Nadeem Niyaz Jan*
Department of Vascular Surgery, Varicose and More PVT LTD, India
*Corresponding Author: Nadeem Niyaz Jan, Department of Vascular Surgery, Varicose and More PVT LTD, India.
Received: July 15, 2024; Published: July 28, 2024
Citation: Nadeem Niyaz Jan. “Dilated Arteries (Aneurysms)". Acta Scientific Paediatrics 7.8 (2024): 09-12.
An aneurysm is an abnormal widening or ballooning of a portion of the artery due to weakness in its wall.
It is not clear what causes aneurysms. Some are present at birth (congenital). Defects in some parts of the arterial wall may be responsible.
Common locations for aneurysms are:
High blood pressure, high cholesterol, cigarette smoking raise risk of you having an aneurysm. High blood pressure plays a role in abdominal aortic aneurysms. Atherosclerosis may also be responsible. Pregnancy is often linked to formation and rupture of splenic artery aneurysm.
Copper deficiency affects the elastin tissue strength. The lysyl oxidase that cross links connective tissue is secreted normally but with reduced activity. People who die of aneurysms have liver content of copper 26% of normal. The median layer of blood vessel containing elastin is thinner but the copper content of elastin is the same as or normal people. Aneurysms are relatively rare is women because oestrogen increases the efficiency of copper absorption. Alcohol increases copper uptake while alcohol in diabetics reduces iron, zinc and copper uptake. Those who handle iron have a 100% reduction in copper. Excessive zinc can reduce copper levels by reducing absorption of copper from the gut.
Local hemodynamic factors are responsible for damage to the arterial segment. Aorta is a low resistance circuit for circulating blood while lower extremity is a high resistance circuit. Repeated trauma of the reflected arterial wave on distal aorta may injure the weakened distal aortic wall leading to aneurysmal formation. Systemic hypertension compounds the injury. Thus aneurysm formation is multifactorial. Increasing aneurismal dilatation leads to increased arterial wall tension and stress. According to Laplace’s law increase in diameter increases the wall tension which in turn increases the wall diameter and promotes risk of wall rupture. The arterial wall supplied by blood from its vasa vasorum. Thus in a developing aneurysm the most ischemic portion is at the farthest end. This aids in weakening the wall and causing further expansion. Thus eventually all aneurysms will if left to complete their evolution rupture without intervention.
They are either true or false.
True aneurysm involves all 3 layers of the arterial wall – adventitia, media and interna. True aneurysms are atherosclerotic, syphilitic, congenital or vertricular following transmural myocardial infarctions.
False aneurysms are pseudoaneurysms which do not involve the arterial wall. The leaking blood is confined by the surrounding tissue. This blood filled either thromboses to seal the leak or flow out into the surrounding tissue. These are caused by trauma that punctures the artery as percutaneous puncture of the artery as in angiography, arterial grafting or puncturing the artery as by drug pushers. They may present as a pulsatile mass on palpation.
They are classified according to their macroscopic shape and size as saccular or fusiform.
Saccular aneurysms are spherical in shape and involve a portion of the arterial wall. They are 5-20 cm in diameter and filled partially or completely with thrombus. Fusiform aneurysms are spindle shaped and extend up to 20 cm in length. They are present in the ascending, arch and descending aorta involving iliac arteries.
Classification due to location
Arterial aneurysms are common but venous aneurysms do occur as popliteal venous aneurysm.
Classification according to underlying condition
These depend on the location of the aneurysm. If present near the body surface, pain and swelling with a throbbing mass are seen. However aneurysms within the body or the brain are asymptomatic. If an aneurysm ruptures, pain, low blood pressure, rapid heart rate and light headedness may occur. The risk of death after a rupture is very high.
These occur when the aneurysm pushes on the surrounding brain structures. The symptoms of a ruptured aneurysm are different from a non-ruptured one. In the latter case they are:
In case of ruptured cerebral aneurysm:
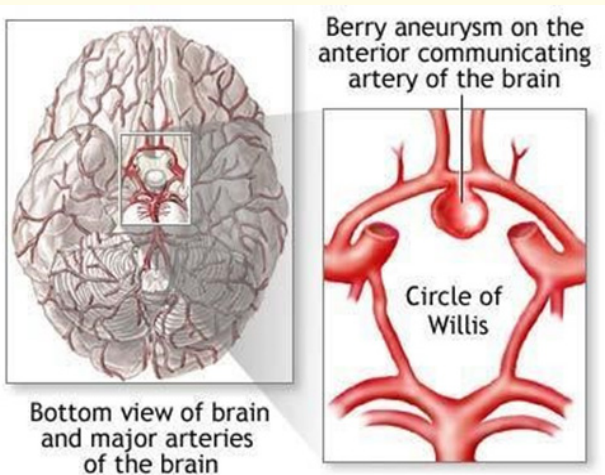
Figure 1
Physical examination is a must. The tests include.
CT scan
Diagnosis of cerebral aneurysm
Surgery is mostly recommended. The type of surgery needed depends on symptoms and type of aneurysm. Some have an endovascular stent repair which is a tiny tube used to prop open a vessel and reinforce its weak wall. No major cut is needed and so recovery is faster. With successful surgical repair the outlook (prognosis) is excellent.
This is either surgical intervention of watching and waiting along with control of blood pressure. Endovascular treatment includes clipping or endovascular coiling. In clipping of the aneurysm a craniotomy exposes the aneurysm and a clip is applied to the base of the aneurysm. This is the best method to permanently eliminate aneurysms. In endovascular coiling. The catheter is passed from the femoral artery via the aorta into the carotids and then the brain arteries reaching the aneurysm. The coils are released into the aneurysm. These coils start a thrombotic reaction within the aneurysm and eliminate it. In broad based aneurysms a covered stent is passed to occlude the neck of the aneurysm. Comparing clipping versus coiling, the latter has shown a 7% reduced mortality rate compared to clipping. However coiling is associated with a higher recurrence rate, almost 30% and increases over time. The patients with endovascular coiling must have annual investigations to look for early recurrence and treated with further coiling or surgery if recurrence is detected.
In these the weakened segment of the arterial wall is replaced by bypass graft. Endovascular stenting is a less traumatic option where a covered stent is placed across the aneurismal artery.
Compression of the adjoining structures mainly nerves giving rise to weakness of the extremity and numbness. This is more common in popliteal artery aneurysms behind the knee.
Infection may lead to body-wide illness (sepsis) and rupture.
Rupture can lead to massive bleeding and death – commonly seen in abdominal aortic aneurysms, mesenteric artery aneurysms, splenic artery aneurysms. Rupture of brain aneurysms leads to stroke, disability and death.
See a doctor if you develop a lump on the body even if it is not painful and throbbing.
Blood pressure control may help prevent some aneurysms. Healthy diet, regular exercise and keeping cholesterol under check helps prevent aneurysms and their complications. Stop smoking to lower the risk.
This is the large blood vessel that supplies blood to the pelvis and legs, balloons outwards.
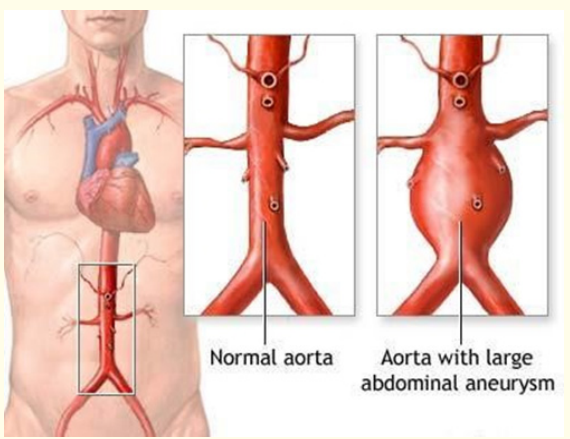
Figure 2
AAA develop slowly over years with no symptoms. If it develops rapidly and breaks open (rupture) or leaks along the wall (dissection) then symptoms develop rapidly. If rupture occurs then: there is severe, sudden, persistent pain in the abdomen or back radiating to the groin buttock or legs.
Evaluation of the abdomen along with the pulses and sensation in the legs. There may be an pulsating abdominal mass, stiff and rigid abdomen.
If there is bleeding from aortic aneurysm then open repair will have to be done.
Asymptomatic aneurysms that are small are generally left alone. Yearly ultrasound is done to see if the aneurysm is becoming bigger. Surgery is recommended for those whose aneurysm is growing over 1 cm / annum or is 5.5 cm on presentation.
There are 2 approaches to surgery:
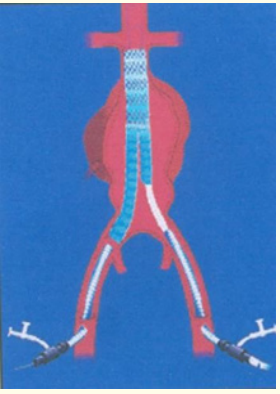
Figure 3: Diagrammatic representation of endovascular graft in AAA.
It is good in experienced hands and < 40% survives a ruptured aneurysm.
Ruptured aneurism is an emergency. Dissection is when the innermost lining of the artery tears and blood leaks within the wall.
Go to the casualty if belly or back ache does not go away or is unbearable.
To reduce the risk of developing aneurysm:
These include diabetes, hypertension, obesity, tobacco use, alcoholism, high cholesterol, copper deficiency and advancing age.
Copyright: © 2024 Nadeem Niyaz Jan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.