Hasan Mahmud Rumi1*, Syed Shafi Ahmed2, Salahuddin Mahmud3, Sohely Akter4 and Muhammed Nurul Islam Shikdar5
1 MD (Paediatrics), Assistant Professor, Department of Paediatrics, Tairunnessa Memorial Medical College and Hospital, Bangladesh
2 PhD Professor and Head, Department of Paediatric Gastroenterology, Hepatology and Nutrition, Bangladesh Shishu Hospital and Institute, Bangladesh
3 MD (Paediatrics), Associate Professor, Department of Paediatric Gastroenterology, Hepatology and Nutrition, Bangladesh Shishu Hospital and Institute, Bangladesh
4 Assistant Professor (CC), Department of Paediatrics, Tairunnessa Memorial Medical College and Hospital, Bangladesh
5 Assistant Professor, Department of Paediatrics, Aichi Medical College, Bangladesh
*Corresponding Author: Hasan Mahmud Rumi, MD (Paediatrics), Assistant Professor, Department of Paediatrics, Tairunnessa Memorial Medical College and Hospital, Bangladesh.
Received: June 13, 2023; Published: June 22, 2023
Citation: Hasan Mahmud Rumi., et al. “Accuracy of Ultrasonography and Hepatobiliary Scintigraphy for the Diagnosis of Biopsy Proven Biliary Atresia”. Acta Scientific Paediatrics 6.7 (2023): 17-22.
Background: Optimizing outcomes in biliary atresia (BA) requires timely diagnosis. Despite early hepaticoportoenterostomy, BA has still been the most common indication for paediatric liver transplantation. So early diagnosis is extremely important for management. Ultrasonography and hepatobiliary scintigraphy are two major diagnostic methods for the diagnosis of biliary atresia.
Aim of the Study: To determine the accuracy of ultrasonography and hepatobiliary scintigraphy for the diagnosis of biliary atresia.
Material and Methods: The present study was a cross-sectional observational conducted in the Department of Pediatric Gastroenterology, Hematology and Nutrition, Dhaka Shishu (Children) Hospital, Dhaka City from March 2018 to August 2019. Data were processed and analyzed using computer software SPSS statistical package, version 23 (SPSS Inc., Chicago, IL, USA) for Windows XP. Data were expressed as numbers and percentages for qualitative variables and median range (minimum and maximum) for quantitative variables. To compare categorical variables between groups of patients with neonatal cholestasis, the chi-square (χ2) test or Fisher’s exact test was used. Fisher’s exact test was used instead of the χ2-test when the expected value in any one contingency cell was ≤5. Student t-test was used for continuous variables. Validity tests were done for ultrasonography and hepatobiliary scintigraphy with liver biopsy confirmed biliary atresia. A p-value < 0.05 was considered to be statistically significant in all the analyses.
Results: Ultrasonography, hepatobiliary scintigraphy and liver biopsy findings of 50 neonatal cholestasis cases were studied where Hepatobiliary scintigraphy had the highest sensitivity of 90.5% but low specificity of 44.8%. The sensitivity and specificity of USG for the diagnosis of BA were found to be 81.0% and 65.5% respectively in this study. Diagnostic accuracy of USG and hepatobiliary scintigraphy for diagnosis of BA was 72.0% and 64.0% respectively.
Conclusion: This study showed that hepatobiliary scintigraphy had high sensitivity but low specificity for diagnosing biliary atresia. The diagnostic accuracy of ultrasonography is more than hepatobiliary scintigraphy for diagnosing biliary atresia.
Keywords: Biliary Atresia; Ultrasonography; Hepatobiliary Scintigraphy; Diagnostic Accuracy
Neonatal cholestasis is defined as conjugated hyperbilirubinemia occurring in the newborn as a consequence of diminished bile flow. Conjugated hyperbilirubinemia in a neonate is defined as a serum direct/conjugated bilirubin concentration greater than 1.0 mg/ dL if the total serum bilirubin (TSB) is <5.0 mg/dL or greater than 20% of TSB if the TSB is >5.0 mg/dL. Jaundice in newborns is most common physiological or due to ABO/Rh hemolytic incompatibility. However, if jaundice is associated with dark urine and/or pale stools, it is suggestive of cholestasis. Cholestasis results from structural and functional impairment of the hepatobiliary system, which is often the target of several environmental factors and disease processes [1]. Cholestasis jaundice affects approximately 1 in every 2,500 infants and has a multitude of causes [2]. Biliary atresia (BA) is an idiopathic inflammatory process involving the bile ducts resulting in obstruction of the biliary tract, chronic cholestasis, progressive fibrosis, and eventually biliary cirrhosis [3]. The number of investigations involving diagnostic evaluation of infantile cholestasis, such as biochemical tests, ultrasonography, hepatobiliary scintigraphy (DISIDA scan), and liver biopsy are basically used, but no such single test can differentiate BA from NH unless performing intraoperative cholangiography which is considered as a gold standard diagnosis and is invasive. Investigators, therefore, have continued to find a new reliable, rapid and noninvasive diagnostic tool for BA [4]. Numerous ultrasonography (US) features have been described as useful pointers for the diagnosis of BA. Abnormalities in the shape and wall of the gallbladder have, for experienced operators, yielded sensitivities and specificities of more than 90% in the diagnosis of BA [5]. The triangular cord (TC) sign, a focal area of increased echogenicity anterior to the bifurcation of the portal vein representing the fibrotic remnant of the extrahepatic biliary tree in BA, has been considered an important diagnostic feature by some [6]. Other groups have suggested that a combination of three gallbladder features namely, length less than 19 mm, an irregular wall, and an indistinct mucosal lining (the so-called gallbladder ghost triad) is diagnostic. In addition to these US features, BA may be associated with other congenital structural anomalies that are detectable in the US [7]. For example, in the BA splenic malformation syndrome, BA can be associated with polysplenia, an interrupted inferior vena cava and other cardiovascular anomalies [8]. Furthermore, infants with BA typically have a degree of hepatic fibrosis or cirrhosis, and the majorities have some evidence of portal hypertension as early as 8 weeks of age [9]. Hypertrophy of the right hepatic artery has also been reported in infants with BA [10]. The absence of a common bile duct (CBD), enlargement of the hepatic artery (HA), and the identification of hepatic subscapular flow (HSF) have also been considered useful for diagnosing biliary atresia [11].
This perspective Cross-sectional study was conducted at the Department of Pediatric Gastroenterology, Hematology& Nutrition, Dhaka Shishu (Children) Hospital, Dhaka, Bangladesh in the period from March 2018 to August 2019.50 patients were selected purposively from infants presenting with cholestasis jaundice admitted into Dhaka Shishu (Children) Hospital seeking medical care. Ultrasonography was performed in all the cases before the liver biopsy. Ultrasonography (USG) of the hepatobiliary system (HBS) was done after 4 hours of fasting and repeats after half an hour of feed. It was interpreted by a single radiologist of Dhaka Shishu Hospital with experience in pediatric liver disease. The absence of gallbladder after fasting, lack of contraction after a meal, and presence of triangular cord sign were taken as USG evidence of BA diagnosis. Hepatobiliary scintigraphy (HIDA scan) was done at the Institute of Nuclear Medicine, Bangabandhu Sheikh Mujib Medical University after administration of phenobarbitone (5 mg/ kg/day orally in two divided doses for at least 5 days). In patients with no intestinal tracer excretion detected even after 24 hrs. was considered biliary atresia. Before performing a liver biopsy, baseline investigations were done. A True-cut biopsy needle was used. Specimen of liver tissue was preserved in formalin and sent for histopathology. It was interpreted by a single pathologist of Dhaka Shishu Hospital with experience in pediatric liver disease. The Histological parameters like ductular proliferation, prominent bile plug, and marked portal fibrosis were considered diagnostic features for BA. The features considered for NH were disruption of normal liver architecture, chronic inflammatory cell infiltration, and giant cell transformation. If paucity of the interlobular biliary tract was found considered intrahepatic bile duct paucity.
Table 1 showed the studied subjects most of the cases 11(52.4%) and 15(51.7%) were ≤2 months of age in BA and non-BA groups respectively but there was no significant difference between the two groups. Table 2 is a Comparison of the sex distribution of the studied subjects in the BA group female (81.0%) were predominant and non-BA group males (58.6%) were predominant and that was statistically significant (p < 0.05). Table 3 is a Comparison of clinical symptoms of the studied subjects presenting history and clinical characteristics compared between BA and non-BA cases. Most of the infants (19, 90.5%) of BA were term while pre-term babies (28, 96.6%) in the case of non-BA cases were statistically significant (p 0.023). The presence of persistently pale-coloured stool was more commonly seen in patients with BA (BA vs. nonBA: 90.5% vs. 13.8%). The difference was statistically significant (p 0.001). Table 4 showed that of the studied subjects 21(42.0%) cases were diagnosed with biliary atresia, 27(54.0%) were diagnosed with neonatal hepatitis and 2 cases were intrahepatic bile duct paucity by liver biopsy. Liver biopsy findings were ductular proliferation, prominent bile plug, marked portal fibrosis in biliary atresia cases and disruption of normal liver architecture, chronic inflammatory cell infiltration, and giant cell transformation in neonatal hepatitis cases. The paucity of the interlobular biliary tract indicates intrahepatic bile duct paucity. Sensitivity, specificity, positive and negative predictive values of the USG and hepatobiliary scintigraphy for diagnosis of BA. Table 5 showed that, diagnostic usefulness of USG and hepatobiliary scintigraphy in the order of accuracy for the diagnosis of BA. Hepatobiliary scintigraphy had the highest sensitivity of 90.5% but low specificity of 44.8%. The sensitivity and specificity of USG for the diagnosis of BA were found to be 81.0% and 65.5% respectively in this study. Diagnostic accuracy of USG and hepatobiliary scintigraphy for diagnosis of BA was 72.0% and 64.0% respectively.
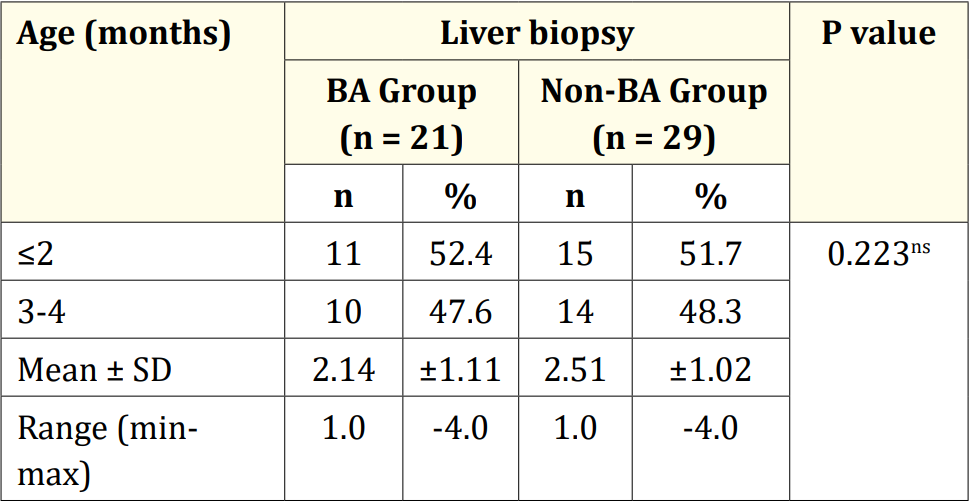
Table 1: Comparison of the age distribution of the studied subjects (n = 50).
ns = not significant and the P-value reached from unpaired t-test.
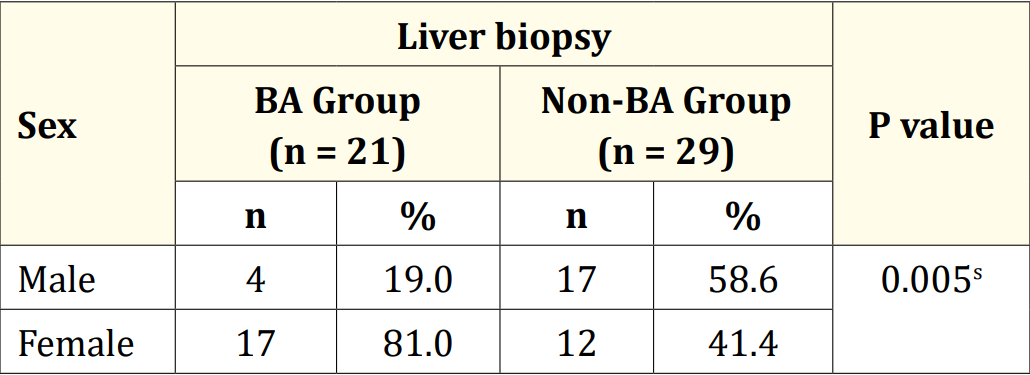
Table 2: Comparison of sex distribution of the studied subjects (n = 50).
s = significant and P value reached from Fisher exact test.

Table 3: Comparison of clinical symptoms of the studied subjects(n = 50).
s = significant, ns = not significant and P-value reached from the Fisher exact test.

Table 4: Liver biopsy findings in the studied subjects (n = 50).
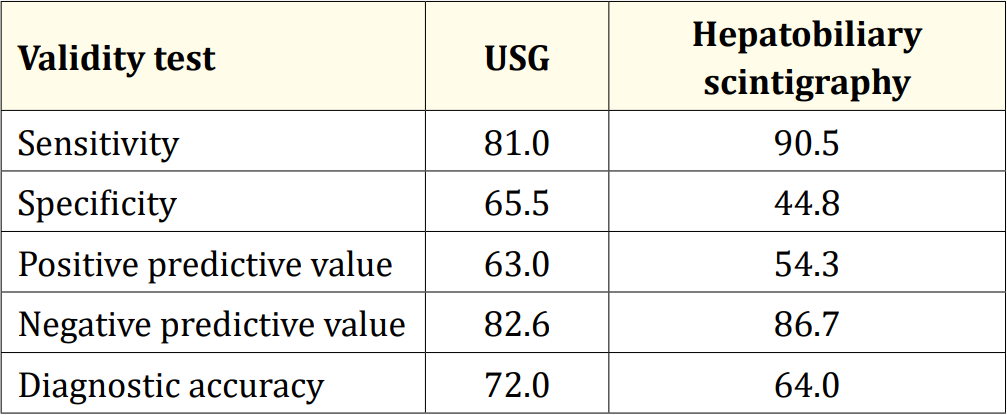
Table 5: Sensitivity, specificity, positive and negative predictive values of the USG and hepatobiliary scintigraphy diagnosis evaluation for the diagnosis of BA.
The study was carried out at the Department of Pediatric Gastroenterology, Hematology& Nutrition, Dhaka Shishu (Children) Hospital, Dhaka, Bangladesh, from March 2018 to August 2019. Ultrasonography, hepatobiliary scintigraphy and liver biopsy findings of 50 neonatal cholestasis cases were studied. A total of 50 cases were diagnosed by liver biopsy among them 21(42.0%) were biliary atresia (BA) and 29(58.0%) were non-BA. Hepatobiliary scintigraphy had the highest sensitivity of 90.5% but low specificity of 44.8%. The sensitivity and specificity of USG for the diagnosis of BA were found to be 81.0% and 65.5% respectively in this study. Diagnostic accuracy of USG and hepatobiliary scintigraphy for diagnosis of BA was 72.0% and 64.0% respectively. In a study by Sultana., et al. 19 cases were biliary atresia and 17 were nonbiliary atresia [12]. Ultrasonography is simple, readily available, and non-invasive, at affordable cost and is free of radiation. It is useful for visualizing biliary tract anatomy and excluding other causes of prolonged jaundice such as choledochal cysts and hence recommended as an initial investigation for the evaluation of infants with cholestasis of unknown etiology [13]. Most reviews report the sensitivity of hepatic-biliary scintigraphy for the diagnosis of BA between 97-100% and the specificity from 33-91% [14,15]. HBS had an accuracy of 64.0% in this study, which is comparable to the data higher [4,16-18]. Poddar., et al. reported the accuracy of various clinical and investigational parameters to differentiate biliary atresia (BA) from neonatal hepatitis (NH) [19]. A total of 101 infants with neonatal cholestasis (NCS) were included in that study. Persistently clay stool was found to have modest accuracy (79%) and the accuracy of HBS improved significantly following UDCA therapy (91% from 77%, p <0.01) whereas liver biopsy was 100% accurate in differentiating BA from NH. In another study, a sensitivity of 90%, a specificity of 92.4%, a positive predictive value of 75.3%, a negative predictive value of 97.3% and an accuracy rate of 91.9% was observed for an ultrasound of the gall bladder in the identification of biliary atresia [5]. Meanwhile, in the study of Rastogi., et al. among the 49 adequate liver biopsies, the sensitivity and specificity of percutaneous liver biopsies for diagnosing BA was 88.2% each [20]. Percutaneous liver biopsy is highly accurate (88.2%) in diagnosing BA in developing countries. This investigation should be done to decrease the frequency of negative laparotomy and to achieve cost–benefit with reduced morbidity. In a study done by Lee., et al. the common clinical features at presentation were jaundice (100%), hepatomegaly (95%), splenomegaly (52%) and pale stools (47%) [21]. Three clinical features were noted to be sensitive for BA (sensitivity of 77%, 80% and 94%, respectively), but the corresponding specificity was poor (51%, 65% and 39%, respectively). But they did not find any single clinical feature with sufficient sensitivity and specificity to differentiate BA from other causes of NC. Yang., et al. also compared the accuracy, sensitivity, specificity, and predictive values of these various methods [22]. The accuracy of HBS SPECT was higher than that of MRCP, HBS, and US in this study. Also, there were no significant differences in diagnostic accuracy among MRCP, HBS, and US.
This was a cross-sectional observational study selected from one selected hospital in Dhaka city with a small sample size which is the main limitation of this study. Also, it was conducted in a very short period.
This study showed that hepatobiliary scintigraphy had high sensitivity but low specificity for diagnosing biliary atresia. The diagnostic accuracy of ultrasonography is more than hepatobiliary scintigraphy for diagnosing biliary atresia. A correlation between clinical, biochemical assessment, scintigraphy and sonographer is important to arrive at a timely diagnosis for appropriate management. Further study with a larger sample size is necessary to find out a test with better accuracy to diagnose BA.
Copyright: © 2023 Hasan Mahmud Rumi., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.