Pasupuleti Siva Pradeep, Sushil Singla, Shweta Kumari, Rashmie Prabha and Anand Narayanan*
Department of Pediatrics, Sarvodaya Hospital and Research Centre, Sector 8, Faridabad -121006
*Corresponding Author: Anand Narayanan, Associate Consultant, Sarvodaya Hospital and research centre, Sector 8, Faridabad -121006.
Received: December 14, 2023; Published: December 23, 2023
Citation: Anand Narayanan., et al. “Subcutaneous Emphysema in a Neonate -The Tip of the Iceberg”. Acta Scientific Paediatrics 7.1 (2024): 19-21.
Subcutaneous emphysema is a rare complication of positive pressure ventilation, especially in neonates. Very few cases are available in literature. We report a postterm neonate referred to us in a state of cardiac arrest with gross subcutaneous emphysema in neck and upper chest region which immediately gave us a clue of the underlying pneumothorax and the same was confirmed on chest x-ray after initial resuscitation. So we were able to do a needle thoracotomy followed by chest tube placement following which respiratory distress improved. Subcutaneous emphysema also weaned gradually. This case demonstrates the importance of prompt identification of subcutaneous emphysema as a clue to its underlying etiology. Care should be taken to avoid high pressures during positive pressure ventilation in order to avoid such complications.
Keywords: Subcutaneous; Emphysema; Neonate; Iceberg
A 2 day old post term male baby weighing 3.8kg delivered by caesarean section due to presence of meconium stained liquor at 43 weeks of POG at a peripheral centre and was admitted there soon after birth for respiratory distress and suspected early onset neonatal sepsis. There he was put on bubble CPAP after which the respiratory distress worsened and the baby started to develop swelling over the anterior chest wall, neck and face. So he was referred to our hospital for further management. When he presented to our emergency there was no pulse, SPO2 was non recordable. CPR as per NRP protocol was given for about 5 minutes, requiring 2 doses of adrenaline after which return of spontaneous circulation was achieved. He was put on ventilator and ionotrope support. On examination there was swelling over the anterior chest wall, neck, face and abdominal distension. On palpation crepitus was demonstrated over the chest wall, neck and mastoids bilaterally. A chest and neck X-ray was done immediately which demonstrated right sided pneumothorax with pneumomediastinum and a mediastinal shift. Gross subcutaneous emphysema involving the chest wall, neck extending up to and beyond mastoid was also seen on Xray. Needle decompression was done immediately and later a chest tube was placed. Few hours later pneumothorax started to settle. Ventilator and ionotrope support continued. Treatment for sepsis was continued with higher antibiotics. Apart from this baby had severe PAH, PPHN, AKI, seizures. His condition worsened in the next few days. He was transferred to another hospital on request where he unfortunately succumbed.

Figure 1: Clinical picture demonstrating subcutaneous emphysema of anterior chest wall, neck and facial edema.

Figure 2: Radiograph of neck and chest demonstrating right sided pneumothorax, pneumomediastinum with mediastinal shift and subcutaneous emphysema of chest wall and neck extending up to and beyond mastoid.
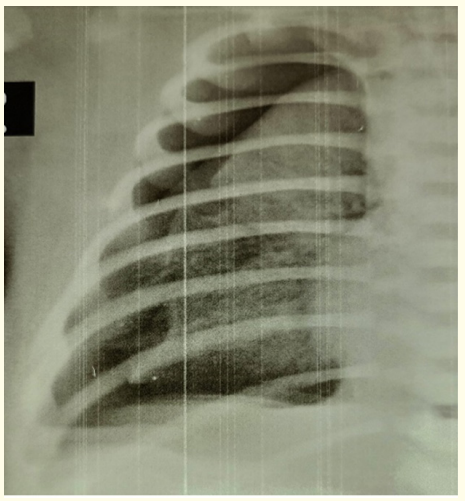
Figure 3: Radiograph of right lung showing gingko leaf sign-gas outlining the pectoralis muscle.
Subcutaneous emphysema is the infiltration of air in the subcutaneous layer of skin [1]. Incidence in general is 0.43 to 2.34% and is even rarer in neonates [2]. It is a rare complication of positive pressure ventilation. It can be caused due to injury to the parietal pleura that allows air to enter the pleural and subcutaneous tissues, air from the alveolus spreading into the endovascular sheath and lung hilum into the endothoracic fascia, air in the mediastinum spreading into the cervical viscera and other connected tissue planes [3]. Proper history taking is necessary to diagnose and rule out other causes. Crepitus on palpation is the most typical physical feature connected to subcutaneous emphysema. There may be bloating or distention in the chest, face, neck, and abdomen. On x-ray a ginkgo leaf sign may be present, which is striations of gas along the pectoralis major [1]. Subcutaneous emphysema usually localizes in the clavicular region as a pocket of air in severe cases [2]. Evaluating the cause of subcutaneous emphysema is important as it is associated with haemodyanamic and respiratory compromise in severe cases like the one being reported. A case was reported in which subcutaneous emphysema was mistaken for allergic reaction and angioedema [4]. Even in this case the physician in the peripheral center who initially treated the baby mistook subcutaneous emphysema as anasarca. Any type of mechanical ventilation including continuous positive airway pressure and intermittent positive pressure ventilation during resuscitation can lead to this serious complication and conservative treatment normally suffices until the air leak closes [5]. We speculate the cause in this case to be either due to high pressure given during PPV during resuscitation or from CPAP leading to pneumothorax and pneumomediastinum further progressing as subcutaneous emphysema. Although rare, there are few case reports of subcutaneous emphysema due to positive pressure ventilation in neonates [5,6]. There was another case reported in which alveolar rupture caused by crying at birth was speculated to be the cause [7]. Nonetheless, due to the benefit of CPAP outweighing the potential danger of developing subcutaneous emphysema, doctors should still adhere to the standard of care and provide infants in respiratory distress with CPAP [6].
Copyright: © 2024 Anand Narayanan., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.