Omar Mohamed Mohamed Kasem1, Mohamed Ibrahim Elsawaf2*, Hamed Mahmoud Seleim3, Khaled Mohamed Elshimy4
1MSC of general surgery, Faculty of Medicin, Tanta University, Egypt
2Professor of Pediatric Surgery, General Surgery Department, Faculty of Medicine, Tanta University, Egypt
3Assistant Professor of Pediatric Surgery, General Surgery Department, Faculty of Medicine, Tanta University, Egypt
4Assistant Professor of Pediatric Surgery, General Surgery Department, Faculty of Medicine, Tanta University, Egypt
*Corresponding Author: Mohamed Ibrahim Elsawaf, Professor of Pediatric Surgery, General Surgery Department, Faculty of Medicine, Tanta University, Egypt. Email: mohamed.elsawaf@med.tanta.edu.eg
Received: February 12, 2024; Published: March 10, 2024
Citation: Mohamed Ibrahim Elsawaf., et al. “Needlescopic Traction (Shehata technique) for Impalpable Undescended Testes: New Era”. Acta Scientific Paediatrics 7.4 (2024): 13-19.
Background: Several techniques were recorded in treating intra-abdominal testis including vessel intact laparoscopic orchidopexy (VILO), microsurgical auto-transplantation, one/two stage open/laparoscopic Fowler-Stephens orchidopexy, and staged laparoscopic traction orchidopexy (Shehata technique). Needlescopic surgery is a recent innovation aiming at scarless surgery, providing safty, efficacy in several pediatric laparoscopic procedures as appendectomy, hernia, and cholecystectomy.
Aim of the work: Evaluating safety, feasibility, and efficacy of needlescopic approach for traction-lengthening treatment of intraabdominal testes.
Patients and methods: This study was carried out in Pediatric Surgery Unit, Tanta University Hospitals, from September 2021 to September 2022, on 53 boys with unilateral impalpable testes. laparoscopic exploration was done for all cases, if testes were intraabdominally, with long testicular vessels decision was taken to do one stage VILO and in case of short vessels needlescopic Shehata technique was then attempted.
Results: Out of 53 testes, 23 testes were vanishing, 5 cases with long vessels enough to undergo one stage VILO, and 25 cases with short testicular vessels underwent Shehata technique using special type of needles. All cases were completed needlescopically, no conversion, nor intra-operative complications were encountered. Three months postoperative follow up showed that testicular size was comparable clinically with normal contralateral one, and it was normal in 24 (96%) while 1 testis was smaller compared to the contralateral side in 4 year old boy and the difference was statistically insignificant (P value was 0.28).
Conclusion: Shehata technique is an excellent option for cases with intra-abdominal testis with short vessels that can gain length by gradual controlled traction, thus can be transposed easily down into the scrotum without tension. Adding needloscopic assistance to shehata technique is a new, and promising technique. Almost non-visible scars were recorded and all parents reported excellent cosmetic results.
Keywords: Impalpable Testis; Staged Traction; Needlescopic Surgery
The testes complete their descent in the third trimester of pregnancy. At birth, incidence of UDT in full-term males is 3-5%; at the age of 3 months drops to 1-2% [1]. Diagnosis of UDT can be done using Ultrasound, MRI or CT, but all are not reliable [2,3]. Nowadays diagnostic laparoscopy is the gold standard for the diagnosis of impalpable UDT [4]. Many techniques were introduced for treatment including (VILO), microsurgical auto-transplantation, Fowler-Stephens techniques, and staged laparoscopic traction orchiopexy (Shehata technique) [6,7]. Needlescopic surgery is a recent innovation aiming at scarless surgery, providing safty, efficacy in several pediatric laparoscopic procedures as appendectomy, hernia, and cholecystectomy [8-10].
To evaluate the safety, feasibility and efficacy of needlescopic approach for traction-lengthening of intraabdominal testes.
Study design was a prospective, single-arm, open-label trial carried out through needlescopic approach using Mediflex needle® and custom-made micro-cautery probe to conduct the staged laparoscopic traction-orchiopexy (Shehata technique) for intraabdominal testes from September 2021 to September 2022.
This study was approved by the Ethics Committee of the Faculty of Medicine, Tanta University, Egypt. Registration NO: 34934/9/21. An informed consent was collected from parents of all gaurdians’/ parents before participation in the study.
All patients with impalpable UDT aged from 6 months to 4 years old were included. While patients with previous abdominal operations, bilateral intra-abdominal testes, and patients with Sub-renal IAT were excluded.
We used a 5-mm trocar for a 30° telescope, a Suture Grasper Device (SGD) [Mediflex Company, 250 Gibbs Road, Islandia, New York 11749, USA] (Figure 1), and a long isolated custom-made diathermy probe (DP) connected to ordinary diathermy handle. The Diathermy Probe was made by thinning out of a Kirschner’s wire to 1.5 mm and isolated with shrinkable rubber tube.
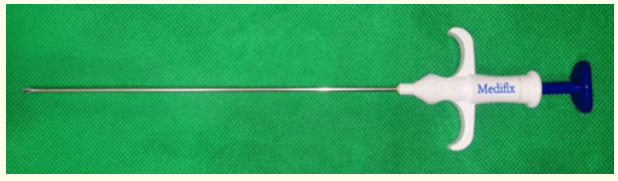
Figure 1: Mediflex Suture Grasper Device.
The child was placed supine at the right upper edge of the operating table. Anesthesia machine was put at the head of the patient to the left side. Operator stood on patient’s right hand in either right or left IAT. Camera man stood at table’s head with the monitor at the patient’s feet, and the scrub nurse stood to the left of the table (Figure 2).
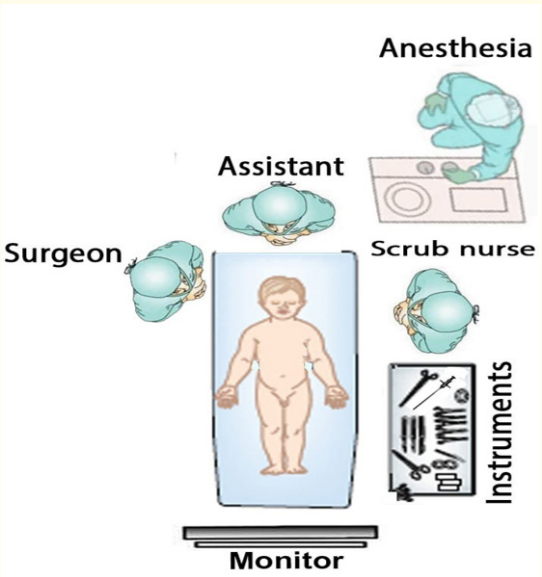
Figure 2: Figure showing the operative room layout.
Examination under general anesthesia was done to confirm impalpable testis and urinary catheter was inserted under complete aseptic condition to evacuate the bladder.
Point A: A vertical trans umbilical incision for insertion of 5-mm camera port then
Point B: A tiny puncture in the midline [midway between umbilicus and symphysis] for either insertion of Suture Grasper Device or Diathermy Probe according to the side of intra-abdominal testis [IAT], and
Point C: tiny puncture at the corresponding Mc-Burney’s point (point RC in right and point LC in left-sided IAT).

Figure 3: Site of port placement in impalpable UDT.
The operating table was put into Trendelenburg position and slightly tilted to the opposite side of the IAT. The peritoneal cavity is explored to confirm the diagnosis. The findings can be classified as: (a) blind ending vas and vessels with closed IIR, (b) vas and vessels passing through opened IIR, (C) peeping testis or (D) IAT found. Type C and D only will be included in our study. If the testes had long testicular vessels decision was taken to do one stage VILO and in cases of short vessels needlescopic Shehata technique was then attempted.
Suture Grasper Device was used to grasp and divide the gubernaculum under direct vision using the insulated custom-made diathermy probe (DP) with monopolar blended low cutting current away from the testis to avoid injury of the ‘long-looping vas’.
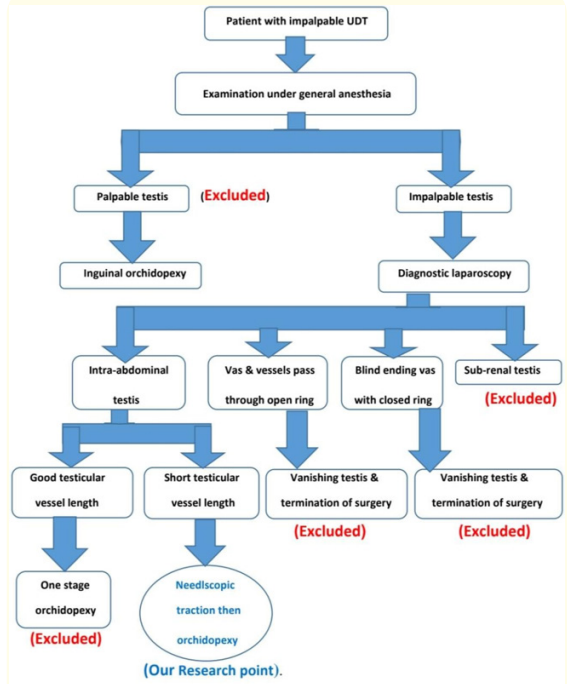
Figure 4: Figure showing our surgical flowchart of impalpable UDT.
The peritoneum lateral to the testicular vessels is incised and the testis mobilized by sharp dissection of the peritoneal covering keeping the triangular peritoneal covering between the vas and the testicular vessels. The testis was then fixed with a single stitch of silk or Ethibond™ 2/0 on round needle to the fixation point one inch above and medial to the contralateral anterior superior iliac spine (ASIS) (Figure 5).
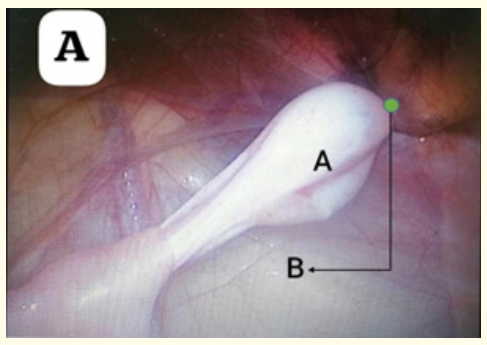
Figure 5: Showing Testis after fixation to the contralateral side.
The pneumoperitoneum is released, the port and instruments are removed. The umbilical wound is closed with absorbable sutures and the puncture sites with Steri-strips™. All boys are discharged home in the evening of operative day.
Traction interval of 6- 8 weeks was considered. Follow-up Doppler U/S scan was done in the last few days before the second stage to check for the position and viability of the testis-under-traction.
The abdominal cavity is inspected for any adhesive bands, slippage of the suture and retraction of the testis, and position of the intestine in relation to the testicular vessels (TV) are noted and recorded. The now-elongated TV are stretched to assess its lengthening. Then, the fixation stitch is divided and the testis is delivered through small scrotal incision using long artery forceps passing upwards through the inguinal canal and entering the peritoneal cavity medial to the inferior epigastric vessels before directing the testis to the scrotum to be fixed in a sub-dartos pouch. The boy is discharged home on the evening of the same day.
Follow up was done 3 months postoperatively to check testicular position and size compared to the other side by U/S, and colour Doppler. Parents’ satisfaction was asked for 3 months postoperatively during follow up visit.
A total of 53 boys with 53 impalpable undescended testes were managed at the pediatric surgery unit, general surgery department, Tanta University Hospitals during the period from October 2021 to September 2022. Out of which, 23 testes (43.4%) were vanishing, and 5 testes (9.4%) underwent conventional single stage vessel intact laparoscopic orchidopexy (VILO). Both were excluded from our study. A total of 25 patients (47.2%) underwent needlescopic staged traction orchidopexy. Right testis was absent in 14/25 cases (56%) and left one was absent 11/25 cases (44%).
Pre-operative ultrasonographic examination revealed intra abdominal testis in only 11 cases (44%), and the remaining 14 cases (56%) were absent. Volume of visualized testes (11 cases) ranged from 0.4 to 1 cc with a mean of 0.69 ± 0.31 cc, while the volume of the contralateral side (in the same 11cases) ranged between 0.5 and 1.3 cc with a mean of 0.854 ± 0.287. The intra-abdominal testis was smaller than the contralateral side but the difference is still non-significant (Table 1).
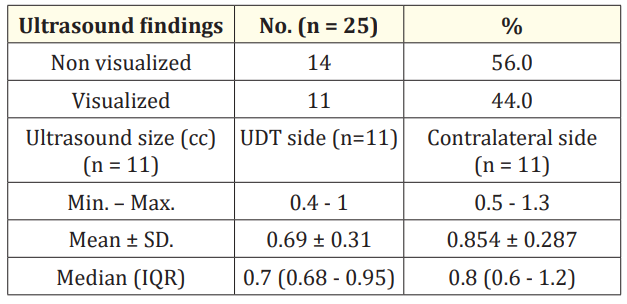
Table 1: Distribution of the studied cases according to pre-operative ultrasound findings.
Operative time was calculated in the second stage from skin incision to skin closure. It ranged from 40 to 52 minutes (Mean± SD was 45.21 ± 4.07 mins). No intra operative complications were encountered in the 2nd stages (No bleeding, no injury to vas, vessels or bowels). All cases were completed needlescopically with no conversion.
All patients started oral fluids 2-6 hours after the operation and tolerated full oral feeding within 8 -12 hours. All patients were discharged at the evening of the same day.
All data obtained after 3 months postoperatively and all patients were examined for:
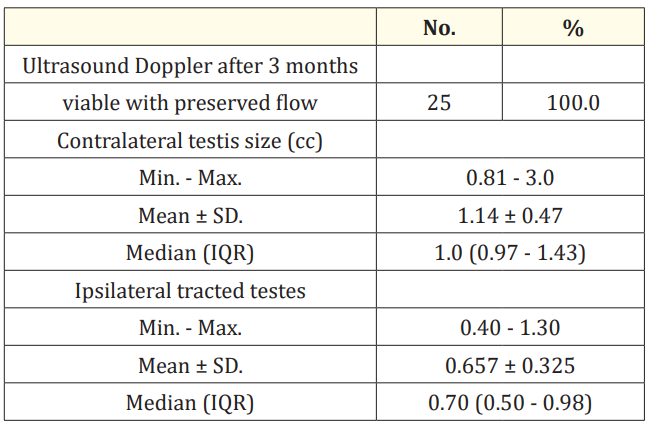
Table 2: Distribution of the studied cases according to post-operative US findings.
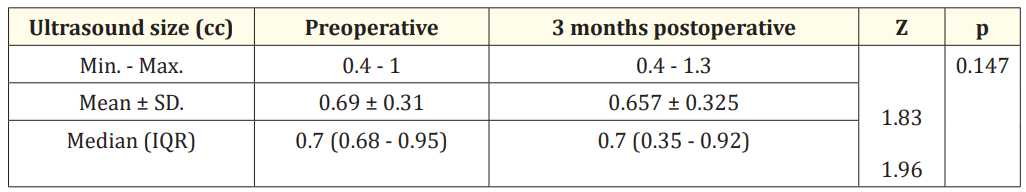
Table 3: Comparison between preoperative and 3 months postoperative in visualized cases by ultrasound (n = 11).

Table 4: Comparison between normal contralateral testes size and 3 months postoperative tracted testes (n = 25).

Figure 6: Follow up photos 3 months post-operative.
The term “needlescopic surgery” was coined by Gagner and Garcia-Ruiz in 1998 in which they described an operation that uses 3mm instruments. later, mini-laparoscopy term was introduced to describe minimally invasive surgery using instruments with a diameter of 3 mm or less [11,12].
Shehata recently reintroduced the concept of gradual traction in the management of high intra-abdominal testes in 2008, he proposed a new staged laparoscopic-assisted technique for bringing down the abdominal testis while minimizing complications and preserving viability [6].
Shehata technique effectively guaranteed the blood supply of the testis as; he preserved the main blood supply of the testis during the operation. The testis was fixed one inch above and medial to the contralateral anterior superior iliac spine (ASIS) during the first stage. The intestine pushes the TV downward to gradually extended with the help of maintained intestinal weight and continuous traction [13].
It is of course easy to explain as in this procedure testicular vessels were kept intact as compared to Fowler-Stephen’s procedure, and also limited or no dissection, skeletonization, and excessive stretch of the vas and vessels in VILO or open orchiopexy. Hence, testicular ischemia caused by extensive dissection, extra tension or ligation of the spermatic vessels was avoided, which is the most significant advantage of this technique. On the contrary, it is important to state that, neither we nor any publication along the years using traction technique reported testicular atrophy after 1st or 2nd stages [6,14,15].
There were almost nonvisible scars recorded in our study after 3 months and all parents reported excellent cosmetic results. As regard parents’ satisfaction (measuring location, size of the testis, and cosmesis after the surgery), 64% (16 cases) of parents reported excellent results, 24% (6 case) had very good results, 8% (2 cases) had good results, and only 1 case (4%) the parents reported poor outcome due to smaller size of the testis, the child was 4 years old.
Staged laparoscopic traction orchiopexy is an excellent option for cases with intra-abdominal testis with short testicular vessels. The testicular vessels gain length by gradual controlled traction on them, thus the testis can be transposed easily down into the scrotum without tension. Needlescopic traction for IAT have a promising potential with almost nonvisible scars and excellent cosmetic results.
This research was conducted without any outside funding or grants.
The authors of this paper have nothing to disclose.
Copyright: © 2024 Mohamed Ibrahim Elsawaf., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.