Urmi Roy1*, Aniruddha Mondal2, Khondaker Mobasher Ahmed3, MD Rukunuzzaman4 and Wahiduzzaman Mazumder5
1 Registrar, Department of Pediatric, Kurmitola General Hospital, Dhaka, Bangladesh
2 Assistant Registrar, Department of Physical Medicine National Institute of Traumatology and Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
3 Assistant Professor (Pediatric Gastroenterology and Nutrition), Comilla Medical College, Cumilla, Bangladesh
4 Head of the Department Pediatric Gastroenterology and Nutrition, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
5 Associate Professor, Department of Paediatric Gastroenterolog and Nutrition, Bangabandhu Seikh Mujib medical University (BSMMU), Dhaka, Bangladesh
*Corresponding Author: Urmi Roy, Registrar, Department of Pediatric, Kurmitola General Hospital, Dhaka, Bangladesh.
Received: November 07, 2023; Published: November 20, 2023
Citation: Urmi Roy., et al. “A Comparative Study on the Performance of Esophageal Varices in Pediatric Patients with Chronic Liver Disease (CLD)”. Acta Scientific Paediatrics 6.10 (2023): 24-32.
Background: Chronic Liver Disease (CLD) is a distressing medical condition that affects millions of children worldwide, posing significant challenges to their health and well-being. Among the myriad complications that can arise from CLD, esophageal varices represent a critical concern. Esophageal varices are abnormal, enlarged blood vessels in the esophagus that can rupture, leading to life-threatening hemorrhage. While much research has focused on adult populations, relatively limited attention has been given to understanding esophageal varices in pediatric patients with CLD. Esophageal varices are a potentially fatal consequence of CLD, with the risk of bleeding being a significant concern. Early detection and management are essential to prevent severe complications.
Aim of the study: This study aims to bridge this knowledge gap by conducting a comprehensive comparative analysis of esophageal varices’ performance in children with CLD.
Methods: This cross-sectional study was conducted over two years, from April 2019 to October 2021, at the Department of Pediatric Gastroenterology and Nutrition at Bangabandhu Sheikh Mujib Medical University (BSMMU) in Dhaka, Bangladesh. It included 32 patients diagnosed with Chronic Liver Disease (CLD), categorized into two groups: Group A (Patients without Esophageal Varices) and Group B (Patients with Esophageal Varices). Each patient underwent a comprehensive clinical assessment, including physical examinations and data collection, with informed consent and ethical approval. Inclusion criteria covered patients under 18 with diagnosed chronic liver disease, while exclusion criteria ruled out those with gastrointestinal bleeding history, prior varices treatment, or severe ascites. Data analysis employed SPSS software, presenting findings with various statistical measures, such as frequency, percentage, and Chi-square or Mann-Whitney U tests as appropriate.
Result: In a study of 32 patients, 75% had esophageal varices with varying grades, and 25% did not. Gender distribution showed 62.5% males in Group A and 79.2% in Group B. Both groups had a similar age distribution. Consanguinity was found in all Group B patients, and jaundice history was prevalent in both groups. Liver disease history was more common in Group A. Anemia rates were 37.5% in Group A and 58.3% in Group B. Stigmata were significantly more common in Group B. Palpable spleens were significantly more common in Group B. None in Group A had ascites, while 75% of Group B had ascites. Diagnoses included Wilson’s disease, Chronic hepatitis B, Autoimmune hepatitis, Cryptogenic cirrhosis, Biliary cirrhosis, and Glycogen storage disease. Hemoglobin values and total counts did not differ significantly. Platelet count was higher in Group A. Group A had lower bilirubin levels, while albumin was higher. Prothrombin time and INR were higher in Group B. At the same time, liver stiffness and serum fibrosis scores were significantly higher in Group B. Child-Pugh scores showed significant differences between the groups.
Conclusion: This study sheds light on the critical significance of early detection and comprehensive care for esophageal varices in children with Chronic Liver Disease (CLD). Collaboration among pediatric specialists is pivotal for effective management. Future research should focus on innovative approaches to enhance the quality of life and outcomes for these vulnerable patients.
Keywords: Comparative Study; Performance; Esophageal Varices; Pediatric Patients and Chronic Liver Disease (CLD).
Chronic liver disease in the clinical setting refers to a condition where the liver undergoes progressive destruction and regeneration, leading to fibrosis and cirrhosis [1]. It is characterized by a duration exceeding six months and encompasses various liver pathologies, including chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma. Cirrhosis is marked by the development of regenerative nodules surrounded by fibrous bands in response to chronic liver injury, resulting in portal hypertension and advanced liver disease [2]. Hepatic fibrosis, a response to liver injury, involves the accumulation of extracellular matrix (ECM) and can disrupt the hepatic vasculature, affecting blood supply and compromising liver function [3]. Esophageal varices are highly dilated sub-mucosal veins in the lower esophagus [4], often caused by portal hypertension, frequently due to cirrhosis [5,6]. These varices can lead to severe bleeding, potentially fatal if left untreated, and are typically diagnosed through esophagogastroduodenoscopy [7]. Esophageal varices develop at a rate of 7-8% annually and progress from small to large varices at a rate of 10-12% per year [8]. When cirrhosis is initially diagnosed, esophageal varices are present in around 40% of patients with the compensated disease and approximately 60% of those with decompensated disease [9]. The 2008 APASL criteria established two categories for varices: high risk (large varices >5 mm with specific red signs) and low risk (small varices ≤5 mm without red signs) [10]. The risk of variceal bleeding is closely related to variceal size and the presence of red signs as assessed by endoscopy. The annual risk of bleeding from esophageal varices is 5% for small varices and 15% for large varices [11]. Despite standard treatments, 15-20% of patients with acute variceal bleeding do not respond, and about 80% of them do not survive even with rescue therapies like trans-jugular intrahepatic portosystemic shunt (TIPS) [12]. Following bleeding, the majority of patients (55%) present with hemodynamic shock, and over a third exhibit other signs of decompensation, including ascites (34%) and encephalopathy (13%) [13]. Variceal hemorrhage is a leading cause of morbidity and mortality in individuals with portal hypertension, highlighting the importance of preventing variceal hemorrhage. Initial identification of patients with esophageal varices and primary prophylaxis with beta-adrenergic receptor antagonists can reduce the incidence of variceal hemorrhage. Primary prophylaxis, involving non-selective beta-blockers (NSBBs), can decrease the risk of the first bleeding episode from 27% to 17%, and esophageal variceal ligation (EVL) can reduce it by 64% in high-risk cirrhotic patients. Therefore, early detection and screening for varices are crucial for the treatment and prevention of progression [14]. Although upper gastrointestinal tract (GIT) endoscopy is the gold standard for variceal diagnosis and assessment, it is time-consuming, invasive, and carries risks, especially in children [15]. In countries with limited pediatric endoscopy facilities, there is a need for a reliable, noninvasive test to replace upper GI endoscopy. Predicting esophageal varices through noninvasive methods can help identify patients at a high risk of having varices, reducing unnecessary endoscopy, particularly in children with chronic liver disease (CLD). Noninvasive markers of liver fibrosis, such as transient elastography, Fib-4, Forns Index, and Lok Score, have shown promise in predicting esophageal varices in cirrhotic patients, given that portal hypertension often results from increased hepatic resistance due to fibrosis [16]. According to the updated Baveno VI guidelines, patients with compensated advanced chronic liver disease with liver stiffness <20 kPa and a platelet count >150,000/μL may avoid routine endoscopy for variceal screening [17]. However, limited efforts have been made in our country to predict esophageal varices in children using these parameters.
This descriptive cross-sectional study occurred at the Department of Pediatric Gastroenterology and Nutrition at Bangabandhu Sheikh Mujib Medical University (BSMMU) in Dhaka, Bangladesh. The study spanned two years, running from April 2019 to October 2021. All 32 patients diagnosed with Chronic Liver Disease (CLD) participated in and were subject to analysis within this research endeavor. The study population was divided into two groups; Group A (Patients without Esophageal Varices) and Group B (Patients with Esophageal varices). Upon entry, each patient underwent a comprehensive clinical assessment, which included a physical examination. During this evaluation, observations such as jaundice, hepatomegaly, splenomegaly, and ascites were meticulously documented using a structured questionnaire. Before data collection, informed consent was obtained from every patient, and the gathered information was treated with utmost confidentiality. Additionally, the study received ethical approval from the institution’s ethical committee.
The investigation results were systematically collected and documented through a structured questionnaire. Approximately 6 ml of venous blood was extracted for subsequent laboratory analysis. An upper gastrointestinal endoscopy was performed to determine the presence or absence of esophageal varices and related findings, utilizing an Olympus video endoscope GIF Q 150 endoscopy machine. A single gastroenterologist from the Pediatric Gastroenterology and Nutrition department of BSMMU conducted all endoscopic procedures. The classification of esophageal varices was based on consistent criteria. Esophageal varices were described using Conn’s classification, which divides them into four grades, with abnormally dilated submucosal veins in the lower third of the esophagus as esophageal varices [18].
Data for this study were gathered by administering a wellstructured questionnaire to the participants. Subsequently, an analysis of the data collected from these individuals was performed. We employed SPSS (Statistical Package for the Social Sciences) version 26 software to conduct the statistical analysis. The study’s findings were presented in tabular format, utilizing frequency and percentage values. We utilized various statistical measures to depict the total sample’s characteristics comprehensively. Continuous variables were summarized using the median and interquartile range (IQR), while categorical variables were summarized through frequency distributions. We employed the Chi-square test or the Fisher Exact test to explore potential associations between categorical variables, depending on the specific circumstances. In cases where the data exhibited skewness, we applied the Mann-Whitney U test to examine associations among continuous variables.
Among the 32 patients, 75.0% had esophageal varices (24), while the remaining 25.0% did not (8). Of those with esophageal varices, 20.0% had grade I, 37.5% had grade II, 25.0% had grade III, and 16.7% had grade IV varices. Regarding gender distribution, 62.5% of Group A and 79.2% of Group B were male. No significant age difference was observed between the groups (p = 0.378). Both groups had a similar age distribution, with 62.5% of patients in Group A and 50.0% in Group B belonging to the over-10-years age group. Consanguinity was found in all five patients in Group B. At the same time, jaundice history was present in 87.5% of patients in Group A and 91.7% in Group B. Liver disease history was reported in 25.0% of patients in Group A and 4.2% in Group B. There were no significant differences between the groups regarding age, gender, consanguinity, jaundice history, or liver disease (p > 0.05). In Group A, 37.5% had anemia; in Group B, 58.3% had anemia, with no significant difference (p = 0.411). Stigmata was present in 50.0% of patients in Group A and 91.7% in Group B, with a significant difference (p = 0.023). Both groups had 75.0% of patients with palpable livers, but palpable spleens were significantly more common in Group B (95.8%) compared to Group A (25.0%) (p < 0.001). None of the patients in Group A had ascites, while 75.0% of patients in Group B had ascites, with a highly significant difference (p < 0.001). Diagnoses included 50.0% as Wilson’s disease, 18.8% as Chronic hepatitis B, and 12.5% as Autoimmune hepatitis. Others were Cryptogenic cirrhosis (9.4%), Biliary cirrhosis (6.3%), and Glycogen storage disease (3.1%). Median hemoglobin values were 12.5 gm/dl in Group A and 10.2 gm/dl in Group B, with no statistical difference (p = 0.160). Total counts showed no significant difference (p = 0.124). The median platelet count was significantly higher in Group A (315,000/µL) than in Group B (90,000/µL) (p < 0.001). Group A had a significantly lower median bilirubin count (1.3 gm/ dl) compared to Group B (2.7 gm/dl) (p = 0.018). No significant differences existed in ALT, GGT, and cholesterol levels (p > 0.05). Prothrombin time and INR were significantly higher in Group B (p < 0.001), while albumin was significantly higher in Group A (p < 0.001). Table 5 displayed liver stiffness and serum fibrosis scores, with LSM, Fib-4, Forns Index, and Lok scores significantly higher in Group B (p < 0.001). Child-Pugh scores revealed all patients in Group A to be Class A, whereas Group B had 12.5% Class A, 37.5% Class B, and 28.1% Class C, with a highly significant difference between the groups (p < 0.001).
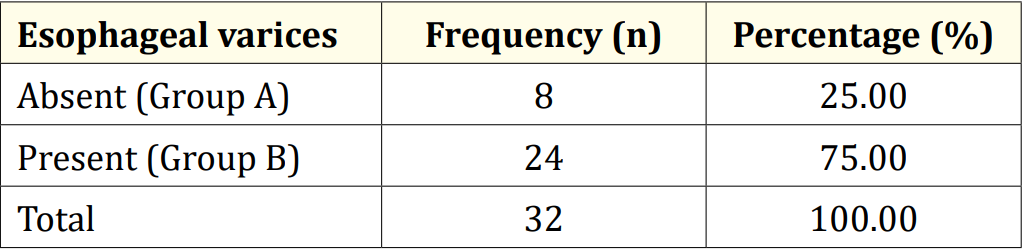
Table 1: Distribution of patients by esophageal varices (N = 32).
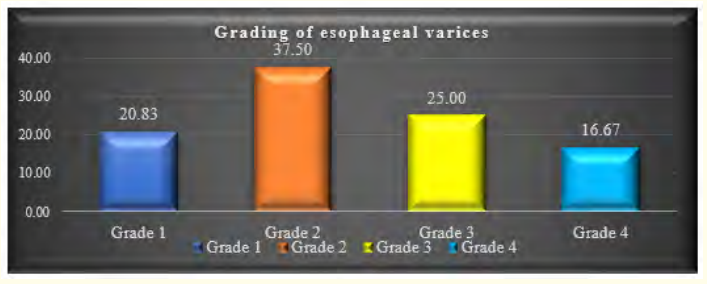
Figure 1: Distribution of patients by grading of esophageal varices (n = 24).
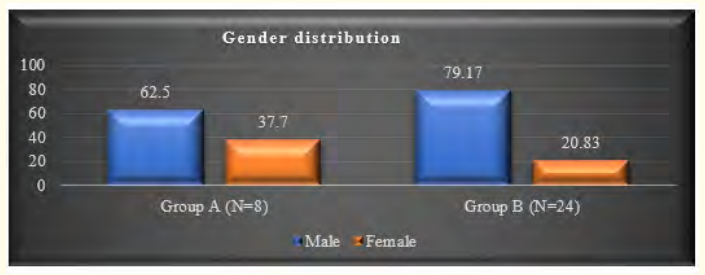
Figure 2: Gender distribution of the study population (N = 32).
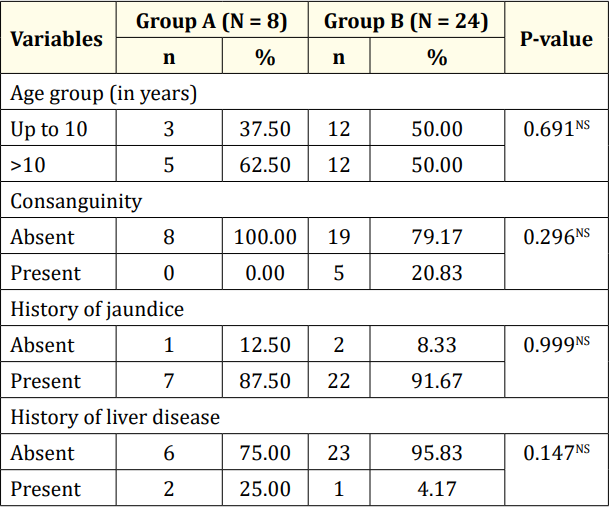
Table 2: Socio-demographic and disease history of the studied population (N = 32).

Table 3: Clinical characteristics of the studied population (N = 32).
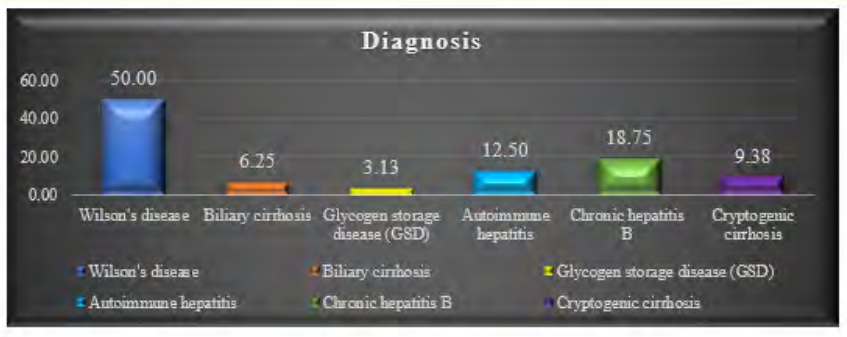
Figure 3: Diagnosis of the study population (N = 32).
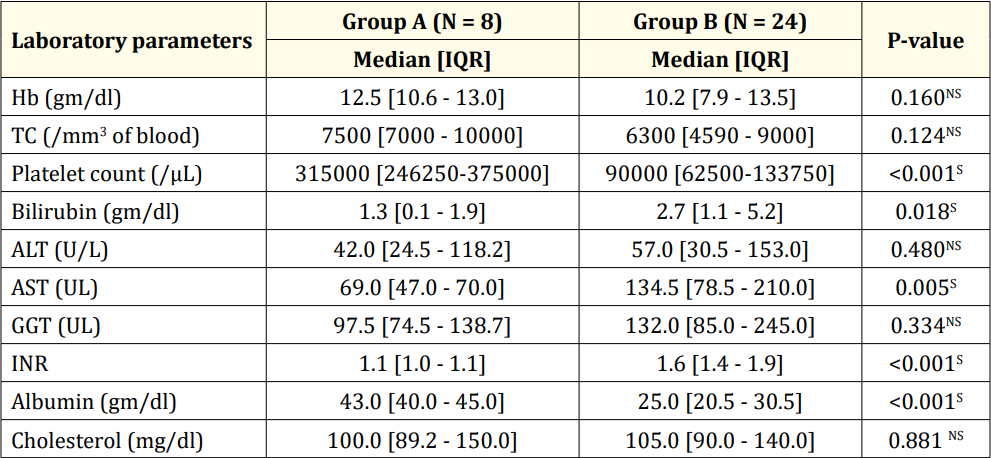
Table 4: Laboratory parameters of the study population (N = 32).
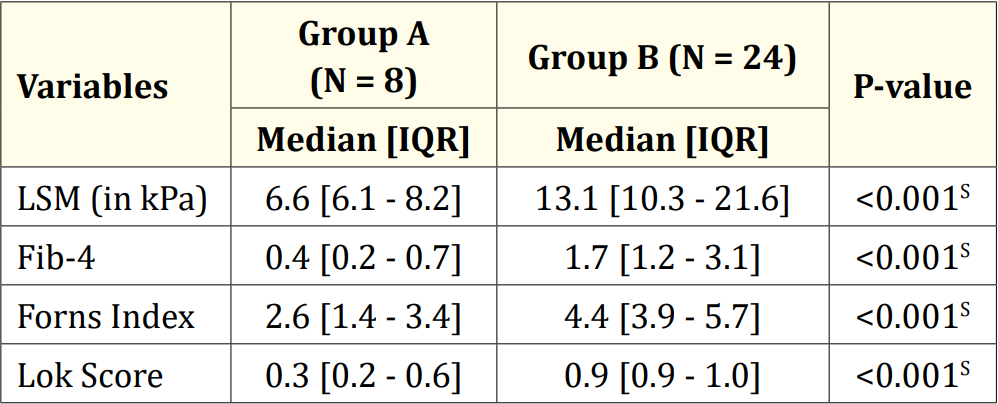
Table 5: Liver stiffness and serum fibrosis scores of the study population (N = 32).
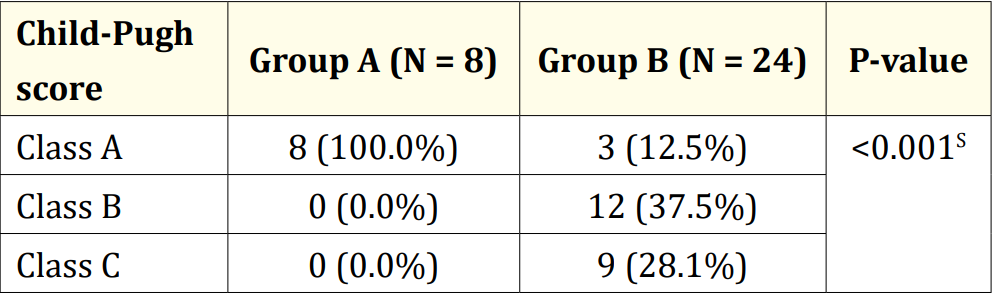
Table 6: Child-Pugh score of the study population (N = 32).
The research was carried out on 32 children who had been diagnosed with chronic liver disease (CLD) at the Department of Pediatric Gastroenterology and Nutrition, BSMMU, Dhaka, Bangladesh. Among this group of 32 patients, 24 (75.0%) were identified as having esophageal varices, while the remaining 8 (25.0%) did not exhibit esophageal varices. It was noted that esophageal varices were present in 71.4% of Bangladeshi children with CLD [19]. In a Canadian study by Gana., et al. (2011), 69% of the studied children were found to have esophageal varices. In contrast, a study conducted in Brazil by Fuguendes., et al. (2008) reported that 60% of children had esophageal varices during their first upper GI endoscopy. Among the 24 patients with esophageal varices in our study, 10 (41.7%) had large esophageal varices [20,21]. This aligns with findings from other studies, which also reported that 32% to 55% of children had large esophageal varices, supporting our current study’s results. It is worth noting that in our study, the majority of the children were male, and there was no significant statistical difference in gender distribution between children with or without esophageal varices (p = 0.378) [20,21]. Similar male predominance was observed in other studies [19,22], although Gana., et al. (2011) found a majority of female children in their study [20]. Another study found no gender difference in this regard [23]. The mean age of the children in our study was 10.7 ± 4.2 years. In a study by Rukunuzzaman (2015) that evaluated the clinical and laboratory profile of Wilson’s disease (WD) in children, the mean age of the children was 8.5 ± 4.5 years, while Alam., et al. (2019) observed a mean age of 9.7 ± 3.2 years in children with CLD, which is comparable to our study’s findings [19,22]. It is worth noting that consanguinity in marriage was observed in 5 patients, all belonging to Group B. Consanguinity in marriage is a feature of WD because it is an autosomal recessive condition. Rukunuzzaman (2015) found consanguinity in marriage in 30% of patients in their study [22], and Tryambak., et al. (2009) found WD to be more prevalent among children of consanguineous parents in Japan [24]. Regarding clinical manifestations, stigmata were present in 50.0% of patients without esophageal varices, whereas most patients (91.7%) with esophageal varices had stigmata. Among the patients with esophageal varices, 13 (54.2%) had clubbing, 6 (25.0%) had leuconychia, 8 (33.3%) exhibited thenar and hypothenar wasting, 2 (8.3%) had gynecomastia, and 6 (25.0%) had Palmar erythema. The prevalence of gynecomastia in cirrhotic adult patients has been reported in one study to be 44% [25]. Spider angioma was found in 33% of cases, and clubbing was observed in 24% of cirrhosis cases [26,27]. In Rukunuzzaman’s study (2015), thenar and hypothenar wasting were found in 8%, spider angioma in 2%, and clubbing and gynecomastia in 1% of cases each [22]. Spider angioma and gynecomastia are attributed to impaired estradiol metabolism in the liver [26], while clubbing develops due to the release of platelet-derived growth factors from aggregated platelets in the nail bed [27]. In both groups, 75.0% of patients had a palpable liver. However, the presence of a palpable spleen was significantly higher in children with esophageal varices (23 out of 24, 95.8%) compared to children without esophageal varices (2 out of 8, 25.0%) (p < 0.001). This finding is consistent with other studies [15,20,28]. Diagnoses among the patients in our study revealed that half were diagnosed with Wilson’s disease, 6 (18.8%) with Chronic hepatitis B, and 4 (12.5%) with Autoimmune hepatitis. Others had Cryptogenic cirrhosis (3 out of 32, 9.4%), Biliary cirrhosis (2 out of 32, 6.3%), and Glycogen storage disease (GSD) (1 out of 32, 3.1%). A prospective study by Alam., et al. (2019) reported that the predominant etiology of CLD was Wilson’s disease (65.5%), with other causes including chronic hepatitis B (6%), autoimmune hepatitis (7.1%), biliary atresia (6%), celiac disease-associated liver disease (1.2%), glycogen storage disease (1.2%), hepatitis C virus infection (1.2%), and cryptogenic (11.9%). The present study did not identify any patients with biliary atresia, which might be attributed to the small sample size of our study. Regarding laboratory parameters, there was no significant statistical difference between children with or without esophageal varices regarding median hemoglobin value (10.2 gm/dl vs. 12.5 gm/dl), which aligns with the findings of Alam., et al. (2019) [19]. However, the median platelet count of children without esophageal varices was significantly higher (315,000/µL) compared to children with esophageal varices (90,000/µL) (p < 0.001). A limited number of pediatric studies, as well as most adult studies, have shown similar results [19-21,29-31]. In a study by Fuguendes., et al. (2008) involving 85 children and adolescents with cirrhosis, patients with a platelet count <120,000/mm3 were found to be more prone to developing esophageal varices (p = 0.027) [21]. Another pediatric study from Brazil also identified a low platelet count as an independent predictor for the presence of esophageal varices, with high specificity (88.2%) and positive predictive value (PPV) (86.6%), consistent with our findings (specificity 95.6%, PPV 96.2%) for the presence of varices [32]. Gana., et al. (2011) also found a low platelet count (<115,000/mm3) in children with esophageal varices on a univariate model [20]. A recent pilot study in adults from India also indicated that a platelet count <150,000/ mm3 was the single best independent predictor of esophageal varices in newly diagnosed CLD, with high sensitivity (82.05%) and specificity (81.82%) [33]. The median bilirubin count of children without esophageal varices was significantly lower (1.3 gm/dl) compared to children with esophageal varices (2.7 gm/ dl) (p = 0.018). This is consistent with the findings of Fuguendes., et al. (2008) and Adami., et al. (2013) [21,28]. The Child-Pugh scoring system, designed to predict mortality in cirrhosis patients, classified all patients without esophageal varices as Class A, while among patients with esophageal varices, only 3 (12.5%) were classified as Class A. Class B and Class C were found in 12 (37.5%) and 9 (28.1%) patients, respectively. A highly significant difference was found between the groups regarding the Child-Pugh score (p < 0.001). This scoring system uses five clinical and laboratory criteria to categorize patients: serum bilirubin, serum albumin, ascites, neurological disorder, and prothrombin time [34]. Since all these parameters were significantly elevated in patients with esophageal varices, a significant difference in Child-Pugh scores between the groups was expected.
The limitations of the study titled “A Comparative Study on the Performance of Esophageal Varices in Pediatric Patients with CLD” include a relatively small sample size, potentially limiting the generalizability of findings. Additionally, the study’s retrospective nature may introduce bias and incomplete data. Long-term followup data might be limited, hindering the assessment of variceal progression over time. Furthermore, the study primarily focuses on pediatric patients, limiting the applicability of results to adult populations with CLD. These constraints should be considered when interpreting the study’s outcomes.
In conclusion, our comparative study on children with and without esophageal varices in the context of Chronic Liver Disease (CLD) has yielded valuable insights into the clinical management of this vulnerable population. Early detection and monitoring of esophageal varices in CLD children are crucial for timely intervention and prevention of potentially life-threatening complications. Additionally, our study underscores the importance of a multidisciplinary approach in caring for these patients, involving pediatric hepatologists, gastroenterologists, and radiologists, to ensure comprehensive assessment and management. We recommend further research to explore innovative diagnostic and therapeutic strategies to improve the quality of life and long-term outcomes for CLD children with esophageal varices.
No funding sources.
None declared.
The study was approved by the Institutional Ethics Committee.
Copyright: © 2023 Urmi Roy., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.