Shimaa Mohamed Reffat*
Department of Pediatrics, Cairo University, Faculty of Physical Therapy, Egypt
*Corresponding Author: Shimaa Mohamed Reffat, Department of Pediatrics, Cairo University, Faculty of Physical Therapy, Egypt.
Received: March 27, 2023; Published: June 28, 2023
Citation: Shimaa Mohamed Reffat. “Thera-Togs Orthotics Versus Reciprocal Electrotherapy on Postural Stability in Children With Cerebral Palsy: Randomized Controlled Trial”. Acta Scientific Paediatrics 6.7 (2023): 23-28.
Background and Objective: Cerebral palsy is the common motor disabilities due to a combination of deficiencies such as deficiency of muscle control, weakness, reduced balance and increase in muscle tone, all of which cause knee joint malalignment while standing and walking. This work aims to explore the impact of Thera togs to reciprocal electrical stimulation on postural stability in children with cerebral palsy.
Methods: A random sample of thirty participants had 6 to 8 years of age with cerebral palsy (boys and girls) were chosen. The participants were assigned into similar groups (I and II). The Biodex balancing system was used to measure over all stability indices before and after 12 weeks of treatment. Group I underwent reciprocal electro-therapy of the quadriceps (agonist) and the hamstring muscles (antagonist) on both sides. Group II received a Thera togs orthotic system with the same physical therapy programme as Group I.
Results: In children with spastic diplegic CP, both reciprocal electrical stimulation and Thera togs appear to produce a positive and statistically significant increase in postural stability metrics (P 0.05) reciprocal electrical stimulation, on the other hand, appears have a favourable and significant statistical effect than Thera togs.
Conclusion: In children with spastic-diplegic CP, reciprocal electrical stimulation significantly improved total postural stability indices compared to Thera-togs orthotic system. This experimental study was registered in the clinical trial registration: NCT05702632.
Keywords: Diplegic; Cerebral Palsy; Reciprocal Electrotherapy; Balance; Thera-Togs
Children with spastic diplegia who are standing may have difficulty initiating and timing muscular contractions, which affects their balance. Muscle weakness caused by inactivity may make this impairment worse. Postural reactions are all functional actions that are made more difficult by the decreased ability to balance while standing [1,2]. Training in balance regulation is crucial to the execution of most tasks and helps to recover from unanticipated postural disturbances [3].
It has been suggested that wearing TheraTogs orthotic clothing will increase one’s ability to stabilise his posture, rectify or prevent abnormalities, improve functionality, and give him access to a more suitable functional pattern [4]. According to a recent clinical investigation, children with CP who wore TheraTogs had dramatically improved gait patterns compared to those who did not [5].
For neuromuscular reeducation and improvement in performance, reciprocating electro-stimulation (RES) is a unique appliance of electro-therapy. Regarding reproducing normal muscle group firing sequences based on electro-myographic results obtained from healthy volunteers during exercise, RES differs from NMES. In order to simulate a voluntary movement pattern, the facilitation from a RES therapy is converted into a sequence that cause contraction of the quadriceps (agonist) muscle and the hamstring muscle (antagonist) [6]. One physiotherapy technique known as neuro-muscular electrical-stimulation (NMES) is frequently used to alleviate muscular stiffness [7], stimulate weak muscles, improve walking in a variety of neurological diseases including cerebral palsy (CP), boost circulation, and facilitate sensory perception [8].
Little research has been done comparing the two modalities, particularly reciprocal electrical stimulation and the Thera-Togs system, despite the support of the literature of the literature of the literature for their efficacy in the treatment of CP [9,10]. This study compared the impact of both treatment modalities ; RES and TheraTogs on the children with diplegic CP’s postural stability.
A random clinical trial was conducted from May 2022 to September 2022 at the Pediatric Outpatient Clinic. The parent of the child signed a written informed form, agreeing to participate and publish the results. This study was approved by the Faculty Ethics Committee No: P.T. REC/012/004393. Thirty participants with diplegic CP of both sexes were chosen to participate for the study based on estimates of the sample size. To assess age, diagnosis, inclusion, and exclusion criteria, they were originally tested and evaluated.
Children with diplegic cerebral palsy (CP) from ages of 6 to 8 years were involved if they had the following criteria: they could stand unassisted with their heels on the ground; they could follow commands and instructions during test and training; and the spasticity averaged from 1 to 1+ on the modified Ashworth scale (MAS) and according to the Gross Motor Function Classification System (GMFCS) their motor function levels ranged from grades I and II, participants with fixation malformations (bone or soft-tissue contractures) in both lower extremities or who had previous hamstring release surgery were excluded from the study. Children with skin disorders, allergic sensitivity toward tapes, contraindicated pacemakers with electrical stimulation, visual, hearing, or sensory impairments, and children with seizure disorders were all excluded from participation.
Participants were split into two group at random (I and II). Allocation for children were randomised and placed in sealed envelopes. Children were divided two groups at random: Group (I) underwent TheraTogs orthotic treatment along with conventional physical therapy, while group (II) received reciprocal electrical stimulation and a conservative physiotherapy training programme.
To enlist participants in the study, The spasticity degree was determined from the supine position by passive movement. According to the Modified Ashworth Scale (MAS), the children with spasticity grades from 1 to 1+ were included [11].
The GMFM was created to monitor variations over time in gross motor function of children. It is standardised, valid, and reliable. By time a child is five years old, they can typically complete every task in the GMFM with normal motor skills. Scale scoring: Each GMFM component received a four-point rating. The following is the scoring formula: 0 means the task is not started; 1 means it is started, but only to a 10% completion rate; 2 means it is partially completed, but 100% completed; and 3 means that the task is fully completed. The walking and standing criteria were used as the measuring variables of the study [12,13].
It is a posture training and evaluation system (Bio-dex Health software, Shirley, New York, USA). It includes safety support rails and a unstable leveling surface that can be adjusted to varying instability degrees. The system connects to a computer program that is displayed on the control panel display. It was used for evaluation. It is assess neuro-muscular coefficient and to maintain postural control on an unstable platform. Biodex comes with support rails, 12 levels of platform control, and a high resolution color touchscreen (12 is more stable and 1 is less stable).
Participants had to switch legs and control a pointed stance on a wobbly platform during the assessment and they could easily hold the center of the cursor while standing. They were instructed to control the leg place to the surface was secured. After the system was configured with foot angles and heel coordinates, testing began. Youth were told to focus their eyes on the visual screen in front , control hands off railings, and their arms at their sides. I was also instructed to get the sensor centered on the screen. The test lasted 30 seconds and the 3 results were averaged. Results were printed after completing test. Results were included total stability indices, anterior-posterior stability index, and medial-lateral stability index. The high scoring values indicate balance disturbances [14].
For group I, A specific programmable electrical stimulator was used (Uniphy, manufacturer Phyaction787; Uniphy, Eindhoven, The Netherlands). The equipment contains two of channels which can alternately (reciprocally) facilitate both opposite muscles [15].
The following settings were used in RES: (1) Asymmetric Biphasic Pulse Current is a current type. (2) pulse duration: 300 s (faradic) steadily increase but not reached maximal contraction, (3) frequency: 5–7 pulses per second (pps), eventually increase up to 30 pps. (4) Momentary for 10 seconds (5) 20 seconds off- time. (6) The treatment lasts 20 minutes. (7) The patient’s position is either supine, lying down or sitting up straight. (8) Electrode placement:
The following two channels, one on each side, were used:
The TheraTogs Harness for use with TheraTogs Group (II) children consists of a sleeveless vest and a pair of shorts with two thigh cuffs and extremities restraints. Wearing the Thera-Togs system directly on the skin under clothing provided unhindered toileting and breathability and comfortable latex on the torso and thighs. Children were not allowed to warred thera-togs with other patients due to infection control and fit issues [16].
Attached her theratogs using a top vest and strap technique often referred to as a hipster fit. First, the upper vest was adjusted properly to ensure that there were no tightness, discomfort, or circulation problems while the patient was standing. The constant extra- and proprioceptive feel of this top fit provides the important safety and stability, allowing them to regain postural stability and proper core orientation. Hip abduction strapping technique was used with the children in the fixed position and hip externally rotated to 5° abduction.
Then the outer thigh straps are brought together and his two bottom straps are attached to the thigh cuff to increase the vertical strength of the torso while preventing hip adduction, making all straps adjusted the length and position to achieve the effect. The upper straps supporting upper vest in the front and back [17,18].
It was neither annoying nor distracting because Thera-Togs undergarments; strapping systems were kept below their everyday routine. Before beginning, the participant get their thera-togs for one week with-out engaging in training, then increased the time they spent wearing them until it reached two hours each day [19,20]. This allowed the children to get used to the system.
Both groups engaged in a daily, 1-hour, 3-times-weekly physiotherapy treatment program for 3 consecutive months as follows: (1) reflex inhibiting patterns that suppress inappropriate reflexes, facilitate normal motor sequences and postural control, using reflex-suppressing patterns and key proximal and distal key point of control. (2) intensive core extension training to facilitate balance and postural stability; (3) Incline in a variety of forward, backward, and lateral positions while performing a variety of activities with the ball and balance board to promote upright and balanced reactions and improve your posture system. (4)Training saving reactions from a seated posture on a roll,, as well as by standing to encourage children to perform protective steps, forward; backward ; or sideways to gain equilibrium. (5) Stretching exercises to keep muscles that are prone to shortening long and elastic, as hip flexors, and adductors of both lower ; tendon -achilles, hamstrings, and upper extremities. (6) exercises to improve gait were crucial components of balance training and included the following:
Walking training on a stepper while moving sideways backward and forward within parallel bars at a large mirror. (b) Prepare outdoor walking by laying wedges and barriers with varying heights and diameters on the path of the walk. (c) Practice on a mat, floor, and carpets to walk on different surfaces (soft and rough surfaces) [21,22].
To carry out the exercise programme, various physical therapy items including tilting boards, wooden blocks, standing bars, parallel bar, steppers mats, wedges, rolls, medical balls, with considerable large mirrors were used.
To prevent error of type II, a analysis of power was conducted (power=0.8, =0.05, effect size=0.5), which led to a sample of 30 participants for this investigation. A versio 3.1 of G Power (Heinrich- Heine-Universität, Düsseldorf, Germany) was used to establish the size of sample.
The data were presented in the form of average and standard deviation (SD). A combination t test was used to compare the mean of all parameters measured before and immediately after treatment for each group, and an unpaired combination test was used to compare two groups before and immediately after treatment. Comparisons of data scores are normally distributed, which has been confirmed by the Shapiro-Wilk test. The significance level was set to alpha 0.05. The static analysis was performed using version 20 of SPSS software (SPSS Inc., IBM, Chicago, IL, USA).
The baseline characteristics of children were tabulated in table 1. The RES with Thera-togs group were comparable in variables of sex, age, weight, height, spa- ticity, and GMFCS-levels.
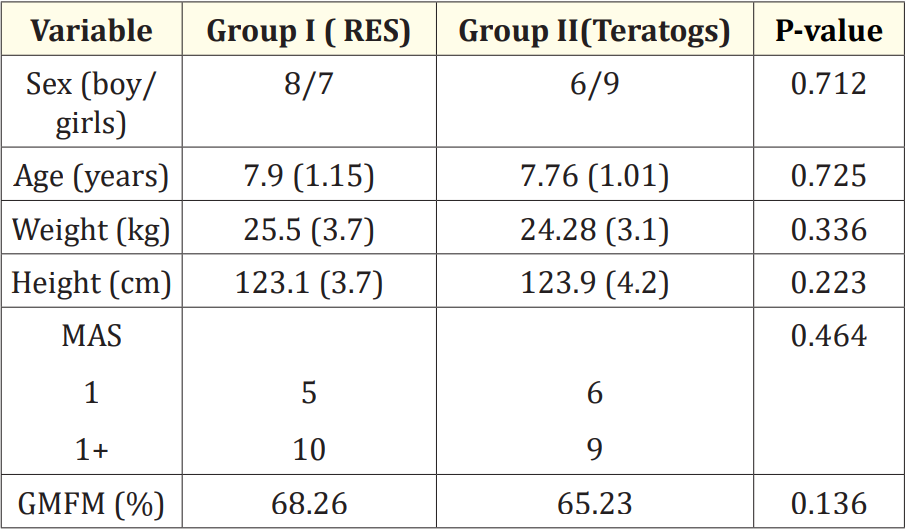
Table 1: Baseline characteristics of the children.
Measures were tabulated as mean +_Standard deviation., MAS;
Modified Ashawar Scale, GMFM; Gross Motor Function Measure.
Prior to treatment, there were no significant statistica differences in the average postural stability index (p > 0.05) between the RES and TheraTogs groups. In both groups, the average postural stability index from baseline and posttreatment assessment was significant statistically (P < 0.05). As shown in table 2, the RES group significantly improved postural stability compared to the TheraTogs group.
Mobility is often hampered by spasticity, particularly when walking. CP Children often experience a reduction in gait distance and an increase in falling due to antagonist and agonist weak contraction with poor motor control [23].
Mean values before treatment of the variables evaluated evaluated for the two groups showed that those children had standing and walking postural impairment. According to Woollacott and Shumway-Cook [24], children with spastic diplegic CP exhibit the following behaviours: crouching posture, which contributes to a decreased ability to recover balance; inappropriate muscle action; and cocontraction of agonists-antagonists.
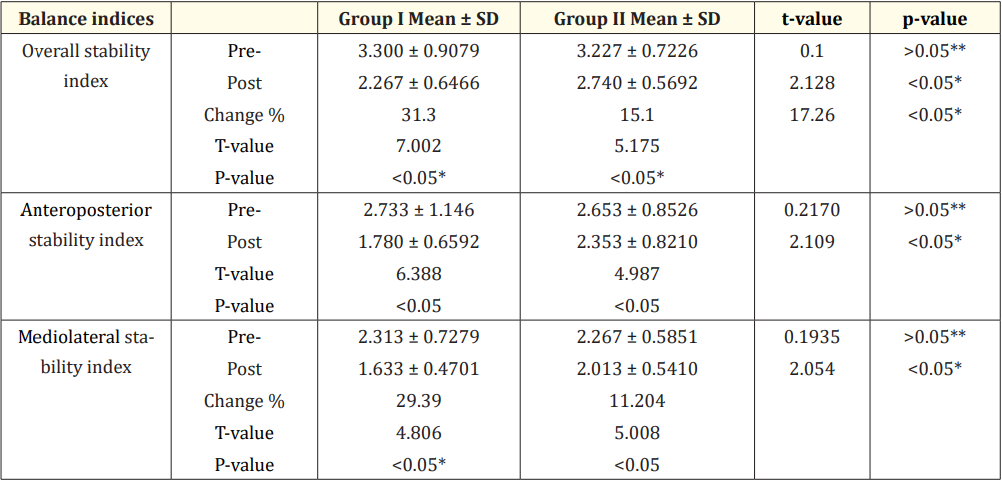
Table 2: Average mean values pre and post treatment of overall balance indices within each group and between groups.
Significance level at P < 0.05. *Significant. **Nonsignificant.
According to Sterba., et al. [25] focused on promoting postural and balance responses and adjusting posture when performing basic task as sitting and walking as a component of a physiotherapy plan for therapists rehabilitating child with neuro-logical disorders. It was recommended that the treatment be targeted and resulted in significant improvement in follow-up studies. Group I support their recommendations. Correspondingly, control of postural requires the ability to respond to changing activities and circumstances needs. This is because mutual electrical stimulation facilitates the precise sensory and motor challenges. There are several operation patterns, and it is necessary to be able to select the optimum one according to the situation and environment.
The impact of RES on quadriceps and hamstring muscles may be responsible for the improvement in the mean after treatment of group I. This is in line with the findings of Daichman., et al. [26], found that an alternative NMES programme for quadriceps muscles dramatically reduced hamstring spasticity in conjunction to facilitation of quadriceps and improvements in temporal spatial gait metrics. Gradual response between agonists (quadriceps) and antagonists (hamstrings) is made possible by activating the reciprocal inhibition mechanism [27].
Proprioceptive stimulation and decreased muscle length induced by the TheraTogs harness system were used. This enables the movement with hip abductors and extensors, enables normal firing and recruitment mechanisms in these muscles, increases the production of force and improves the static and dynamic balance of the body.
Additionally, the spastic hip internal rotators and adductor muscles were reflexively inhibited when the afflicted leg was placed in external rotation and abduction utilising the TheraTogs strapping device. This allowed for normal antagonistic muscular activity [4].
In the current investigation, it was evident that the physical therapy programme that was added to the treatment plan enhanced the results. After three months of intervention, the variables of postural stability increased.
The small sample of children in two groups reduced the statistical power and made it not easy to find conclusions about significant effects. The absence of a third group to evaluate the effectiveness of the physiotherapy programme as intended lonely; to lessen impact of spasticity, the study was conducted conducted only on children with grade 1 and 1+ MAS.
The results of this study indicated that; reciprocal electrostimulation is noticeably had a significant effect than Thera Togs strapping systems in enhancing stability of posture in CP children.
There is no conflict of interest in this study.
Applicable.
I want to thank the parents and their children who took part in the research for their cooperation and for all staff and managers of the Department for their the support.
Copyright: © 2023 Shimaa Mohamed Reffat. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.