized trials demonstrating more harm than benefit associated with postmenopausal hormone therapy [14]. The decision to undergo an elective bilateral salpingo-oophorectomy during a hysterectomy is even more challenging since women are more averse to taking hormone replacement [15,16]. A prospective cohort study showed that although bilateral salpingo-oophorectomy at the time of hysterectomy for benign disease is associated with a decreased risk of ovarian cancer, however, there is an increased risk of all-cause mortality associated with other health conditions such as coronary heart disease [17]. The results suggested that ovarian conservation until at least age 65 benefits long-term survival for women at average risk of ovarian cancer [18]. Prophylactic salpingo-oophorectomy after completion of childbearing in women with BRCA1/2 mutations can significantly decrease the risk of ovarian cancer. However, the benefit associated with removing one or both ovaries in low-risk populations remains unclear.
A spectrum of sequelae follows the Hysterectomy. The sequel Residual Ovarian Syndrome (ROS) occurs when the ovaries are left in place during a hysterectomy and later causes pelvic pain, a pelvic mass, or dyspareunia. This is in contrast to the ovarian remnant syndrome, in which a patient undergoes bilateral salpingo-oophorectomy, leaving a remnant of ovarian tissue. The incidence of Residual Ovarian Syndrome is 2-3% and the symptoms usually include chronic pelvic pain (71-77%), an asymptomatic pelvic mass (14-25%), or dyspareunia (67%). Malignant neoplastic change takes place in the residual ovary in 0.26-12.3% of cases, however, one must keep in mind the advanced age and further clinical and histopathological correlation to rule out the malignancy. The majority of women in the general population are at average risk of ovarian and breast cancer, however, the risks associated with bilateral oophorectomy before age 50 far outweigh the benefits. They must be informed about the complex risk-benefit ratio of the surgery. Oophorectomy performed after age 50 and up to age 65 may still have deleterious effects, but the risk-benefit ratio seems to be less dramatic.
In conclusion, this case report highlights the rare occurrence of an ovarian mucinous cystadenoma in a post-hysterectomy female, underscoring the importance of continued surveillance for ovarian pathology even after a hysterectomy. While the hysterectomy typically reduces the risk of gynaecological malignancies, it does not eliminate the possibility of ovarian pathology. This case serves as a reminder that residual ovarian tissue can still be a site for benign and malignant tumours, necessitating careful monitoring of patients who undergo hysterectomy. The presence of an ovarian tumour in this context may raise concerns for malignancy; however, thorough imaging and histopathological evaluation confirmed the benign nature of the cystadenoma. Overall, this case contributes to the growing body of literature emphasizing the need for vigilance in monitoring ovarian health in post-hysterectomy women and highlights the significance of interdisciplinary collaboration in managing such cases effectively.
Copyright: © 2025 Rajshree D Katke., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.