Agbeille MF1, Noudamadjo A1, Dansou JD1, Oke B2, Kpanidja MG1, Agossou J1 and Adedemy JD1
1Faculty of Medicine, Mother and Child Department, University of Parakou, Benin
2Department of Statistics and Epidemiological Surveillance of Borgou, Regional Health Directorate of Borgou, Benin
*Corresponding Author: Agbeille MF, Faculty of Medicine, Mother and Child Department, University of Parakou, Benin.
Received: January 30, 2024; Published: February 24, 2024
Citation: Agbeille M., et al. “Performance of the Prevention of Mother-to-Child Transmission of HIV in the Municipality of Parakou (Benin) in 2018”. Acta Scientific Paediatrics 7.3 (2024): 65-72.
Introduction: Mother-to-child transmission of HIV is currently inconceivable. The objective of this study was to evaluate the performance of the prevention of mother-to-child transmission of HIV in Parakou in 2015, in order to determine the factors associated with the quality of this strategy.
Patients and methods: This was a descriptive and analytical cross-sectional study ,conducted from May to July 2018. It focused on three groups of subjects: HIV-positive pregnant women seen for the first prenatal care in 2015, the children born to these pregnancies who integrated pediatric follow-up and PMTCT service providers. The indicators were calculated according to the Tanahashi model. The quality of PMTCT services was the dependent variable. The data collected were analyzed using Epi info version 7.2 software. The significance level retained was p < 0.05.
Results: The rate of HIV among pregnant women was 1.73%. The quality of PMTCT services was 28.96%. There were bottlenecks in all indicators of both supply and demand. The quality of PMTCT was significantly associated with the following factors: screening and early initiation of ARV therapy in pregnant women (p = 0.000), desire of HIV-infected women to become pregnant (p = 0.000), disclosure of HIV status to spouses (p = 0.000), knowledge of HIV-positive women about PMTCT (p = 0.000) and geographic access to pediatric services (p = 0.000). The residual rate of mother-to-child transmission was 6.25%.
Conclusion: The quality of PMTCT in the municipality of Parakou in 2015 is still low and all indicators don’t meet the standards. To improve the performance of this strategy, it is important to reorganize the management at all levels.
Keywords: PMTCT; Performance; Tanahashi; Benin
UNAIDS: United Nations AIDS Program; HIV: Human Immunodeficiency Virus; PMTCT: Prevention of Mother-to-Child Transmission; CHUD B/A: Regional Teaching Hospital of Borgou/Alibori; ANC: Antenatal Care
HIV infection is a major public health problem with a devastating effect on children [1]. According to UNAIDS, 1.8 million people infected worldwide were under the age of fifteen with 110,000 deaths in 2015. The heaviest price of this scourge is paid by children living in sub-Saharan Africa where 87% of deaths occur [2]. Vertical transmission is responsible for 90% of pediatric infections [3]. The prevention of mother-to-child transmission (PMTCT) is a strategy recommended by the World Health Organization (WHO) and recognized as one of the most effective in the fight against HIV/ AIDS. It has contributed to substantially reduce the rate of motherto-child transmission in several countries around the world. The elimination of mother-to-child transmission (EMTCT) is now the objective to be achieved, particularly in low-income countries [4,5]. This underpins greater mobilization of resources and political will from governments with more efficient health systems.
In Benin, the prevalence of HIV within the general population has been 1.2% since 2012 with a female predominance of infection [6]. The residual risk of mother-to-child transmission is currently 6.2% [7]. Benin is also committed to EMTCT. In the municipality of Parakou in the north of Benin, a study carried out in 2012 on the performance and factors associated with the quality of PMTCT services made it possible to evaluate the quality of PMTCT at 4.3% and to identify several bottlenecks [8]. This study was limited to the early diagnosis of children at 6 weeks of life without addressing the follow-up of the latter up to 18 months of life, the recommended time limit for determining the serological status of children in the context of PMTCT. As the current ambition of Benin is to achieve EMTCT, the question of the performance of PMTCT remains unresolved. The aim of this work was to evaluate the performance of this strategy in the municipality of Parakouin order to improve the management of children exposed to HIV.
This was a descriptive and analytical cross-sectional study which took place from May to July 2018 and focused on three groups of subjects
Subjects meeting the following criteria were included in each group:
Subjects meeting the following criteria were excluded from each group:
The dependent variable was the quality of PMTCT services. It was good when
The independent variables were of several orders: As for mothers, the variables were sociodemographic, biological and those relating to their knowledge and attitudes about HIV and PMTCT. Regarding infants, the variables were biological (PCR, HIV Serology). With regard to healthcare providers, they were socio-demographic, in relation to their seniority in the position and their knowledge of PMTCT. The other variables were linked to the availability of inputs for the diagnosis and the management of patients, the availability of human resources on PMTCT sites and geographic access to the different sites. The indicators were calculated according to the Takahashi model on which the national guidelines for monitoring and supervision of health facilities at the national level are based [9]. Thus, the indicators relating to the performance of PMTCT were of two types
We carried out an exhaustive recruitment of all HIV-positive pregnant women meeting our inclusion criteria and their children, as well as providers at the PMTCT sites. Attendance records at the workplaces of agents, PMTCT registers, stock sheets of inputs, medical records of mothers and infants were used for data collection. An interview with mothers as well as service providers was also carried out. At the end of the survey, the previously collected data were entered and then analyzed using Epidata 3.1 software and Epi Info version 3.5 software, respectively. Regarding the analysis of performance indicators, the standard for supply indicators was 100%. A difference of 5% between the lowest supply indicator and the 1st demand indicator constituted a bottleneck. The same applies for a difference of 5% between the 1st and 2nd indicator, as well as the 2nd and 3rd demand indicator. Factors associated with the quality of PMTCT were analyzed. The chi2 test was used to compare proportions and the difference was considered significant at p < 0.05. This study was conducted with strict respect for anonymity and the confidentiality of data was respected.
During the study period, 12,590 pregnant women were seen at the first antenatal care visit at the PMTCT sites of Parakou, 12,053 women were screened or 95.73%. Among them, 209 women were positive for HIV, i.e. a seropositivity rate of 1.73%. Out of the 209 HIV-positive pregnant women, 183 meeting our inclusion criteria were retained (Figure 1).
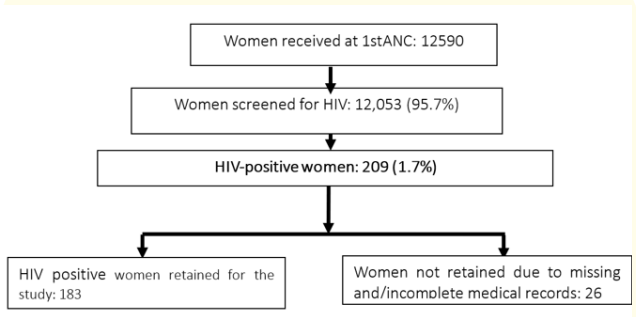
Figure 1: Flowchart of pregnant women screened at inclusion.
Regarding the children born to these mothers, 183 were born and retained for the study. Among them, 87 had joined the pediatric follow-up, or 47.54%. The children who had not joined the follow-up were 96, representing 52.4%. Among those who joined the follow-up, 17 were lost to follow-up (20.69%), including 13 after the age of 9 months (76.4%). Among these lost to follow-up, 7 were not found after the active search (41.2%). A total of 80 infants had a serology test at 18 months, including 75 seronegative (93.75%) and 5 seropositive, representing a rate of mother-to-child HIV transmission of 6.25% (Figure 2).
The average age of HIV-positive women was 26.7 years ± 4.3 years with the extremes of 19 and 42 years; those aged between 30 and 35 years were the most represented (39.3%). The mothers were traders in 36.6% of cases and housewives (24.6%); they were in a monogamous marriage (32.7%) and had no level of education in 45.4% of cases.

Figure 2: Flowchart of HIV-exposed infants included in the study.
Figure 3 illustrates the indicators of PMTCT performance in the municipality of Parakou according to the Tanahashi model.

Figure 3: Indicators of PMTCT performance in the municipality of Parakou according to the Tanahashi model.
All supply indicators were less than 100% and there was a difference of more than 5% between the lowest supply indicator (geographic access to pediatric departments 34.43%) and the first indicator of demand (use of PMTCT services, 74.86%). There was also a difference of more than 5% between the first indicator of demand (use of PMTCT services, 74.86%) and the second indicator (continuity of care, 59.01%) and between the second indicator and the third one (quality of care which is 28.96%).
Among the 183 women selected for the study, 124 were able to be interviewed. Regarding their knowledge, 95.16% of them knew the moments of HIV transmission from mother to child. Likewise, 52 women (41.94%) had good knowledge of the follow-up of children born to HIV-positive mothers. As for their attitude, 33.06% said they wanted the pregnancy, 33.87% said they had the first antenatal care (ANC) visit in the first trimester and 35.5% said they had the support of their spouses. Furthermore, 41 (33.06%) were using ARV before pregnancy and 17 of them said they did not want the pregnancy (41.46%). Among the 24 others who wanted their pregnancies, 5 (20.83%) had knowledge about safe conception measures without the risk of infecting their newborns and their sexual partner. In addition, 49 women (39.52%) among all those interviewed, claimed to have informed their spouses of their HIV status and the follow-up of children. For those who did not inform their spouses (60.48%), the reasons were as follows: fear of being rejected from the home (90.67%) and guilt (9.33%).
The health service providers had a mean age of 37.03 years ± 6.3 years with the extremes of 25 and 60 years. Midwives were the most represented (59.26%) followed by nurses (16.6%). They had seniority in the position of more than one year in 87% of cases and had received training on PMTCT in 88.9% of cases. In 90.74% of cases, the service providers had good knowledge of the follow-up of HIV-positive pregnant women and 61.11% had good knowledge of the follow-up of children born to HIV-positive mothers.
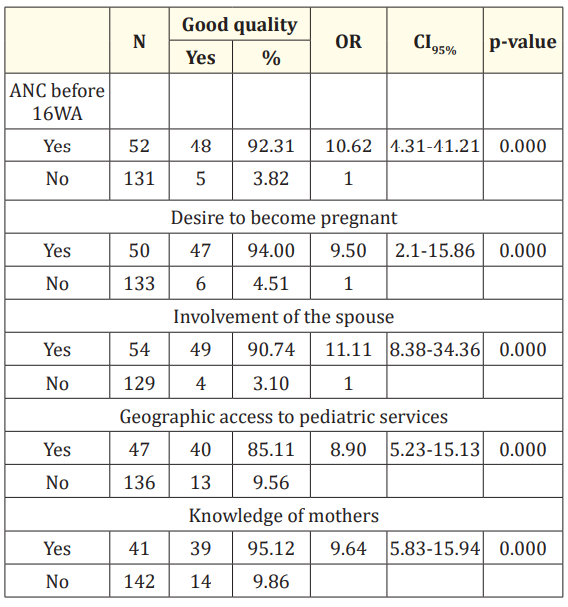
Table 1: Factors associated with good quality of PMTCT.
This was a descriptive and analytical cross-sectional study which focused on HIV-positive pregnant women and their children as well as service providers at the sites of PMTCT. Despite the retrospective nature of the study, the data collected was sufficient to ensure the reliability of the results. Recruitment was exhaustive,
which made it possible to reduce possible biases related to the selection of medical records. Our study took place in a municipality of Benin; the results cannot be generalized to a national health situation.
The rate of screening acceptance was 95.73% in the present study, similar to that of Manzi., et al. in 2015 in Nigeria [10]. Oke., et al. in 2012 reported a rate of 78% in the same municipality [8]. This demonstrates the progress made in access to screening among pregnant women. Indeed, the period between 2012 and 2015 coincided with the launch of EMTCT activities in Benin with the corollary of improving health coverage on the sites of PMTCT from 74.73% in 2012 to 96.2% in 2015 and therefore better access to these sites for pregnant women [8,11].
The rate of seropositivity in the present study was 1.73%. This rate is similar to that reported by Oke., et al. in 2012 which was 1.92%. The seropositivity rate of pregnant women in Borgou in 2015 was 1.86% [8,12]. In Sub-Saharan Africa, higher seropositivity rates were observed particularly in Burkina Faso in 2015 and Mali in 2011 with 4.86% and 2.27%, respectively [13,14]. The rate observed in our study corroborates national data, where HIV prevalence is 1.2% [6].
The rate of pediatric admission for the follow-up of PMTCT is 47.54%. Manzi., et al. in Nigeria [10] reported a lower rate of admission at 34%. On the other hand, Ouédraogo., et al. in Burkina Faso [13] reported a higher rate of pediatric admission at 92.5%. Less than one in two children had been followed up in our study. This could be explained by the low level of knowledge among HIVpositive mothers regarding the follow-up of children as noted in the current work since only 41.90% of mothers knew the importance of follow-up. But also, other factors such as non-disclosure of HIV status to the spouse or those around them. Likewise, for those who have joined the pediatric follow-up, it could be done clandestinely due to the non-disclosure of their serological status to their spouses. This follow-up is initially hidden by the routine Expanded Program on Immunization (EPI) which is commonly accepted by the spouse but after the last vaccination at 9 months of life, the follow-up stops, reflected in the high rate of loss to follow-up after this age. Beyond the screening of pregnant women, there is a need to make mothers more aware of the importance of follow-up until the age of 18 months.
The rate of mother-to-child transmission of HIV in our study was 6.25%, similar to the national rate of mother-to-child transmission of HIV in 2016 which was 6.2% [7]. Sangho., et al. in Mali in 2013 observed a higher rate of 7.3% [15]. InBorgou where the municipality of Parakou is located, the transmission rate in 2017 was 10.80% [16]. In Southern Africa, lower rates were observed varying between 2.7% and 1.1% [17,18]. In our context, the rate of vertical transmission is still high. It is certainly underestimated due to the high number of birth losses because more than half of children did not enter pediatric follow-up. Even if efforts have been made to increase the number of PMTCT sites and therefore improve the screening of pregnant women, the follow-up of children remains weak. As for mothers, decentralization of pediatric follow-up could help improve the access of children to PMTCT services. It is also important to take into account all other factors such as good information for mothers during pregnancy and support from spouses during the management to improve this indicator.
The quality of PMTCT was low in our study (28.96%). Oke., et al. had reported a lower quality of 4.30% in 2012 [8]. On the other hand, Sangho., et al. in Mali [15] observed a quality of 72.67%. Certainly, progress has been made to improve the quality of PMTCT services, but efforts still need to be made to achieve the objectives of EMTCT. All performance indicators did not meet standards. And there were bottlenecks in all indicators of both supply and demand. To achieve a good quality of PMTCT and secondarily ETME, all indicators must be improved from the availability of inputs and human resources to the access to PMTCT services, the use of ARVs and continuity of care. The strategies used do not seem to be sufficiently effective in improving the performance of PMTCT in the municipality and therefore deserve to be reviewed from top to bottom to be more efficient.
In the present study, several factors were significantly associated with the quality of PMTCT services. The first ANC visit before 16 weeks of amenorrhea (p = 0.000) is an example. Women who performed the first ANC before 16 weeks had a quality of PMTCT 10.62 times better than those who performed it later. This observation is corroborated by a study conducted by Oke in 2012 [8]. Early antiretroviral treatment in pregnant women increases the chances of birth without transmission of HIV to children. Likewise, the desire to procreate among HIV-positive women was also linked to the quality of PMTCT (p = 0.000). Women who wanted their pregnancies had a quality of PMTCT 9.50 times better than those who did not want it. A strong association is established between the desire to become pregnant in these women and better adherence to follow-up. The quality of PMTCT is therefore improved as noted by Iwelunmor., et al. in 2014 in Nigeria [19]. In our study, the question of sexual and reproductive health of women infected with HIV arises with possibly the unmet need for contraception among these HIV-positive women of childbearing age. Moreover, the lack of education on reproductive health without risk for people living with HIV, the lack of information and awareness among the population about HIV which should no longer be a taboo subject or a source of discrimination should be taken into account.
Furthermore, knowledge among HIV-positive women about PMTCT is essential. A significant association (p = 0.000) was identified between this factor and the quality of PMTCT. HIV-positive women with good knowledge of PMTCT had 9.5 times better quality than those who did not. A good understanding of PMTCT leads to better follow-up and improves the quality of services. In addition, good geographic access to pediatric services improves the quality of PMTCT. Children living less than 5km from the pediatric department had a quality of PMTCT 8.9 times better than those who did not. A similar observation was made in Malawi and Nigeria [20,21]. Hence the need to decentralize pediatric follow-up for better access of children to PMTCT. Finally, disclosure of the serological status to the spouse and his adherence to the approach improve the quality of PMTCT. It is 11.11 times better when the spouse adheres to the follow-up, similar to the findings made in Malawi [18].
The quality of PMTCT in the municipality of Parakou in 2015 is low at 28.96%. The rate of seropositivity among pregnant women is 1.73% and the residual rate of mother-to-child transmission of HIV is 6.2%. All PMTCT indicators don’t meet the standards with several bottlenecks. To improve PMTCT in the municipality, it is important to reorganize the management both at the community level and at the health facility level by improving the availability of inputs, human resources, but also geographic access, particularly to pediatric sites.
We would like to thank all the nursing staff at the PMTCT sites and the pregnant women who took part in the study.
None.
Copyright: © 2024 Agbeille MF., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.