Foli AGBEKO1,2*, Ounoo Elom TAKASSI1,3, Edem Koffi DJADOU1,4 and Yawo Dzayissè Atakouma1,3
1Department of Pediatrics, University of Lomé, Lomé, Togo
2Pediatrics wards, CHU Campus, Lomé, Togo
3Pediatrics wards, CHU Sylvanus Olympio, Lomé, Togo
4Pediatrics wards, CHR Tsevié, Tsévié, Togo
*Corresponding Author: Foli AGBEKO, Department of Pediatrics, University of Lomé, Lomé, Togo.
Received: February 05, 2024; Published: February 16, 2024
Citation: Foli AGBEKO., et al. “Malnutrition and Breastfeeding of Infants at 6 Months in Rural TOGO”. Acta Scientific Paediatrics 7.3 (2024): 06-10.
Introduction: Breastfeeding is the best way to provide ideal nutrition for ideal infant growth and development. The objective of the study was to determine the prevalence of malnutrition at 6 months according to the mode of feeding.
Patients and Method: This was a multicenter cross-sectional study that took place from January to July, 2021, in 6 health centers.
Results: A total of 353 mother-child pairs participated in the survey. The sex ratio of children was 1.15 with 54% being boys. The overall prevalence of malnutrition was 48.4%, including 3.12% obesity and 5.38% wasting. Wasting was present in 10.4% of infants who were not exclusively breastfed. Stunting was found in 3.68% of infants, of whom 2.52% were exclusively breastfed, compared with 6.1% who were not exclusively breastfed. Underweight was found in 3.48% of infants who were not exclusively breastfed. Under weight was significantly associated with non-exclusive breastfeeding (p < 0.001).
Conclusion: Malnutrition exists in all forms in 6-month-old infants, even in those exclusively breastfed. Breastfed children were less likely to suffer from severe malnutrition.
Keywords: Malnutrition; Feeding; 6 Months; Togo
Breastfeeding is the best way to provide ideal nutrition for the ideal growth and development of infants. Since 2001, the World Health Organization (WHO) has recommended exclusive breastfeeding for infants up to 6 months of age [1]. Exclusive breastfeeding (EB) from birth to six months of age can reduce infant mortality by 13%, and it is estimated that the lives of 1.2 million children could be saved each year worldwide thanks to this measure [2]. Unfortunately, most children are not exclusively breastfed, but also consume water, milk, substitute or complementary foods, which are frequent sources of infection in unsafe environments [3]. Non-exclusive breastfeeding of infants under 4 months of age is a major cause of diarrhoea, and tends to reduce the mother’s milk production, thus contributing to the onset of malnutrition [4]. The United Nations Children’s Fund (UNICEF) estimates that malnutrition kills 13 million children a year, or 36,000 a day [5]. In Togo in 2017, the proportion of children exclusively breastfed for the first six months was 64.3% [8]. During the same period, children’s nutritional status was marked by prevalences that showed little change compared with those recorded in 2013. Stunting had a prevalence of 23.8% in 2017, compared with 27.4% in 2013; wasting a prevalence of 5.7% in 2017, compared with 27.4% in 2013; and underweight a prevalence of 15.2% in 2017, compared with 16.1% in 2013 [8,9].
In 2017, in the Plateaux region, 61.7% of children under 6 months were exclusively breastfed. Also, 12.7% of children under 5 were underweight, 25.4% stunted and 6.2% wasted [8]. The aim of this study was therefore to determine the prevalence of malnutrition in 6-month-old infants according to feeding mode in the Agou health district.
The Agou health district is one of 12 health districts in the Plateaux Region. It covers an area of 1026 km2. There were 32 health facilities, including 2 referral hospitals and 30 peripheral care units. This was a multicenter, cross-sectional study. Data collection took place from January 18 to July 17, 2021, a 6-month period, in 6 health centers in the Agou health district. All children of both sexes, aged six (6) months and apparently healthy, accompanied by their mother or carer, who came to the health facility during the study period for vaccination or anthropometric measurements, were included in the study. Not included in the study were children aged six (6) months whose mothers had refused to participate in the study, and children who were not accompanied by a parent. The parameters studied were sociodemographic characteristics, the child’s personal medical history, the parents’ medical history, clinical data and dietary practices. A team of 2 health workers from each health facility collected the data. Data collection took place on the day of the vaccination sessions. Sampling was consecutive, so women were recruited as they came to the vaccination units in the centers selected for the survey. To collect data from mothers/ guardians, the questionnaire was administered on the days of the vaccination sessions. The teams first consulted the child’s vaccination record before administering the questionnaire to the mothers/guardians. Weights and heights were measured according to WHO recommendations by the department’s trained interviewers. Infants were weighed unclothed using a SECA-type electronic baby scale, to an accuracy of 100g. Infant height was measured by two people using an infantometer, to an accuracy of 1mm. Brachial perimeter (BP) and cranial perimeter (CP) were measured by two people using a tape measure. The children were weighed using a scale and their heights were measured using a toise. Age, height and weight were used to calculate the weight-for-age (W/A), weightfor-height (W/H) and height-for-age (H/A) indices for each child, and to compare these WHO 2015 growth indices in terms of standard deviation (SD) against the reference median. We concluded after assessment of anthropometric constants according to WHO 2015 recommendations that, 6-month-old children in whom all 3 indices Size for Age, Weight for Age, Weight for Height were in the normal range had good nutritional status. Those in whom at least one of the 3 indices was not in the normal zone had a growth anomaly. At the end of the interview, we provided nutritional advice to correct any shortcomings noted in the interviews in relation to breastfeeding or dietary diversification. Data were entered into a database designed using Epidata software version 3.1. Statistical analysis was performed using R Studio software version 3.4.3. For descriptive analysis, results were presented as mean and standard deviation or median and inter-quartile range for quantitative variables, and as numbers and proportions for qualitative variables. For comparative analysis, the Chi 2 or Fisher test was used to compare qualitative variables, and the Student test to compare quantitative variables. The statistical threshold chosen was 0.05. During the survey phase, we obtained a field trip authorization by note N°02/21/EAM/UL/01/2021 from the University of Lomé and the Agou Prefectural Health Directorate in order to carry out research in the health district. Clear verbal consent from mothers was systematically required for data collection. Data collection was anonymous, and the data collected was used only for the purposes of the study.
A total of 353 mother-infant pairs whose infants were 6 months old participated in the survey. The average age of the mothers was 28 ±6 years (extremes 15 and 45 years), with the 30-35 age group the most represented at 27.77%. Mothers with an income-generating activity (IGA) represented 53.82% and housewives 43.63%. Mothers attended school in 77.91% of cases, with 46.45% at primary level. The sex ratio of the 353 children was 1.15, with 54% boys.
The overall prevalence of malnutrition was 48.4% (171 infants), including 11 cases of obesity (3.12%) and 19 cases of severe acute undernutrition (5.38%). Nutritional status according to the weight-for-height index was normal in 182 infants (55.56%), obesity in 11 infants (3.12%), moderate acute undernutrition in 21 infants (5.95%) and severe acute undernutrition in 19 infants (5.38%). Severe acute undernutrition was present in 12 infants (10.4%) not exclusively breastfed. There was no statistically significant correlation between exclusive breastfeeding up to six months and acute undernutrition (Table 1).
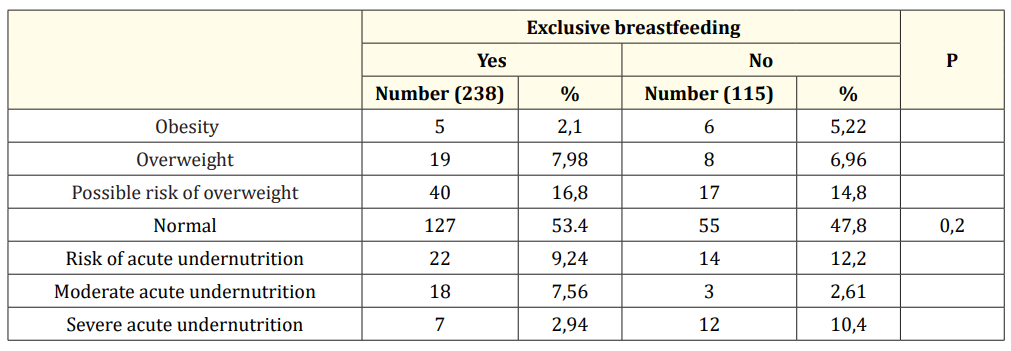
Table 1: Distribution of infants by weight-for-height index and exclusive breastfeeding status.
With regard to the size-for-age index, 257 infants (72.8%) had no growth problems. Severe growth retardation was found in 13 infants (3.68%), of whom 6 (2.52%) were exclusively breastfed, compared with 7 (6.1%) not exclusively breastfed. There was no statistically significant correlation between exclusive breastfeeding up to six months and chronic undernutrition (Table 2).
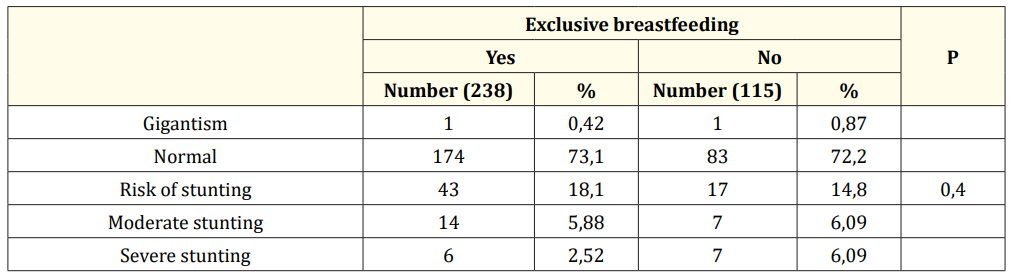
Table 2: Distribution of infants according to Size-For-Age index and exclusive breastfeeding practice.
For the Weight-for-Age index, 223 infants (63.17%) were of normal weight for age. No exclusively breastfed infant was severely underweight. There were 4 (3.48%) severely underweight infants who were not exclusively breastfed. Underweight was significantly associated with non-exclusive breastfeeding (p < 0.001) (Table 3).
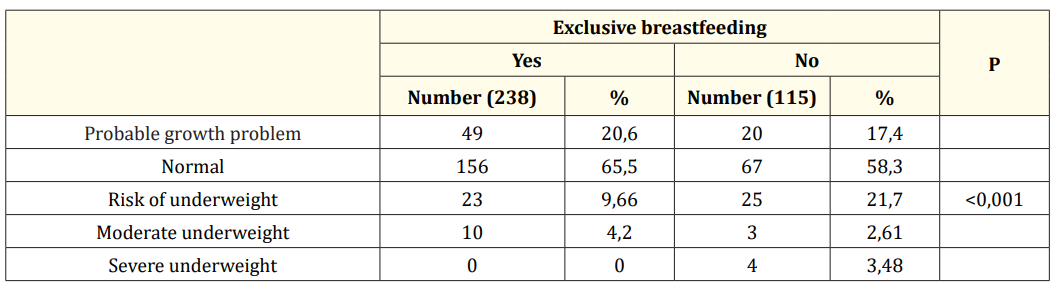
Table 3: Distribution of infants by weight-for-age index and exclusive breastfeeding status.
This multicenter study investigated malnutrition in 6-month-old infants according to their diet. The study focused on mother-child pairs from the Agou health district who brought their child home for the 6th-month weighing. This choice of study population enabled us to determine the prevalence of malnutrition in these infants. The prevalence of severe acute malnutrition was 5.38%. In hospitalized infants under 6 months of age in Burkina Faso, the prevalence of severe acute malnutrition was 8.18% [10]. Also in Sikasso hospital in Mali, the prevalence of severe acute malnutrition was 7.17% among hospitalized infants [11]. A significant proportion of infants under 6 months of age suffer from severe acute malnutrition. It was associated with death in a hospital study. In a cohort study of infants admitted to hospital in Kenya from 2007 to 2009, severe acute undernutrition was associated with inpatient death and death within one year of discharge. The use of MUAC to detect severe acute undernutrition based on brachial circumference and weight-for-age index predicted in-hospital and post-discharge mortality [12].
There was no statistically significant correlation between exclusive breastfeeding up to six months and acute undernutrition. Acute undernutrition in infants under 6 months of age is often overlooked. It is a complex, multifactorial problem associated with numerous risk factors in infants under 6 months of age. It is not only linked to the practice of exclusive breastfeeding. Multiple risk factors were statistically associated with acute undernutrition. These included poverty; low maternal body mass index; small size at birth; late onset of breastfeeding; milk feeding; and recent history of diarrhoea. Protective factors associated with a significantly reduced likelihood of acute undernutrition in infants under 6 months of age included educated mothers; working mothers and exclusive breastfeeding [13].
There was no statistically significant correlation between exclusive breastfeeding up to six months and chronic undernutrition. This was to be expected, given the young age of the infants. Chronic malnutrition takes time to set in. A study in Mexico looked at the association between breastfeeding and stunted growth. Breastfeeding was identified as one of the key affordable and modifiable maternal health behaviors that protect against stunting. Breastfeeding and female gender were consistent protective factors against child stunting in all models. In contrast, low birthweight, short maternal stature, higher number of children under 5 years of age and moderate to severe food insecurity were consistent risk factors for child stunting in all models [14].
Many maternal interventions are available to improve infant growth and nutritional status in low- and middle-income countries. Many maternal interventions have been shown to improve infant growth or feeding. These included breastfeeding promotion, education, support and counseling. The mother’s mental health, although under-researched, has been shown to have a positive impact on infant growth. There is also evidence of the positive impact of women’s empowerment, conditional cash transfers, water, sanitation and hygiene, and agricultural interventions. Effectiveness was increased when implemented as part of a multi-sectoral program [15].
Malnutrition exists in all forms in infants aged 6 months, even in those who are exclusively breastfed. Breastfed infants were less likely to suffer from severe malnutrition. Nutritional assessment should be systematically carried out on infants whenever they come into contact with the healthcare system for treatment. The prevention of malnutrition requires the promotion of exclusive breastfeeding.
The authors declare no conflicts of interest.
EOT contributed to the study design, data analysis and drafting of the manuscript. EKD reviewed the study protocol and revised the draft. AF collected data and reviewed the literature. FA revised the draft.
Special thanks to the Agou health district team.
Copyright: © 2024 Foli AGBEKO., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.