Shamsun Nahar Shanta1*, Afroza Begum2, Syed S Haque3, Tahmina Jesmin3, Abdullah-Al Mamun4, Shanjida Sharmim4, Ashiqur Rahman Khan5 and Ashraful Islam6
1 Medical Officer, Department of Pediatric Nephrology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
2 Professor and Chairman, Department of Pediatric Nephrology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
3 Associate Professor, Department of Pediatric Nephrology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
4 Assistant Professor, Department of Pediatric Nephrology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
5 Associate Professor, Department of Medicine, Colonel Maleque Medical College, Manikganj, Bangladesh
6 Assistant Professor, Department of Pediatrics, Comilla Medical College, Comilla, Bangladesh
*Corresponding Author: Shamsun Nahar Shanta, Medical Officer, Department of Pediatric Nephrology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Received: March 15, 2023; Published: November 28, 2023
Citation: Shamsun Nahar Shanta., et al. “The Risk Factor Associated with Relapse in Childhood Nephrotic Syndrome- A Hospital Based Retrospective Study”. Acta Scientific Paediatrics 6.10 (2023): 49-53.
Background: NS is a disease of relapse. So, it is very important to find out such children who are prone to develop frequent relapses and the predictors responsible for deterioration. This retrospective study was conducted in the Department of Pediatric Nephrology, Bangabandhu Sheikh Mujib Medical University, from September 2016 to August 2017.
Methods: A total of 75 patients of idiopathic nephrotic syndrome (INS) with the initial attack, aged 1–18 years, were enrolled in this study. All patients were treated with prednisolone 60 mg/m2/day, single morning dose for six weeks, followed by 40 mg/m2 every alternate day for another six weeks and were analyzed and followed up for a minimum period of six months to identify the risk factors related to relapses.
Result: Among them, 50 (66.7%) were males, 25 (33.3%) were females, with a male: female ratio of 2:1. Ten (13.3%) children had no relapse, 18 (24.0%) had infrequent relapse, and 40 (53.3%) had frequent relapse. Children responding between 2 and 4 weeks after the start of treatment had a higher chance of relapse (P = 0.002) than those who responded less than one week. Only urinary and respiratory tract infections are independent risk factors for subsequent relapse. Children with INS who have UTI at onset had a 1.55 times more chance for further relapse, and RTI caused a 1.42 times more chance for relapse. Patients with low serum albumin have 1.91 times more chance for relapse than those with high albumin, with insignificant association.
Conclusion: Young age at diagnosis of INS, male gender, low serum albumin, and infections were predictive risk factors of multiple relapses. So, physicians should be vigilant to monitor these patients closely and counsel the families of nephrotic children regarding the prediction of subsequent relapses and outcomes.
Keywords: Children; INS; Risk Factor
Idiopathic nephrotic syndrome (INS) is a common childhood illness characterized by massive proteinuria, hypoalbuminemia, hyperlipidemia and oedema [1]. It constitutes about 72% to 85% of all nephrotic syndrome (NS) in children. About 90% of the first episodes of INS achieve remission by corticosteroid treatment. However, 70 to 80% of these children experience relapse, and 30% of them develop frequent relapse [2,3]. Multiple studies have tried to identify the risk factors associated with a relapsing pattern of illness but remains unsolved how to predict this relapse and what should be the management strategy [4]. Different risk factors such as young age at diagnosis, male gender, initial time to response, decreased serum albumin level and haemeturia have been reported in frequent relapsing nephrotic syndrome (FRNS) and steroid-dependent nephrotic syndrome (SDNS) with conflicting results. There are only a few predictors of the risk of subsequent relapses after the initial response [5]. Karim et al. showed that young age and low serum protein level at onset were associated with increased frequency of relapse [6]. Biswas et al. showed that infection is an important cause of relapse in minimal change nephrotic syndrome (MCNS), prevention and treatment of which could reduce proteinuria without the necessity of steroid treatment [7]. Gulati et al. also showed that asymptomatic UTI might be an important and undiagnosed cause of relapse [8]. In our country, illiteracy, inadequate health care facilities and referral system, lack of knowledge about the disease and poor compliance cause the failure of early detection and prevention of disease relapse [9]. Hence, predicting and preventing risk factors is the key to successfully managing INS in children.
This retrospective observational study was carried out in the Department of Pediatric Nephrology, Bangabandhu Sheikh Mujib Medical University, from September 2016 to August 2017. A total of 75 patients with idiopathic steroid-sensitive nephrotic syndrome who fulfilled the inclusion criteria were taken. Patients with systemic and chronic diseases, congenital nephrotic syndrome, secondary causes of nephrotic syndrome, steroid resistance, hematuria, hypertension, incomplete medical records (demographic and laboratory data), hypocomplementemia and patients who had received previous immunosuppressive treatment were excluded from the study. After confirmed diagnosis and screening out of infection, all patients were treated with prednisolone 60mg/m2 / day single morning dose for six weeks, followed by 40 mg/m2 / day every alternate day for another six weeks. The following variables were recorded for all subjects: age, sex, height, body weight, history of infection, blood pressure, and laboratory findings such as serum protein, serum albumin, serum cholesterol, serum creatinine, complete blood count, as well as urinalysis, at the time of the INS diagnosis. The response to treatment was assessed by clinical examination, such as consecutive protein-free urine for three days, adequate diuresis, and no features of oedema, ascites, and infections. The response was also assessed by doing spot urinary protein creatinine ratio. Parents were counselled about disease course, treatment, prognosis, and drug toxicity and trained about interpreting and testing urine at home by the heat precipitation method. All patients were followed for at least 6 months after completion of the treatment of the first episode. Search for infection was done at every visit in both relapse and no-relapse groups. Patient characteristics (age, sex) and clinical parameters (presenting complaints, treatment history, time to remission, number of relapses within six months) were obtained and recorded in the data collection sheet. Relapse was detected by using bedside urine for albumin 3+ or more for three consecutive days. Relapse was treated by the daily dose of prednisolone 60mg/m2/day up to protein-free for three consecutive days. Then, 40mg/m2 every alternate day for four weeks in infrequent relapse (IFRNS), and gradually, the dose was tapered by 5mg every two weeks in frequent relapse (FRNS). Patients were categorized during follow-up into the following groups, depending on their response to therapy: Remission: bedside urine albumin nil for three consecutive days. Relapse urine albumin 3+ or more for three consecutive days, previously in remission. IFRNS: <2 relapses within six months of the initial response. FRNS: ≥2 relapses within six months of initial response or four or more relapses within one year. All the investigations were done at the pathology and biochemistry laboratory, BSMMU, Shahbag, Dhaka. After collection, all the data were checked and edited. Several demographic, clinical and laboratory variables were studied from hospital records and discharge papers to determine relapse risk factors. Data were coded, edited, entered into a computer, and analyzed using the SPSS program. Data presented on a categorical scale were expressed as frequency and corresponding percentages. They were compared between groups using the Chi-square (χ2) test. In contrast, data presented on a continuous scale were expressed as mean and standard deviation from the mean. They were compared between groups using Student’s t-Test and further analyzed by multivariate regression analysis to find out risk factors for relapse where p-value < 0.05 was taken as significant.
Out of 75 patients, the majority (61.3%) were between 1-5 years of age, with a mean of 5.3±3.3 years. Fifty of 75 subjects (66.7%) were male, and the rest (33.3%) were female, giving a male-female ratio of roughly 2:1 (Figure 1). Regarding socioeconomic condition, 66.7% of the subjects came from poor socioeconomic class, followed by 29.3% from the middle class and only 4% from the upper class (Table 2). Sixty percent of the subjects came from rural, 35% from urban areas, and 5% from urban slum areas (Table 3). Among the study subjects, atopy, family history of kidney disease, hypertension and hematuria were presented at 56%, 10.7%, 20% and 16%, respectively. Table IV shows the baseline characteristics of study subjects at presentation. The parameters such as gender, infections, and serum albumin level did not differ significantly among the three age groups except serum cholesterol level and UTP, which were significantly (p = 0.03) lower (≤500mg/dl) in the 1-5 years age group and UTP is higher (5.90 ± 3.54 mg/dl, p = 0.003) in children >10 years of age. Bar diagram showing the association of age of onset with relapse in study subjects. The mean age of children with relapse was 5.48 ± 3.39, and without relapse was 4.38 ± 1.90 years, but there was no statistically significant difference between these two groups. Multivariate logistic regression analysis of parameters showed that only urinary and respiratory tract infections were independent risk factors for subsequent relapse. Children with INS who have UTI at onset had 1.55 times more chance for further relapse, and RTI showed 1.42 times more chance for relapse. Patients with low serum albumin have 1.91 times more chance for relapse than those with high albumin, with insignificant association. There was also no significant relationship between serum cholesterol level and relapse.
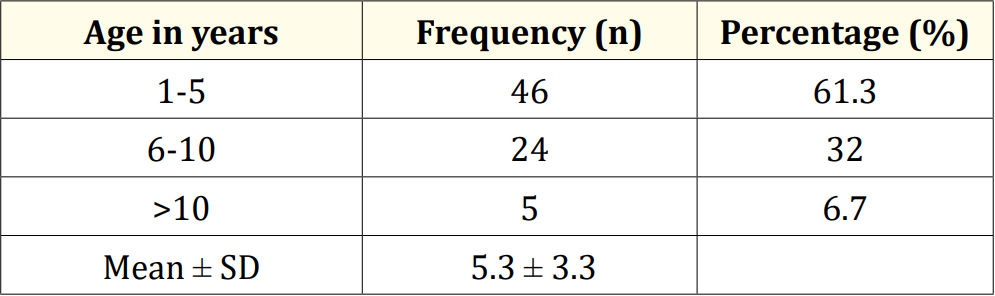
Table 1: Distribution of patients by age (N = 75).
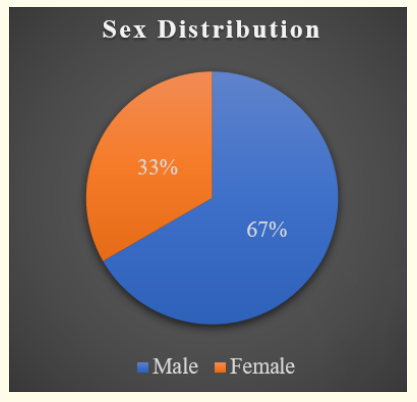
Figure 1: Sex distribution of the study population (N = 57).
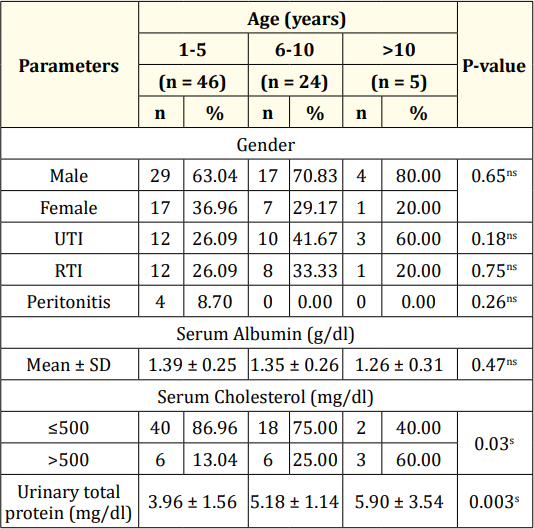
Table 2: Risk factors distribution of the study patients (n = 75).
Ns = Not significant (p > 0.05), s = Significant (p < 0.05).
P value was reached from the Chi-Square test for qualitative data and the ANOVA test for quantitative data.
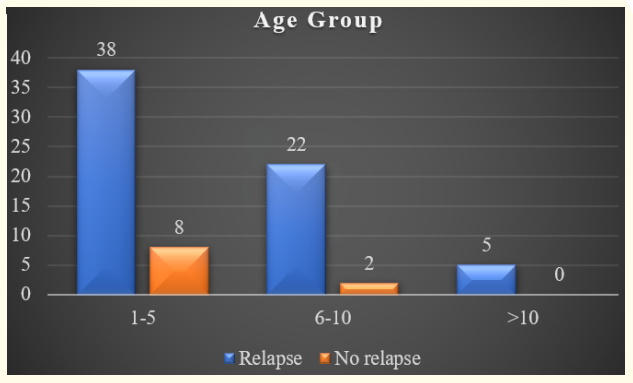
Figure 2: Patient characteristics at presentation according to age groups (n = 75).
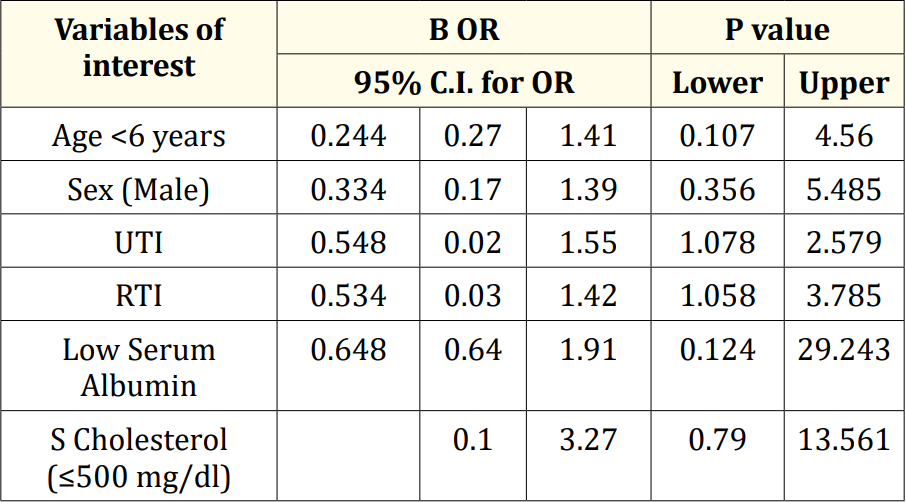
Table 3: Multivariate logistic regression analysis of risk factors for relapse.
The long-term outcomes of children with steroid-sensitive nephrotic syndrome are far better than a resistant disease. A subgroup of SSNS that behaves as frequently relapsing or steroiddependent nephrotic syndrome is subjected to recurrent steroid therapy, rendering them fatal side effects [10]. A total of 75 patients with an initial episode of INS were analyzed and followed for at least six months after the completion of treatment of the initial attack. Maximum 40 (53.3%) children had two or more than two relapses, 18 (24%) less than two relapses, 10 (13.3%) children had no relapse, 5 (6.7%) had steroid resistance, and 2 (2.7%) had steroid dependence within six months of follow- up period. This finding is comparable with the findings of Chwat., et al. [11]. Frequently relapsing nephrotic syndrome is the most common subgroup. The mean age of the patient ranges from 5.48 ± 3.39 years in the relapse group and 4.38 ± 1.90 years in the relapse group. In agreement with previous studies performed by Constaninescu et al. and Takeda et al., no correlations were present between age at presentation and future relapses among patients with NS [3,5]. On the other hand, Andersen., et al. and Sarker., et al. found a significant correlation between age at presentation <4 and <5 years, respectively and an increased incidence of relapses in the future [4,12]. A recent study from India by Sinha., et al. [13] found that patients with FR were younger at the onset of the disease, and the frequency of relapses declined with age. Out of 75 patients, 50 (66.7%) were male, and 25 (33.3%) were female, with a male-tofemale ratio of 2:1. Male predominance was observed in patients with relapse. Andersen et al. reported that the male gender was associated with a higher risk of steroid dependency and FRNS despite the prolongation of the steroid course [12]. Noer., et al. also found that male gender is a predictive factor for FR [14]. Takeda., et al. showed that low serum protein or albumin is a significant predictor for frequent relapses in future [5]. Our study also showed that out of 75 patients, albumin levels did not differ significantly among the three age groups except serum cholesterol level and UTP, which were significantly (p = 0.03) lower (≤500mg/dl) in 1-5 years age group and UTP (5.90 ± 3.54 mg/dl, p = 0.003) was higher in >10 years age groups. This finding was comparable with that of Ali., et al. [16]. Of those 75 patients, 28 suffered from various types of infections at the onset of the disease. Urinary tract infection was the most common (26.2%) in the relapse group, followed by respiratory tract infections (15.2%) and peritonitis (8.7%). In patients receiving alternate-day prednisone, one nonrandomized trial and two RCTs suggested that the frequency of relapse was reduced if prednisone is administered for 5-7 days at the onset of an upper respiratory infection [18]. However, Biswas BK [7] described that infection is an important cause of relapse, and Gulati., et al. [8] stated that asymptomatic UTI might be an important and underdiagnosed cause of relapse.
Every hospital-based study has some limitations and the present study undertaken is no exception to this fact. The limitations of the present study are mentioned. Therefore, the results of the present study may not be representative of the whole of the country or the world at large. The number of patients included in the present study was less in comparison to other studies. Because the trial was short, it was difficult to remark on complications and mortality.
Young age at diagnosis of INS, male gender, low serum albumin, and infections were predictive risk factors of multiple relapses. So, physicians should be vigilant to monitor these patients closely and counsel the families of nephrotic children regarding the prediction of subsequent relapses and outcomes. We suggest that further studies be performed without a six-month time limit to assess other possible risk factors for relapse in pediatric nephrotic syndrome.
No funding sources.
None declared.
Copyright: © 2023 Shamsun Nahar Shanta., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.