Di Nora A1, Scarlata F1, Di Mari A2, Pizzo F1, Palermo M2, Biasco A1, Distefano C1, Cacciaguerra G1* and Pavone P3
1Department of Clinical and Experimental Medicine, University of Catania Postgraduate Training Program in Pediatrics, Catania, Italy
2Radiology Unit 1, Department of Medical Surgical Sciences and Advanced Technologies "GF Ingrassia", University of Catania, Catania, Italy
3Section of Paediatrics and Child Neuropsychiatry, Department of Clinical and Experimental Medicine, University of Catania, Catania, Italy
*Corresponding Author: Cacciaguerra G, Department of Clinical and Experimental Medicine, University of Catania Postgraduate Training Program in Pediatrics, Catania, Italy.
Received: February 15, 2024; Published: February 27, 2024
Citation: Cacciaguerra G., et al. “Urosepsis as the First Presentation of Discopathy in an Adolescent with Occult Neurogenic Bladder ”. Acta Scientific Paediatrics 7.3 (2024): 53-55.
Urological complications are very common among patients with spinal cord injury, impacting meaningfully quality of life. While upper urinary tract dysfunction is less common, lower urinary tract dysfunction, such as “neurogenic bladder” is a common sequel of neurological diseases, due to morphofunctional alterations of the bladder sphincter complex. Herein we report the challenging case of a 15-years-old female with urosepsis secondary to neurogenic bladder in a disc disease.
Keywords: Urosepsis; Bladder; Neurogenic; Dysfunction
Urological complications are very common among patients with spinal cord injury, impacting meaningfully quality of life [1]. While upper urinary tract dysfunction is less common, lower urinary tract dysfunction, such as “neurogenic bladder” is a common sequel of neurological diseases, due to morphofunctional alterations of the bladder sphincter complex [2]. The alteration of the bladder–sphincter complex can be secondary to central or peripheral neurological lesions. Literature review reveals that approximately 40% of patients with lumbar disc disease have abnormal urodynamic testing, and an even larger proportion complain of voiding symptoms [3]. The most common urodynamic finding is detrusor areflexia, but underactive or overactive detrusor can also be observed. The control of micturition can be impaired by lumbar disc disease: the most frequently involved discs are L4/L5 and L5/ bladder innervation [3]. Patients with discal disease may have classical lower back pain, but not in every case. Herein we report the challenging case of a 15-years-old female with urosepsis secondary to neurogenic bladder in a disc disease.
A 15-years-old female presented to the emergency with three days of fever, vomiting and suprapubic and flank tenderness, without abdominal tenderness. The general conditions were unsatisfactory: on examination, the temperature was 39.6°C, the pulse 120 beats per minute, and the blood pressure 105/50 mm Hg. We performed three fluid bolus of saline solution (NaCl 0.9%) in twenty minutes, according with the Pediatric advanced life support (PALS) guidelines. Laboratory test revealed elevate acute-phase reactants and high white-cell count (20.500 per cubic millimetre). The serum creatinine concentration was 1.24 mg per decilitre (124 μmol per litre) and the most recent measurement 0.7 mg per decilitre (71 μmol per litre). Urinalysis was positive for leukocyte esterase and nitrites, with also bacteriuria with 10⁵ colony-forming units (CFU)/ mL. An abdomen ultrasound revealed the right kidney increased in volume, with multiple cortico-medullary areas of non-perfusion, some of which tending to abscess, report complaint with a right pyelonephritis. We started a general therapy with parenteral antibiotics with ceftriaxone and amikacin. Collecting the anamnesis of the patient, we discovered an history of urinary incontinence and enuresis for about one year, attributed by the family to a psychological disorder for the death of the grandmother. Thus, after the resolution of the infectious event, an urodynamic evaluations was performed revealing an overactive detrusor. Therefore, a spinal cord magnetic resonance imaging (MRI) was carried out that displayed a medial disc protrusion of L4-L5 with initial signs of intervertebral disc degeneration (Figure 1-2). So, the patients started therapy with oxybutynin, a drug that exerts direct antispasmodic effect on smooth muscle and inhibits the muscarinic action of acetylcholine on smooth muscle. It exhibits one-fifth of the anticholinergic activity of atropine on the rabbit detrusor muscle, but four to ten times the antispasmodic activity. No blocking effects occur at skeletal neuromuscular junctions or autonomic ganglia (antinicotinic effects). We discharged the patient with a 4-weeks treatment and with the recommendation to complete a voiding diary. At our next follow-up visitan improving of urinary incontinence and resolution of recurrent urinary tract infections was reported.
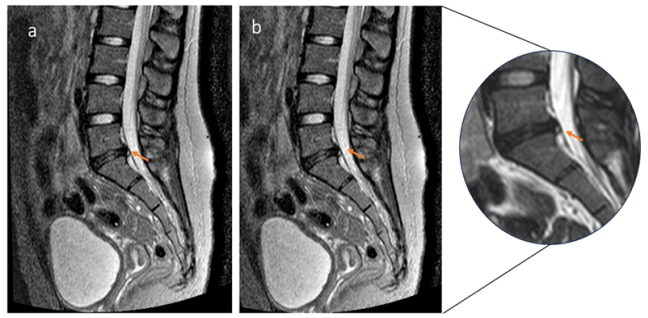
Figure 1: MRI of a 15 years-old girl with L4-L5 disc herniation and neurogenic bladder. Sagittal Short Tau Inversion Recovery (STIR) WI (a) and Sagittal T2WI (b) show posterior displacement of the L4–L5 disc (orange arrows). The height of the disc is reduced and there is focal hyperintensity within the posterior L4–L5 disc compatible with the annulus fibrous fissure (orange arrows).

Figure 2: Neurogenic bladder. Sagittal T2 WI shows atonic large bladder with focal wall thickenings that make it to assume a trabecular appearance.
Voiding is a coordinated process that engages distal sphincter relaxation, detrusor contraction and the opening of bladder neck, and this involves several nerves, originated from cauda equina. Neurogenic bladder is a common sequel of central or peripherical neurological lesions. A lumbar disc disease, in particular lesions that involved L4/L5 and L5/S1, such as herniation or protrusion, can damage bladder innervation and cause neurogenic overactivity in early stage, that lead in a late stage to underactivity and areflexia [2]. In neurogenic bladder peripheral nerves and bladder morphology can be modified, and this depending on disc disease extent and duration [3]. In fact, discal protrusion can damage nerve roots because compression interfering blood flow, as some studies have shown [4,5]. Overactive detrusor in an early stage of discal protrusion is an uncommon condition; in this case, bladder deformation could be represented by modest hypertrophy of detrusor, similar that in obstructive diseases [2].
The most common symptoms of disc diseases are back pain and leg or foot pain (sciatica), that can occur with or without back pain. In literature some cases of disc diseases without classic painful syndrome are reported [6,7]. Therefore, urodynamic evaluations of patients with lumbar disc disease reveal a prevalence of neurogenic bladder from 26% to 74% [8].
Disc disease is a rare, but possible, disorder in children, with about 5% of lumbar disc disease occurring in patients younger than 18 years of age [9]. The segmental distribution of disc herniation in children is like that seen in adults, the L4-to-L5 and L5-to-S1 disk herniations represent 50% of the total cases [10]. Like adults, paediatric patients who have symptomatic lumbar disc herniation commonly present with new-onset low back pain and lower extremity radiculopathy, but many patients may only have radicular symptoms [9]. Even if sports trauma are the most common causes of disc disease in paediatric age, physical loading, obesity, socioeconomic status, and genetic and behavioural influences may contribute to the onset of the disorder [11,12].
Neurogenic bladder is a possible sequel of disc disease because protrusion of the disc can cause degeneration of nerve roots and alteration of detrusor contractility. Even if low back and leg pain is common in disc diseases, the classic painful syndrome may lack. Disc diseases are rare but possible in paediatric age. In the case of our patient, the onset symptom was represented by the pyelonephritis, due to the overactive detrusor and an increased post-void residual volume. A correct clinical history has allowed us to suspect the diagnosis, then confirmed by apposite urodynamic evaluations.
The authors would like to thank AME (USA) Editor American manuscript Editors, for editing the manuscript.
The authors declare no conflict of interest.
Copyright: © 2024 Cacciaguerra G., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.