Djibril Boiro1*, Aminata Mbaye2, Amadou Sow1, Aliou Abdoulaye Ndongo3, Aurore Samira Ewagnignon1, Ndiogou Seck4, Idrissa Basse5, Ndeye Fatou Sow6, Lamine Thiam7 and Modou Gueye1
1 Abass Ndao Hospital Center, Cheikh Anta Diop University, Senegal
2 Albert Royer Children's Hospital, Cheikh Anta Diop University, Senegal
3 Pikine Hospital Center, Cheikh Anta Diop University, Senegal
4 Saint Louis Regional Hospital, Gaston Berger University, Senegal
5 Diamniadio Children's Hospital, Iba Der Thiam University, Senegal
6 Dalal Diam Hospital, Cheikh Anta Diop University, Senegal
7 Ziguinchor « La Paix » Hospital, Assane Seck University, Senegal
*Corresponding Author: Djibril Boiro, Abass Ndao Hospital Center, Cheikh Anta Diop University, Senegal.
Received: October 25, 2023; Published: November 09, 2023
Citation: Djibril Boiro., et al. “Type 1 Diabetes in Adolescents: About 207 Cases Monitored at the Abass Ndao Hospital Center in Dakar (Senegal)”. Acta Scientific Paediatrics 6.10 (2023): 01-06.
Introduction: T1D represents more than 90% of diabetes in children and adolescents. Adolescence is associated with an increase in insulin requirements which may contribute to the imbalance in T1D. The objective of our study was to describe the characteristics of type 1 diabetes in adolescents in our cohort in order to identify difficulties encountered.
Methods: This was a retrospective, descriptive study focusing on type 1 diabetic adolescents between 12 and 19 years old receiving insulin therapy in the pediatric department of CHAN, from April 2018 to December 2020. All patient files were collected and recorded on a questionnaire. The data were analyzed with Microsoft Office Excel 2019 software and its add-in XLSTAT 2022 version 3.1.1338.
Results: We collected 207 adolescents with type 1 diabetes. The average age was 15.43 ± 2.24 years and the sex ratio was 0.67.
The conventional intensified schedule of 3 injections per day was the most used (86.47%). The average daily insulin dose was 0.78 ± 0.26 IU/kg/day with extremes of 0.2 and 2.2 IU/kg/day. It was noted that 8.62% of patients remained without insulin for more than 30 days. 75.85% of patients practiced self-monitoring of blood sugar and 76.33% of patients were regularly monitored. During the 4 controls, the average glycated hemoglobin was greater than 9% in more than 60% of cases. The first reason for hospitalization was ketoacidosis (61.8%). Psychosocial impact was present in 14% of patients. We found a phobia of injections (38.46%) and weariness with regard to diabetes (30.76%). No deaths were reported in our study. 26.57% patients were lost to follow-up and 5 (2.41%) were transferred to adults.
Conclusion: Beyond the relative insulin resistance at this age, we must provide educational means to improve the quality of life and the prognosis of these patients by emphasizing compliance and self-monitoring of treatment.
Keywords: Adolescence; Type 1 Diabetes; Abass Ndao.
T1D: Type 1 Diabetes; NPH: Neutral Protamin Haegadorm; HbA1c: Glycated hemoglobin
It was estimated that 108,300 children under the age of 15 will be diagnosed in 2021, and that this figure will increase to 149,500 when the age range expands to those under 20. The incidence ratio among those aged 15-19 years compared to those aged 0-14 years was particularly high [1]. Adolescence is a period of transition characterized by a high rate of growth and significant psychological changes [2]. Their rapid physical growth and cognitive and psychological development have consequences for how they feel and how they think, make decisions, and interact with the world around them [2]. The increase in insulin requirements, the risk of weight gain and chronic hyperglycemia further increase this insulin resistance and contribute to the imbalance of T1D [3]. Without regular monitoring and appropriate management, it can develop into acute and chronic metabolic complications [4]. This constitutes one of the particularities of T1D in adolescents. It is an increasingly important public health problem globally among children [5].
In Senegal, insulin is free under the “Changing Diabetes in Children” (CDiC) project. Follow-up consultations for diabetic patients are done twice a week, however human resources remain insufficient [6].
The objective of our study was to describe the characteristics of type 1 diabetes in adolescents in our cohort in order to identify difficulties encountered.
This study was carried out in the Pediatrics department of the Abass Ndao Hospital Center (CHAN) in Dakar (Senegal), which is a public health establishment. This is a retrospective, descriptive study over a period of 2 years (April 2018 to December 2020). We included in our study all adolescents with type 1 diabetes, aged between 12 and 19 years. We did not include in our study: Adolescents with an incomplete file, or with less than one year of followup. The data was collected from the files and recorded on survey sheets pre-established for this purpose.
Therapeutic regimen was defined according to the number of injections and the type of insulin carrying out the conventional regimen (rapid insulin + NPH in 2 injections), the conventional intensified regimen (rapid insulin + NPH or rapid analogue + NPH or analogue rapid + slow analogue in 3 or 4 injections), the basal bolus scheme and the other schemes. Glycated hemoglobin was divided into 3 groups: less than 7% (balanced), 7 to 9% (moderately balanced), greater than 9% (poorly balanced). Four groups of glycated hemoglobin were reported corresponding to four measurements three months apart. The data were analyzed with Microsoft Office Excel 2019 software and its add-in XLSTAT 2022 version 3.1.1338.
In total, we collected 207 adolescents with type 1 diabetes during the study period.
The mean age was 15.43 ± 2.24 years. The extremes were 12 years and 19 years. The sex ratio was 0.67. The socio-economic level was considered low for 38.65% of the subjects. The majority of children were in school, i.e. 66.67%. Among them, 19 children (13.77%) were educated in a Koranic school and 119 in a French school (86.23%). For the latter, 51.26% had normal schooling and 48.74% had delayed schooling.
In our study, 72 (58.06%) adolescents girls had already had their periods. The mean age of menarche was 13.78 ± 1.56 years with extremes of 10 and 18 years and the median was 14 years. Among them, 4.17% had late menarche.
The mean age at diagnosis was 12.38 ± 3.41 years with extremes of 2 and 19 years. In 53.14% of cases, the discovery was made between 10 and 14 years of age. Ketoacidosis was the main mode of discovery of diabetes in our patients, i.e. 49.76%.
The 3 injections per day regimen was the most used with 86.47% followed by the 4 injections regimen (8.21%) and the 2 injections regimen (5.31%). The average daily dose was 0.78 ± 0.26 IU/kg/day with extremes of 0.2 and 2.2 IU/kg/day.
The notion of insulin skipping was found in 28.02% of patients. For 5 patients (8.62%), there was a delay of more than 30 days without insulin during their follow-up. There were 54 of our patients (26.09%) who practiced physical activity, with a duration of one hour per week in 50% of them.
In 51.21% of cases, patients snacked between meals. Lipodystrophies were observed in 22.22% of patients.
There was a linear correlation between insulin dosage and duration of diabetes.
In our study, 76.33% of patients were regularly followed up and 46.38% attended their appointments.
During the last 4 controls, the average glycated hemoglobin was greater than 9% in more than half of our patients, respectively for 65.52%, 68.97%, 58.62% and 68.97%. The mean HbA1C at diagnosis was 10.38 ± 1.38% (Figure 1).
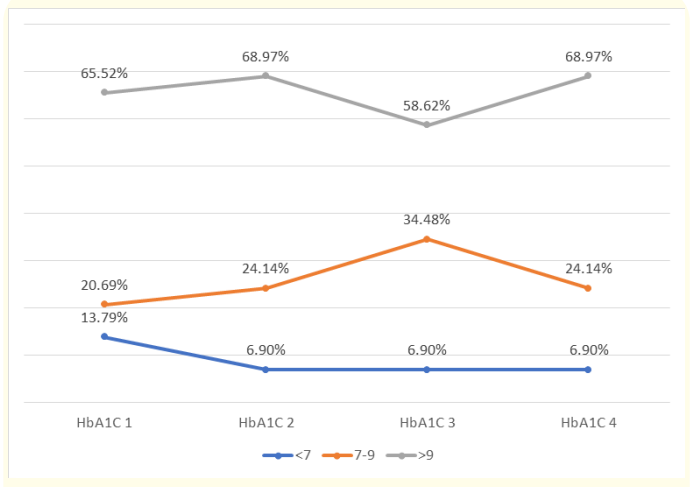
Figure 1: Change in average quarterly HbA1c levels during follow-up.
In 75.85% of cases, patients practiced self-monitoring of blood sugar levels. The monitoring log was available in 77 patients or 37.20%. There were 41.75% of patients who did 2 blood sugar checks per day and 15.98% who did 3 with 19.59% of our patients who did not control their blood sugar throughout the day.
In our study, 76.33% of patients were regularly followed up and 46.38% attended their appointments. We found that 91.14% were reviewed every three months.
124patients, i.e. 67.39%, presented acute metabolic complications such as ketoacidosis (72.58%) and hypoglycemia (5.65%).
In 1.93% of cases, patients presented with retinopathy. We found 0.92% neuropathy, 1.93% presented microalbuminuria and only 0.48% were at the nephropathy stage (Table 1).
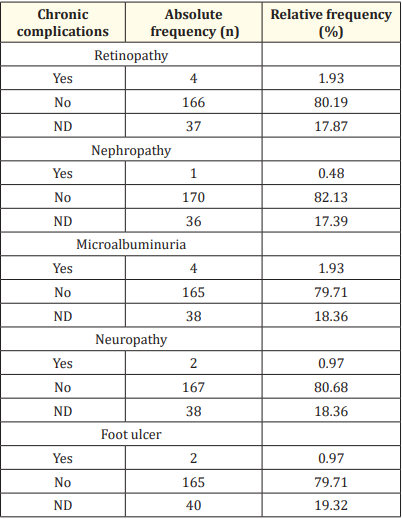
Table 1: Chronic complications of diabetes in adolescents.
Psychosocial impact was present in 14% of patients. There were notions of phobia of injections (38.46%) and weariness with regard to diabetes (30.76%). More than half were not informed (60.39%). No deaths were reported, 55 (26.57%) of patients were lost to follow-up and 5 patients (2.41%) were transferred to adults.
The average HbA1C in girls was 10.38% and that of boys was 11.47% (Figure 2). There was a statistically significant difference in glycated hemoglobin between the two groups with a p-value of 0.03.
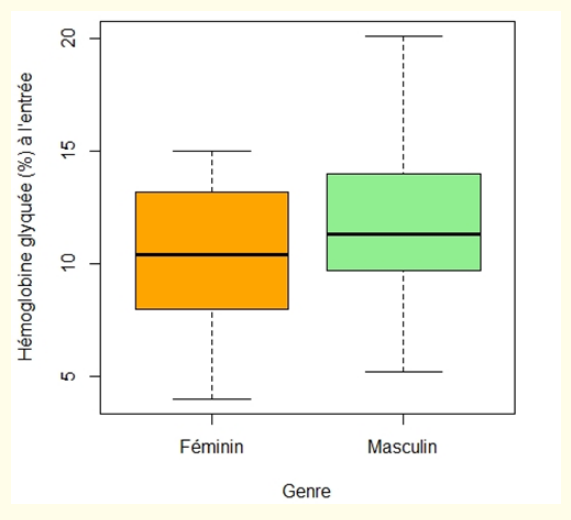
Figure 2: Mean glycated hemoglobin as a function of gender.
The average of glycated hemoglobin with self-monitoring was 10.59%, lower than that of the group without self-monitoring (11.78%) (Figure 3). This difference was statistically significant (p: 0.037).
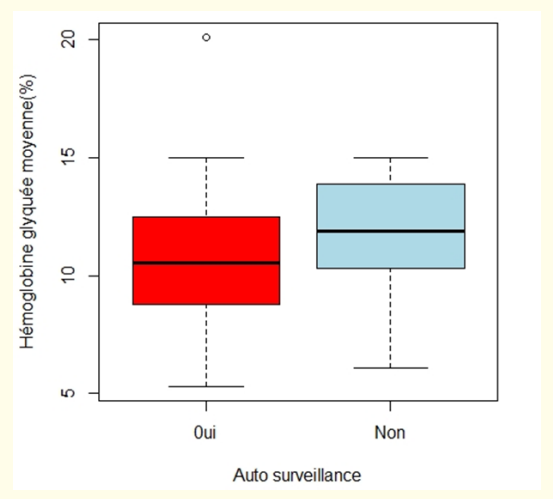
Figure 3: Average glycated hemoglobin according to self-monitoring practice.
There was no difference in mean glycated hemoglobin depending on insulin regimen (Figure 4).
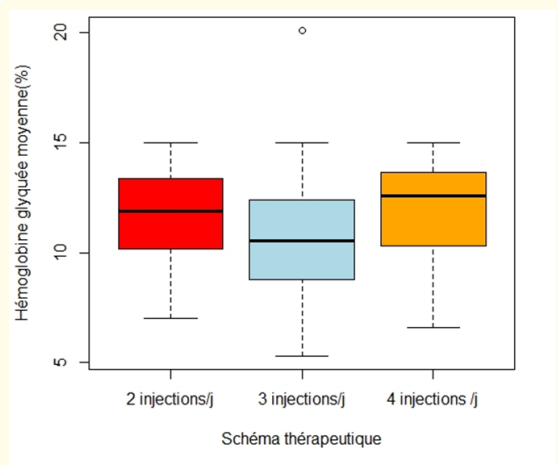
Figure 4: Average glycated hemoglobin according to the therapeutic regimen.
In the present study, we had 124 girls for 83 boys with a sex ratio of 0.67. Other authors reported that the predominance was female before and male during adolescence [7]. However, in the literature, there is no real difference in prevalence between the two sexes [8], which explains the discrepancies in results.
The majority of children were in school (66.67%). Some adolescents suffering from T1D have difficulty managing their diabetes alone at school, and abstain in order to avoid the stares of their peers so as not to feel different from others. Which can contribute to absenteeism or dropping out of school.
Poor diabetes control can stunt growth and delay puberty [9]. In our study, 0.97% of subjects had delayed puberty. The mean age of menarche was 13.78 ± 1.56 years in our study, with 4.17% having late menarche. Fagbèmi., et al. observed irregularity or even absence of menstruation in 53.6% and 3.6% of female subjects respectively [10].
The mean age at diagnosis was 12.38 ± 3.41 years. The discovery was made between 10 and 14 years of age and was following initial ketoacidosis (49.76%). Overall, similar data have been found in the literature [7,11]. However, in some studies we found a lower age of discovery of diabetes [8,12].
Ketoacidosis remains the most common discovery of T1D. It poses a real problem when we take into account the seriousness of this picture. Earlier diagnosis could help prevent this emergency from occurring by treating the signs of hyperglycemia very early.
Insulin therapy constitutes the cornerstone of treatment [13]. According to ISPAD, daily insulin requirements are around 0.6 to 1IU/kg/d in pre-puberty up to 2IU/kg/d in the pubertal period when requirements are increased [14]. In our study, the average daily dose was 0.78 ± 0.26 IU/kg/d, similar to that of Khamassi., et al. [15].
Insulin therapy can be used following several therapeutic regimens in order to obtain blood sugar levels as normal as possible, and to avoid complications linked to diabetes as much as possible, while maintaining the comfort of life for the diabetic. The 3 injections per day regimen was the most used. Elsewhere, Niang., et al. reported the use of the three injections per day regimen in 45.5% of cases [8].
The adolescent period is frequently marked by a glycemic imbalance and average glycated hemoglobin (HbA1c) rising from 8.1% at the age of 5 to 9.3% at the age of 15-18 [16]. There was a statistically significant difference in mean glycated hemoglobin depending on the existence or not of monitoring and according to gender with a higher mean HbA1C in boys. In the study by Aminou., et al. glycated hemoglobin was performed in 35% of patients with an average of 10.45 ± 3.2% (5.8-15%), similar to that of our series [11]. Khamassi., et al. in their study found glycated hemoglobin at 9.19 ± 2.39%; and only 27.7% of its patients reached the glycemic goals that were set in 2007 by the American Diabetes Association (ADA) [15].
In our study, 1.93% of patients presented retinopathy, 0.92% neuropathy, 1.93% microalbuminuria; and only 0.48% were at the stage of nephropathy and 0.92% of foot ulcer. In a previous study, prevalences of diabetic nephropathy and retinopathy were reported to be 50 and 20%, respectively. They were both linked to noncompliance with treatment [17].
Furthermore, 26.57%patients were lost to follow-up. The socioeconomic level was considered low for 38.65% of the subjects. In the literature, families who have a lot of socio-economic difficulties have a higher rate of loss to follow-up [10]. No deaths have been reported. This could be explained by the improvement in care through the implementation of the CDiC project with free insulin and better training of health personnel. Likewise, Fagbèmi., et al. explain the drop in mortality in their series by the improvement of care, thanks to a better understanding of the pathophysiology on the one hand and the application of standardized protocols on the other hand [10].
Adolescence is a period of transition characterized by a high rate of growth and significant psychological changes. Without regular monitoring and appropriate management, T1D can progress to acute and chronic metabolic complications. This situation also encourages school delays and sometimes dropping out of school. Even if there is relative insulin resistance at this age, we must provide educational means to improve the quality of life and the prognosis of these patients by emphasizing therapeutic compliance and self-monitoring of treatment.
No acknowledgements.
No conflict of interest for authors.
Copyright: © 2023 Djibril Boiro., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.