Sunita Singh*
Department of Paediatric Surgery, All India Institute of Medical Sciences, Raebareli, U.P., India
*Corresponding Author: Sunita Singh, Department of Paediatric Surgery, All India Institute of Medical Sciences, Raebareli, U.P., India.
Received: June 03, 2024; Published: June 28, 2024
Citation: Sunita Singh. “Acute Colonic Obstruction Due to Rare Pharmacobezoar (Chalkolith) in an Adolescent Girl: An Unusual Complication of Pica”. Acta Scientific Paediatrics 7.7 (2024): 10-13.
The compulsive eating of non-food items can lead to many complications. The undigested or poorly digested non-food items can form various types of bezoars. These bezoars usually presents with features of upper gastrointestinal obstruction. We discussed a rare case of distal colonic obstruction in a child by rectal impaction of phramocobezoare. The child was successfully managed without laparotomy.
Keywords: Bezoars; Chalkolith; Children; Colonic Bezoar; Colonic Obstruction; Geophagy; Geophagia; Pica; Paediatric Colonic Obstruction; Pharmacobezoar.
Pica refers to the problematic, unsocial, and compulsive consumption of non-nutritive non-food substances [1]. The non-food items could be soap, plaster, paints, buttons, clay, cigarette buds, pencil chewing, chalk, paper, gum, coal, soil, earthen pots, laundry starch, ice, chalk, etc. Pica is commonly observed in pregnancies, biomedical disorders (anemia and sickle cell disease), cases of lead poisoning, and nutritional deficiencies (Iron and zinc deficiency) [2,3]. Pica is considered a mental disorder according to DSM-V (Diagnostic and Statistical Manual of Mental Disorders) [4,5]. The risks of pica vary from mild and transient habits to life-threatening medical issues such as infections, poisoning, choking, gastrointestinal problems require life-threatening surgeries [6].
Gastrointestinal bezoars are aggregates of inedible or undigested material found in the GI tract. The types of bezoars can be Trichobezoar (hair and food particles), Lactobezoar (milk protein), Pharmacobezoar (concretions of cholestyramine, kayexalate resin, cavafate, calcium coarbonate, and antacids), Phytobezoar (indigestible food particles). The bezoares usually cause upper gastrointestinal obstruction. Distal colonic obstruction is very rare due to bezoars [8-11]. We discussed a rare pharmacobezoar (Chalkolith) causing distal colonic obstruction in a child.
A 13-year-old female presented with acute intestinal obstruction for 5 days. The girl was the youngest among 5 siblings. According to the Modified Kuppuswami classification, her parents belongs to low socioeconomic status. She was of average intelligence but neglected in the family. At the time of presentation, her vitals were stable. Per-abdomen examination showed minimal abdominal distension with minimal diffuse tenderness, but there were no guarding or rigidity. A few intraabdominal hard mobile lumps were palpable at the left paraumbilical region.
Digital rectal examination wasn’t possible because of the stony hard intraluminal impacted mass in the rectum. X-ray erect abdomen showed showing dilated air-filled colonic loops with a huge opacified mass occupying the rectal lumen extending up to the sigmoid colon (Figure 1). USG Showed a hyperechoic mass in the pelvis with gaseous distension of bowel. Blood biochemistry revealed Iron Deficiency anemia. Hemoglobin was 8.4 gm/dl, serum ferritin was 8 gm./ml, and serum calcium was 8.3 ng/dl.
On inquiry, the girl came out with a history of compulsive eating of chalk (calcium carbonate) used for writing on the blackboard in schools. There was no clinical feature of hypercalcemia (confusion, delusion, headache, vomiting, etc.).
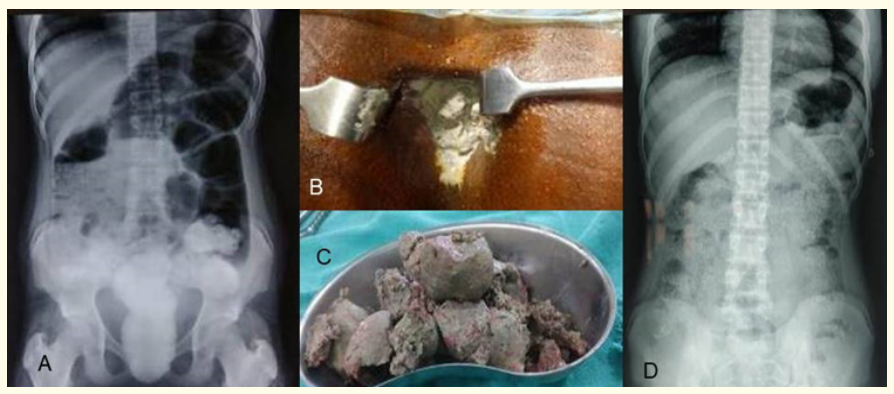
Figure 1: (A) Plain X-ray of the erect abdomen showing dilated air-filled colonic loops with a huge opacified mass occupying the rectal lumen extending up to the sigmoid colon. (B) Chalkolith visible through the anal orifice; (C): Chalkolith evacuated per rectally, (D) Follow-up X-ray abdomen erect showing persistent diffuse punctate calcification in the colonic wall.
Under spinal anesthesia rectal examination was done. A white chalkolith was visualized through anal orifice (Figure 1). The bezoar was stony hard and tightly impacted into the rectum. The bezoar (chalkolith) was extended from anal verge to beyond the fingertip. The Chalkolith was evacuated with difficulty (needed instrumentation) in piecemeal through the rectum. Intraoperative rectal wash was given with warm saline. The child was allowed orally on next day. Oral Polyethylene-glycol was administered twice a day for three days, followed by once a day for two weeks (to wash out the remnants from the colon). The perioperative period was uneventful.
The follow-up abdominal X-rays after seven days and one month were suggestive of persistent diffuse, punctuate calcification within the limits of the colon termed by the author as a persistent snowstorm appearance. The explanation regarding persistent calcification could not be explained.
The nutritional supplements were administered in a follow-up of one year. Further, the patients with her parents were in regular follow-ups for counseling to psychiatrist and social workers.
‘Geophagy’ or ‘geophagia’ is the habit of consuming clay soil such as chalk (calcium carbonate or calcite) or kaolin (clay) [7]. A bezoar is a solid mass formed in the gastrointestinal tract as a result of the consumption of indigestible or poorly digestible substances. Bezoars most commonly form in the stomach, but can occur in the small intestine and, rarely, in the colon or rectum.
The pathophysiology of pica or Geophagy is completely not understood. The pica is usually associated with Iron, Zinc, and Calcium deficiency. The compulsive unusual eating of non-food items leads to the deficiency of minerals and iron in the body. The ingested starch and clay bind with iron and calcium leading to deficiency of minerals in the body [3,7].
Another proposed theory was chronic lead poisoning because of the consumption of lead-based paints (used in old houses) or licking of lead-based-paint coated toys. Consequently, based paint was banned in 1978. We couldn’t measure the serum lead levels because of the unavailability of the procedure [4].
The habit of pica is usually seen in pregnant women, anemic children, mentally retarded oand depressed individuals. In children, some unusual behaviours like abnormal language, strange methods of play, and strange relationships with friends of their age group can also be found. A paediatric psychologist should be involved in counseling of such parents [5].
The usual complications of pica are malnutrition, intestinal obstruction, intestinal infections, parasitic infestation from the soil, anemia, mercury poisoning, lead poisoning, progressive liver and renal damage with constipation, and abdominal problems [6].
There can be pica-related deaths due to acute choking during ingestion or complications related to surgeries done for perforation peritonitis, and enteostomies done for persistent sepsis [5]. Obstructions of the gastrointestinal tract caused by bezoars are about 0.4-4% of the total obstructions and mainly occur in the stomach or small intestine [8]. The occurrence of colonic obstructions caused by bezoars is considered pretty rare. Contrary to other bezoar chalkolith leads to distal colonic obstruction. Colonic bezoar is a rare and difficult diagnosis as a cause of intestinal obstruction. The colonic bezoars have been reported in elder age groups with risk factors of gastro motility impairment, past gastrointestinal surgery, diabetes mellitus, muscular atrophy, and cerebrovascular disease [9].
Abdominal computed tomography can discriminate not only bezoars but also other potential causes of gastrointestinal tract obstructions such as gastrointestinal malignancies. The CT has higher sensitivity and specificity in diagnosing gastrointestinal obstructions compared to other tests. The CT must be considered for the diagnosis of intestinal bezoars [8,9]. In our case, the cause of obstruction was evident by history and per rectal examination, so a CT scan was not done to avoid radiation exposure to the child.
If patients are clinically stable, distal rectal obstruction due to bezoars can be managed by manual evacuation and bowel washing [8]. A colonoscopy is recommended to ensure complete evacuation. However, the author could not do it because of the unavailability.
Complicated colonic bezoars such as strangulated intestinal obstruction, massive melena, or perforation peritonitis warrant the administration of broad-spectrum antibiotics fluids and electrolyte correction and early surgery [8,9].
Regular post-operative Psychiatric follow-up, counselling, motivation and treatment of Iron deficiency anemia are necessary to prevent reoccurrence of bezoar [2,4].
Among the causes of colonic obstruction, bezoar can be difficult to diagnose because they are very rare. This case was a unique case of distal colonic obstruction as a manifestation of geophagy and the first of its type. Conservative approaches such as the use of enemas and manual disimpaction can be considered in uncomplicated cases of colonic bezoars.
None to declare.
None.
46th Annual Conferences of Indian Association of Paediatric Surgeons, 2022 (virtual conference).
Copyright: © 2024 Sunita Singh. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.