Chiraz Regaieg1,3*, Ben thabet Afef1,3, Kolsi Nadia1,3, Amira Trigui2,3, Bouraoui Amira1,3, BEN HAMED Amel1,3, Manel Charfi1,3 and Hmida Nedia4
1 Department of Neonatology, Hedi Chaker University Hospital, University of Sfax, Sfax, Tunisia
2 Department of Ophtalmology, Habib Bourguiba University Hospital, University of Sfax, Sfax, Tunisia
3 University of Medicine of Sfax, Sfax, Tunisia
*Corresponding Author: Chiraz Regaieg, Department of Neonatology, Hedi Chaker University Hospital, University of Sfax, Sfax, Tunisia.
Received: January 20, 2023; Published: February 12, 2023
Citation: Chiraz Regaieg., et al. “Retinopathy of Prematurity: Findings After 15 Years of Screening in a Neonatal Care Unit in Tunisia”. Acta Scientific Paediatrics 6.3 (2023): 16-20.
Background: Retinopathy of prematurity (ROP) is the leading avoidable cause of childhood blindness. It is an abnormal retinal vascular development in preterm, due to several risks’ factors.
Objectives: To evaluate the results of the screening program for ROP in the neonatal care unit of Sfax.
Methods: A retrospective study of all cases of ROP screened in the neonatal intensive care unit of Sfax (Tunisia) between January 2005 and December 2020. The screening program included all preterm under 32 weeks of gestation (GW) and/or having a birth weigh less than 1500 grams and all preterm under 34 GW with one of ROP risk factors.
Results: During the study period, 3644 newborns were examined for ROP at the age of 30 days (with an average of 243 exams/year). Twelve cases of ROP were diagnosed which 5 in 2005. The incidence was 0,22% of newborns at risk. The ROP was Stage V in 5 cases, Stage III in 3 cases, Stage II in 2 cases and Stage I in 2 cases. One of the stages III ROP cases progressed to a stage IV and another to a stage V due to a delay in treatment. The mean term was 30 weeks + 3 days [26-33 GW]. The mean weight was 1425 grams [970-2050 gr]. All newborns were hospitalized for neonatal respiratory distress syndrome. Seven required mechanical ventilation which was associated to exogenous surfactant administration in 6 cases. The mean duration of oxygen therapy was 12 days [2-57 days]. Severe sepsis associated to hemodynamic disorders were observed in 7 patients. The treatment was surgical in stage IV ROP. It was based on cryotherapy in stage III and stage II ROP. Stage I ROP was treated successfully by argon laser photocoagulation. For stage V ROP cases no treatment was proposed given the definitive vision loss.
Conclusion: The incidence of ROP in our unit decreased since the renovation of the department in 2006, with the generalization of cardiorespiratory monitoring and the acquisition of a blood gas measuring device allowing the measurement and control of oxygen therapy. Furthermore, the screening enables an early diagnosis and management, which improve the prognosis. Screening can be improved by using new technologies especially the Ret-cam.
Keywords: Screening; Retinopathy; Premature; Risk Factors.
ROP: Retinopathy of the Prematurity; GW: Weeks of Gestation;CPAP: Continuous Positive Airway Pressure
Retinopathy of the prematurity (ROP) is a complication of prematurity. The incidence increases with the survival of extremely premature newborns especially in developed countries. It is a leading curable cause of childhood blindness worldwide (6 to 20% of childhood blindness) [1]. An effective screening of this pathology improves its outcome. In our unit we started screening for retinopathy of the prematurity in year 2005. The aim of our study is to evaluate the results of our screening program after 15 years of screening program.
This study was a retrospective review of the medical records of premature infant who were examined for retinopathy of prematurity and were born between January 2005 and December 2020. The screening concerned
These selection criteria were revised in year 2008 and since screening concerned
The fundus exam was performed by a single voluntary ophthalmologist at an average of seven exam/weeks.
During the study period, the screening for retinopathy of prematurity had concerned 3644 surviving newborns at risk, which makes an average of 243 newborn at risk/year. Twelve infants had developed a retinopathy of prematurity given an incidence of 0, 22% of newborns at risk. Among these infants, five were diagnosed in year 2005 (Figure 1).

Figure 1: Distribution of the newborns with retinopathy of the prematurity (ROP) by year.
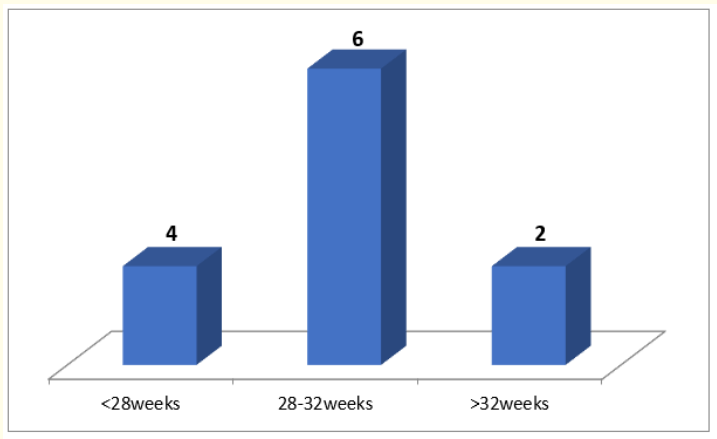
Figure 2: Distribution of the newborns with retinopathy of the prematurity according to their gestational age.
Mean gestational age was 30 weeks of gestation (GW) + 3 days (extremes: 26 to 33 GW) (figure 2). Mean birth weight was 1425 grams (extremes: 970 to 2050 grams). Of these 12 infants, 8 were male. Six were multiple births: all twins. Only one twin of each pregnancy had retinopathy of prematurity.
Maternal preeclampsia was present in two cases and a premature rupture of membranes in three other cases. Corticosteroids for lung maturation were administrated to only 7 mothers.
Delivery was vaginal in 4 cases. The APGAR score at the first minute of life was ≤ 7 in five cases requiring resuscitation in the delivery room.
All newborns were hospitalized for respiratory distress. Seven had required artificial ventilation and six surfactant administrations. Mean duration of artificial ventilation was 8,4 days and it exceeded 5 days in 4 cases. The mean duration of oxygen therapy was 12 days and it exceeded 5 days in 9 cases. Severe or repeated apnea was present in five cases. Seven newborns had developed a severe sepsis associated to hemodynamic disorders. Blood transfusion was given to four infants. Seven newborns had developed a nosocomial infection and three babies had developed an intraventricular hemorrhage.
The mean delay diagnosis was 10 weeks (4 to 21 weeks). The retinopathy of prematurity was classified stage V in five cases which three were included in 2005, one in 2012 and a other in 2017. In fact, the diagnosis was late was late at stage V for these last two newborns because they were rehospitalized several times in a pediatric intensive care for severe bronchiolitis.
The ROP was stage III in 3 cases, stage II in 2 cases and stage I in 2 cases. One of the stage III ROP cases progressed to a stage IV and another to a stage V (case in 2020) due due to a delay in treatment because of the confinement during the COVID 19 pandemic.
For stage V ROP cases no treatment was proposed given the definitive vision loss. The stage I ROP was treated successfully with argon laser photocoagulation. The treatment was surgical in stage IV ROP. It was based on cryotherapy in stage III and stage II ROP. Cryotherapy was unsuccessful for a stage III ROP and a vitrectomy dissection was indicated. The remaining infants (stage IV and stage III ROP) were treated unsuccessfully with surgery. Lesions worsened for the stage III and IV ROP as management was delayed (men delay treatment after diagnosis was 9 weeks (1 to 32 weeks)). Thus, the outcome was blindness for 6 infants and impaired vision for 2 infants.
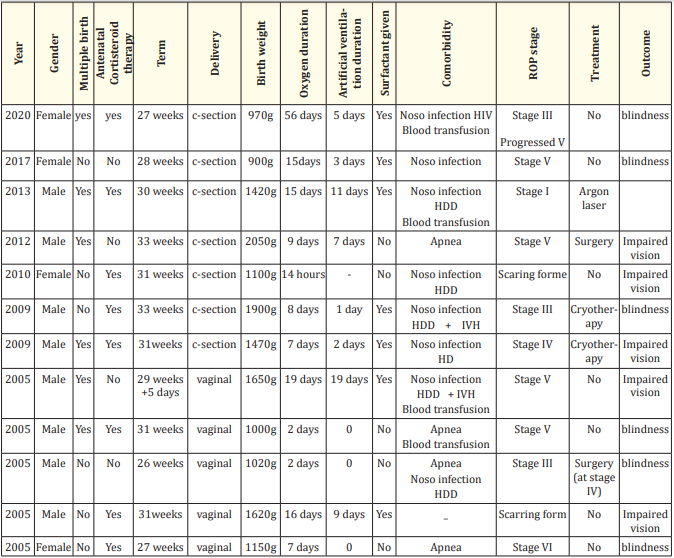
Table 1: Characteristics of the twelve cases of retinopathy of prematurity.
ROP: Retinopathy of Prematurity; c-section: Caesarean Section; Noso Infection: Nosocomial Infection;
HDD: Hemodynamic Disorders; IVH: Intraventricular Hemorrhage
The incidence of retinopathy of prematurity is increasing with the improvement of neonatal care as well as the increase of premature and low-birth weight infant survival rates. The reported findings concerning the incidence of ROP and its severity are varying and even controversial. Indeed, many factors can influence the study’s results: the development level of the unit, the survival rate of premature and low-birth infant, the existence or not of an effective screening and treatment program, the type of the study and the considered criteria (gestational age, the ROP stage…). This makes findings hardly comparable. In our unit global incidence were 0,22%. The reported incidence of ROP varies from 0,17% (global incidence) to 89% (incidence in newborns with gestational age < 27 WG) [1-5]. In a Turkish study similar to ours, managed in a tertiary neonatal intensive care unit, on a population of 330 preterm gestational age ≤ 34 weeks screened between September 2005 and July 2009, the incidence of retinopathy of prematurity all stages combined was 32.1% [6]. In another French study including 94 screened newborns with gestational age < 32 weeks or with birth weight < 1500 g in year 2002 the incidence of ROP was 22,3% [7]. The low incidence found in our study (0,22%) could be explained by the fact that the mortality rate is still high among the newborns at risk especially that in our unit we opt for no aggressive therapy for newborns with gestational age < 28 weeks or birth weight < 1000g.
In most developed countries, infants with gestational age > 32 weeks and birth weight > 1500 g are not screened. In our study 2 infants who had a stage III and V ROP were born at 33 weeks gestational age and their birth weight was > 1500g (1900 and 2050g respectively). These two newborns would have been missed if we had used the criteria of developed countries for screening. It seems then reasonable to set criteria for ROP screening programs according to local conditions. In fact, in developed countries, the situation seems to be different from developing ones where ROP is concerning more mature infant [2,8]. This could be explained by the fact that in developing countries other risk factors in addition to low gestational age and low birth weight interfere especially severe sepsis, nosocomial infections, poor management of severe respiratory distress syndrome, lack of monitoring, poor management of apnea etc. aIndeed, recent studies showed that ROP is rather a multifactorial disease. It implicates both oxygen-dependant (including oxygen stress) and oxygen-independent (including deficit in growth factor) mechanisms [1,2,9]. Several conditions or stimuli can lead to these pathogenic mechanisms and many studies have investigated risk factors of ROP. The most reported were low gestational age, low birth weight, respiratory distress syndrome, apnea, duration of artificial ventilation, intraventricular hemorrhage, sepsis, blood transfusion and prolonged parenteral nutrition [2]. Our study did not assess risk factors of this pathology because our sample was not statistically representative. However, we noticed that some factors were rather common in our infant especially respiratory distress syndrome (all infants), duration of artificial ventilation (7/12 infants), apnea (5/12 infants), sepsis and hemodynamic disorders (7/12 infants). Indeed, the risk of ROP persists beyond the first month of life if the newborn is again exposed to the oxygen. In our study, two infants who had a stage V were rehospitalized for severe bronchiolitis.
The decrease of ROP incidence after year 2005 can be explained by the improvement of care for newborns with low gestational age and low birth weight, thanks to the renovation of our unit in 2007. The introduction of new Continuous Positive Airway Pressure (CPAP) devices as well as a device for the measurement of blood gases allowed us a more precise and controlled oxygen administration with a better control of blood pressure and oxygen fluctuations which are known to be implicated in the pathogenesis of retinopathy of prematurity. The introduction of CPAP has also enabled us in combination with caffeine use to improve the management of apnea of prematurity and reduce hypoxic episodes they induce. In addition, the availability of new incubators, new syringes and electric pumps permitted a better controlled parenteral support and then improved the management of newborn premature and low birth weight as evidenced by the decrease in the mortality of children under 32 GW.
The incidence of severe injury and poor outcome especially in the first year of the study could be explained by a still limited specialized management of this disease in our country (photocoagulation treatment Laser Argon was introduced in 2012 and only in private clinics), but also a delayed diagnosis at an advanced stage despite the screening program. The mean delay diagnosis was 10 weeks (4 to 21 weeks). Two infants had missed their first exam and their pupils were poorly dilated in the second exam. For the others the fundus exams were delayed because of the lack of availability of appointments, not only because there was a single ophthalmologist, but also because of the wide selection criteria. This has prompted us to revise our selection criteria in year 2008 considering the new U.S recommendation (≤ 30 weeks gestational age or birth weight <1500g) [10] and the new British recommendations (gestational age ≤ 31 weeks or birth weight ≤ 1500g) [11].
The incidence of ROP decreased after 2005 due to the renovation of the service. To improve the visual outcome of children at risk, it is imperative to improve the early care by training others for screening, the introduction of new screening equipment especially RetCam, and the introduction of new therapies especially Argon Laser.
We thank all patients and their parents.
The Author(s) declare (s) that there is no conflict of interest; This research has not received specific help from public agencies, commercial or other non-profit entities.
Copyright: © 2023 Chiraz Regaieg., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.