Shvets LV1, Kucherov YuI1,2*, Samorokovskaya MV1,2 and Balabanov VS2
1 GBUZ "DGKB No. 9 Named After G.N. Speransky DZM", Moscow, Russia
2 RNIMU Named After N.I. Pirogov of the Ministry of Health of Russia
*Corresponding Author: Kucherov YuI, 1GBUZ "DGKB No. 9 Named After G.N. Speransky DZM" and RNIMU Named After N.I. Pirogov of the Ministry of Health of Russia.
Received: January 11, 2023; Published: February 03, 2023
Citation: Kucherov YuI., et al. “Spontaneous Perforation of Extrahepatic Bile Ducts in A 3-Month-Old Child”. Acta Scientific Paediatrics 6.3 (2023): 03-08.
Spontaneous perforation of extrahepatic bile ducts is a rare surgical disease. In childhood, this condition most often develops at the age of 6 months. The etiological causes of this condition may be blunt abdominal trauma, congenital weakness of the wall of the common bile duct, abnormal pancreato-biliary anastomosis, distal obstruction of the common bile duct, cysts of the common bile duct, increased pressure in the common bile duct. The disease is an extremely urgent condition, however, bright clinical symptoms may not be observed in patients. The purpose of this work is to present a rare clinical observation of spontaneous perforation of extrahepatic bile ducts with the development of sterile bile peritonitis, to increase the alertness of pediatric surgeons to poorly studied and rare pathology in childhood. This article discusses a clinical case of spontaneous perforation of the common hepatic duct in a 3-month-old child who underwent previous surgical treatment for esophageal atresia and distal tracheoesophageal fistula in the newborn period. The etiopathogenetic links of the developed condition in the patient are discussed in order to understand the pathophysiological mechanisms and predisposing factors, the features of its clinical manifestations, the methods of the most indicative variants of instrumental diagnostics for the verification of the disease, the choice of rational and reasonable intraoperative tactics depending on the causes of the disease, comorbid factors, the activity of the inflammatory process in the abdominal cavity, as well as the degree of sterility of the gallbladder peritonitis, the level and volume of damage to the extrahepatic bile ducts and options for surgical treatment of the disease.
Keywords: Spontaneous Perforation; Cyst of the Common Bile Duct; Extrahepatic Bile Ducts; Biliary Peritonitis.
Spontaneous perforation of extrahepatic bile ducts is a rare urgent surgical disease that develops in children of the first months and years of life, ranging from 25 weeks of gestation to 7 years, with a peak incidence of 6 months [1,2]. The earliest reports of spontaneous rupture of the bile ducts were in the works of Dijkstrat in 1932 [4] and Weber in 1934 [5]. The etiology of the disease is not exactly known, but a number of authors in their works suggest that the causes of this condition may be blunt abdominal trauma, congenital weakness of the wall of the common bile duct, abnormal pancreato-biliary anastomosis, distal obstruction of the common bile duct, cysts of the common bile duct, increased pressure in the common bile duct, due to reflux of the pancreatic secretion [3,6-9,15]. In some patients, this condition is preceded by episodes of sepsis or immunological incompatibility in the fetus and mother in the form of an AVO-conflict [18]. According to the statistics of Dr and Jan. [1] the ratio of incidence in boys and girls is 1:2.5, respectively. More often, perforation occurs at the junction of the common hepatic and cystic ducts, since this is the weakest point of the wall of the common bile duct [1,10,11], but sometimes perforation can be noted in other places. As an example, we present a clinical case of spontaneous perforation of the common hepatic duct in a child of 3 months of life, with previous surgery for esophageal atresia, distal tracheoesophageal fistula, with subsequent endoscopic balloon dilation of the esophagus.
To present a rare clinical observation of ADHD in a child of 3 months of life, to increase the alertness of pediatric surgeons to poorly studied and rare pathology in childhood, to discuss etiopathogenetic mechanisms, clinical diagnosis and intraoperative tactics in children with ADHD.
We observed a child of 3 months of life, with previous surgical intervention for esophageal atresia, distal tracheoesophageal fistula. The child underwent direct esophagoesophagoanastamosis and separation of the tracheoesophageal fistula. Subsequently, the child underwent courses of balloon dilation of the esophagus due to stenotic narrowing at the site of anastamosis.
We reviewed the available materials of various authors on this nosology to identify possible clinical variants of the course of the disease, search for pathognomonic symptoms, its clinical diagnosis and intraoperative tactics, in the case of the discovery of SPVL.
A child from the 1st pregnancy, 1 timely operative delivery. The boy was born full-term at 39 weeks, birth weight 3200 g, body length - 52 cm, according to the Apgar scale - 7/8 points. On the first day of life, the child was diagnosed with esophageal atresia with distal tracheoesophageal fistula, for which, on the 1st day of life, the child underwent surgical intervention in the following volume: separation of the tracheoesophageal fistula, imposition of direct esophagoesophagoanastamosis. During 3 months of life, the child received endoscopic balloon dilation of the esophagus 3 times a week. At the age of 2 months, the mother drew attention to the appearance of a weak jaundice of the skin, a lighter color of the stool, dark urine. With these complaints, the child was hospitalized in the clinic. The child underwent a biochemical blood test (total bilirubin - 75 mmol/l). Ultrasonographic examination of the abdominal organs revealed the presence of a voluminous rounded formation in the area of the liver gate. The child was prescribed cholelitic therapy, after which he was discharged home in a satisfactory condition.
The child was admitted to our clinic at the age of 3 months, with complaints about the light color of the stool, dark urine, cough. On examination, weak icterichericity of the skin, a pethial rash on the right cheek were revealed. Auscultatively, the child was listened to dry wheezing on the back surface of both lungs. During palpation, the abdomen is soft, palpation is available in all departments, painless, no peritoneal symptoms were detected. The child calmly reacted to the examination. The child’s stool had a weakly aholic character, the urine was dark in color. A general blood test was performed, mild anemia was detected (Hb - 104g/l), monocytosis (12.5%). In the biochemical analysis of blood, hyperbilirubinemia was noted due to the direct fraction (total - 46 mmol/l, direct - 33.1 mmol/L), gammaglutamyltransferase - 604 units/l.
The child underwent an ultrasound examination of the abdominal organs (Figure 1), which revealed a “large” hydroperitoneum, a volumetric formation of the abdominal cavity and was regarded by us as a cyst of the common bile duct (Type I by Todani). Also, to clarify the diagnosis, the child underwent computed tomography with intravenous contrast enhancement (Figure 2), the picture of which also most corresponded to the cyst of the common bile duct type I according to Todani with signs of hydroperitoneum (ascites). Upon further observation, the condition of the child with negative dynamics, due to the deterioration of the general condition of the child and an increase in the figures of direct hyperbilirubinemia (total - 55 mmol/l, direct - 40 mmol/l), in connection with which indications for diagnostic laparoscopy are formulated.
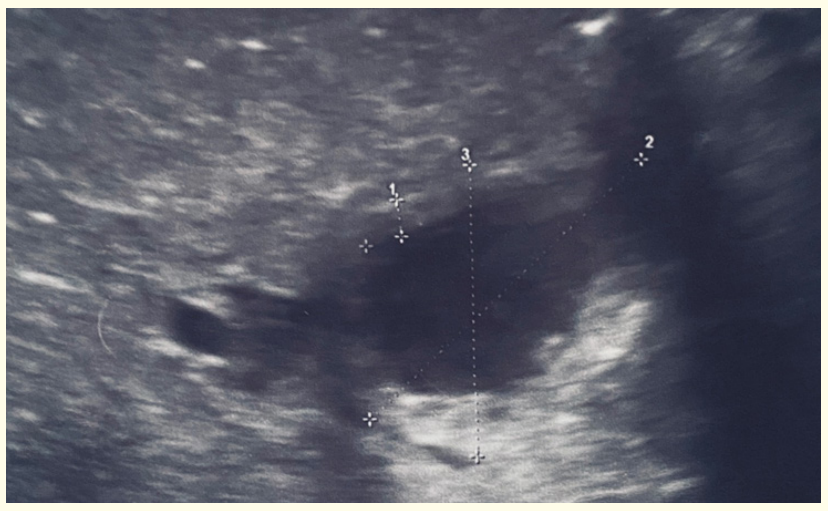
Figure 1: Ultrasound examination of the abdominal cavity organs: hypoechoic formation in the area of the liver gate of a "spindle-shaped" shape, with dimensions of 23 x 18 mm. The formation has well-defined thickened walls up to 2.3 mm. A significant amount of "lumpy" sediment is determined in the cavity of the formation.
Ultrasound examination of the abdominal cavity organs: hypoechoic formation in the area of the liver gate of a "spindleshaped" shape, measuring 23 x 18 mm. The formation has clearly defined thickened walls up to 2.3 mm thick. A significant amount of "lumpy" sediment is detected in the formation cavity.
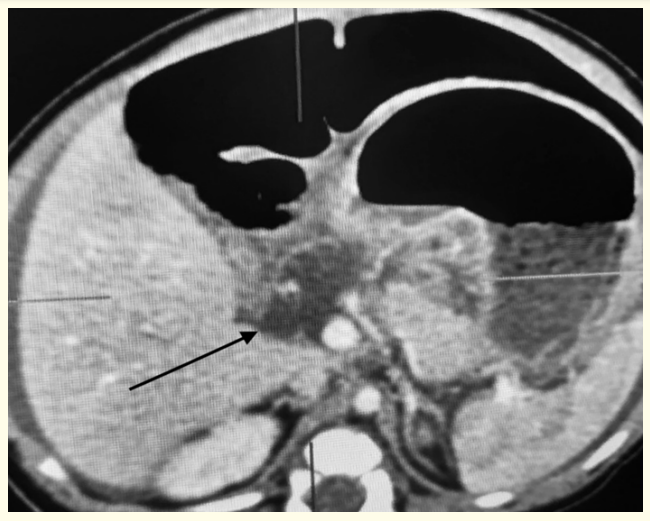
Figure 2: Computed tomography with intravenous contrast enhancement: hypodensive formation in the area of the liver gate (indicated by a black arrow).
Computed tomography with intravenous contrast enhancement: formation of hypodension in the area of the liver gate (indicated by a black arrow).
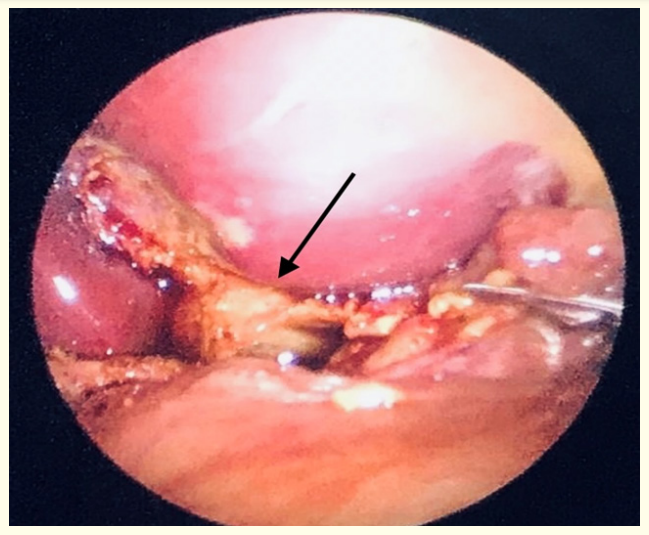
Figure 3: Laparoscopic picture: a false cyst of the common hepatic duct has formed in the area of the liver gate (shown by a black arrow). The surrounding tissues are imbibed with bile. Laparoscopic image: a false cyst of the common hepatic duct formed in the area of the liver gate (shown by a black arrow). The surrounding tissues are soaked with bile.
4 trocars were inserted into the abdominal cavity. During the revision of the abdominal cavity, a large amount of bile contents was revealed, about 500 ml was sanitized. The loops of the small intestine, the large omentum and the liver gate were imbibed with bile. The liver is brown in color, of a tightly elastic consistency, not enlarged in size. During the revision, it was revealed that the gallbladder was reduced in size, in a pronounced adhesive process, the gallbladder was mobilized from adhesions, a false cyst was differentiated at the site of the perforated common hepatic duct (Figure 3). Delicate isolation of the common hepatic duct, gallbladder, and common bile duct was performed. This was the end of the laparoscopy. Next, the child underwent laparotomy through an incision in the right hypochondrium, the peritoneum was opened in layers. At a distance of 20 cm from the ligament of the Tracer, the loop of the jejunum is dissected, a Roux loop is formed 40-50 cm from the ligament of the Tracer (the leading part of the intestine is sewn into the loop of the jejunum end to the side). Through the formed window in the mesentery of the colon, the diverting part of the jejunum is brought to the liver site, the end of the intestine is muffled. A cholicystectomy was performed. The common hepatic duct was isolated, the right hepatic and left hepatic ducts were visualized. A hole has been formed in the jejunum discharge loop, a biliodegistive anastomosis has been applied, the jejunum to the common hepatic duct with nodular sutures. The anastomosis is hermetic. 8 Ch drainage is installed under the anastomosis, it is fixed to the skin from the outside. 12 Ch drainage is introduced into the abdominal cavity into the pelvis, fixed to the skin from the outside.
In the postoperative period, the child received antibacterial, replacement (albumin), transfusion and hemostatic therapy. When performing ultrasonography in the dynamics of hepaticoejunoanastamosis is present. Biochemical parameters have returned to normal. In the future, the child’s condition showed positive dynamics, after which the child was discharged on the 19th postoperative day.
In the presented clinical case, we are faced with two of the most difficult questions for the clinician: how pathognomonic are the symptoms detected in a child for ADHD and which etiopathogenetic component played a key role in this situation?
From the available material on this disease, a number of authors suggest that the cause of the disease may be blunt abdominal trauma, congenital weakness of the wall of the common bile duct, abnormal pancreato-biliary anastomosis, distal obstruction of the common bile duct, cysts of the common bile duct, increased pressure in the common bile duct, due to reflux of the pancreatic secretion [3,6-9]. It is not possible to assess the abnormal pancreato-biliary anastomosis, since we did not perform endoscopic retrograde cholangio-pancreatography, as well as intraoperative cholangiopancreatography. However, Goel., et al. [12], as well as Razumovsky AYu., et al. [18], in their works claim that performing magnetic resonance radionuclide scintigolangiopancreatography (MRRSHG) is the most reliable imaging study to detect extravasation of bile into the free abdominal cavity from the site of perforation of extrahepatic bile ducts. Magnetic resonance imaging (MRI) or magnetic resonance cholangiopancreatography (MRCPG) is less indicative, and the least informative imaging method for detecting perforation is computed tomography (CT) with contrast. In our patient, ultrasound and CT examinations revealed a bulky formation in the area of the liver gate, which we mistakenly regarded as a cyst of the common bile duct, but in fact intraoperatively we found a pseudocyst filled with bile, while we did not identify the true cyst. In their work, Lloyd., et al. [13] mention that due to an increase in pressure in the pseudocyst, due to a violation of the outflow of bile in the distal part of the common bile duct, its rupture is possible, with the development of bile peritonitis. It was biliary peritonitis that we detected during laparoscopy.
The clinical picture of the presented child was not pronounced. So the authors, after analyzing the available literature, say that the most common complaints and clinical manifestations are nausea, vomiting, fever, acolic stools, peritoneal symptoms and abdominal pain. In laboratory parameters, an increase in the level of C - reactive protein and neutrophilic leukocytosis (78.6%) were often determined. The level of total bilirubin exceeded the normal value in 67.9% of cases and only 17.9% due to the conjugated fraction. In 28.6% of cases, there was an increase in AST, ALT and GGT [1]. In our case, only stool acholia, dark urine, icteric skin and petechial rash on the cheek, increasing direct hyperbilirubinemia and increased GGT were clinically detected, while the markers of inflammation were within the reference values. Prevot J. and Babut J. M. suggested that perforation of extrahepatic biliary tracts may develop against the background of a previous infection. Based on this assumption, it can be assumed that the presence of petechial rash in the child was a manifestation of the infectious process. During the laboratory examination, IgM and IgG to cytomegolovirus were detected in the child. Tests for HBV, HCV, EBV, Herpes simplex I, II, Herpes IV, Treponema pallidum, Toxoplasma gondii were negative. Klibsiella pneumoniae was detected in the stool and pharynx crops, which explained the course of respiratory infection upon admission. There is no reason to clearly assert that the course of the infectious process itself served as a predictor of this condition. However, the presence of a dry cough in a child could serve as a trigger for the development of perforation, due to an increase in intra-abdominal pressure and, as a consequence, an increase in pressure in the extrahepatic bile ducts, which led to perforation.
Doneray and co-authors [15] presented a review of a clinical case of spontaneous perforation of a cyst of the common bile duct in an 8-year-old boy who had a history of endoscopic balloon dilation of the esophagus and esophageal augmentation for esophageal stricture after his chemical burn. The authors suggested that it was the esophageal dilation procedures that triggered the rupture of the cyst of the common bile duct, which led to biliary peritonitis. An increase in intra-abdominal pressure, at the time of endoscopic dilation, due to gag Reflex, causes an increase in intra-abdominal pressure. In their study, Emir., et al. [16] showed that any increase in intra-abdominal pressure, including during laparoscopy, can affect the oxygenation of the rabbit colon.
Congenital weakness of the extrahepatic bile duct wall is also an important predictor in the development of the disease. Blood supply to the extrahepatic bile ducts in 60% of cases is carried out from the posterior branch of the upper pancreatoduodenal artery, while the remaining 40% is from the common hepatic artery. These arteries run along the common bile duct and are proximal to the junction of the common hepatic and cystic ducts. The junction of the common hepatic and cystic ducts receives the most terminal blood supply from these arteries, as a result of which these anatomical structures are the lowest possible point of blood supply and perfusion pressure, which is a predictor of congenital weakness of the wall of the common bile, common hepatic and cystic ducts [1,17]. Thus, from the above data, it is justified to assume that congenital weakness of the wall of the biliary tract and increased intra-abdominal pressure (regardless of the cause) and as a consequence of ischemia of their wall, are predisposing factors to the development of spontaneous perforation of extrahepatic bile ducts. In our clinical case, probably the reason for the increase in intra-abdominal pressure was the presence of a respiratory infection in the patient, which was accompanied by a dry cough and endoscopic balloon dilation of the esophagus.
As for intraoperative tactics, we performed the formation of hepaticoejunoanastomosis on a disconnected Roux loop. A number of authors report that the surgical tactics in case of ADHD may be limited to conservative methods of treatment, such as drainage of the false cyst cavity by external drainage, performing cholecystostomy and choledochostomy by T-shaped drainage. In their work, Yan., et al. [1] showed that the choice of operative tactics depends on the condition of the liver gate, since bile extravasation causes severe inflammation. In the case of large perforations, preference should be given to external drainage of the common bile duct by Tshaped drainage. Cholecystostomy, as one of the simplest and most justified methods of treatment, should be performed under the condition of a small perforation in the extrahepatic bile ducts, as well as in the case of perforation of the gallbladder. However, cholecystostomy is associated with the risks of insufficient drainage of bile and the development of recurrent bile peritonitis. To solve this problem, it is proposed to place safety drains in the subhepatic bag and small pelvis. If it is possible to carry out the MRCP, it must be carried out. If it is impossible to perform the study, priority is given to cholecystostomy or choledochostomy by T-shaped drainage.
In urgent cases, when intraoperatively, due to severe inflammation in the abdominal cavity, it is not possible to reliably verify the site of bile leakage or to mobilize anatomical structures in the area of the liver gate without the risk of damage, it is possible to limit ourselves to simply removing safety drains from the subhepatic space, splenic sac and Douglas pocket, until the inflammatory process subsides, on average by 3-4 weeks.
The intraoperative decision to suture the perforating hole is fundamentally wrong and should not be considered as an option of surgical tactics, since, firstly, this will lead to imminent stenosis in the perforation area, and secondly, there is a high risk of damage to the structures of the liver gate, due to poor visualization against the background of a pronounced inflammatory process.
Performing biliodigestive anastomoses on a disconnected Roux loop is possible only in cases when the patient has a cyst of the common bile duct, in the wall of which perforation has occurred and under the condition of sterile bile peritonitis. As a rule, this surgical intervention is performed in the second stage. But it is worth remembering that with any tactic adopted during surgery, the main point is a good and complete sanitation of the abdominal cavity, especially the area of the liver gate.
In our case, the patient did not have inflammatory markers in the blood and signs of a systemic inflammatory reaction, as well as inflammation of the abdominal cavity, and therefore biliary peritonitis was regarded as sterile, which in turn was not a contraindication to performing hepaticoejunoanastomosis on a disconnected Roux loop by the first stage.
Spontaneous perforation of the extrahepatic biliary tract is a relatively rare surgical disease. Etiopathogenetic components are still worth studying, accumulating experience and clinical observations about this pathology. Practicing surgeons should be aware of the risks of developing ADHD in children with a cyst of the common bile duct. The attention of surgeons should also be attracted to children with changes in the biochemical analysis of blood, with signs of sluggish peritonitis, visual signs of ascites and changes in the area of the liver gate, considering these indicators as signs of SPVLP. The choice of intraoperative tactics depends on the presence of inflammation in the abdominal cavity, the size of the defect in the extrahepatic bile ducts, as well as on the possibility of intraoperative instrumental diagnosis.
The authors of the article confirmed the absence of a conflict of interest, which must be reported.
Voluntary notification the consent of the patient’s legal representatives to the publication of the clinical case has been obtained.
Copyright: © 2023 Kucherov YuI., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.