Nasibova EM*, Polukhov RSh and Polukhova A
Azerbaijan Medical University, Baku, Azerbaijan
*Corresponding Author: Nasibova EM, Azerbaijan Medical University, Baku, Azerbaijan.
Received: October 27, 2022; Published: November 29, 2022
Citation: Nasibova EM., et al. “Caudal Anesthesia as an Alternative for Surgical Interventions for the Correction of Anorectal Malformations in Newborns and Young Children”. Acta Scientific Paediatrics 5.12 (2022): 25-31.
Background: The frequency of anorectal malformations worldwide is 1:2000-1:5000 newborns. Surgical correction for anorectal malformations is a significant operation, accompanied by severe pain. Currently, little research is available on the use of caudal block for anorectal malformation surgery. We hypothesized that general anesthesia combined with a caudal blockade could effectively relax the anal muscles, which significantly reduces the complexity of the operation and shortens the duration of the operation. In this study, we evaluated the effect of caudal blockade on the duration of the operation and on postoperative pain relief.
Methods: The research work was carried out in the surgical clinic of the AMU. The study included 65 children aged 0 to 3 years at risk of ASA class II anesthesia. Depending on the method of anesthesia, the patients were divided into two groups: group I - patients with general anesthesia and group II - general anesthesia in combination with caudal blockade.
Results: The recovery time after extubation in the general anesthesia + caudal block group was significantly shorter than in the general anesthesia group (17.05 ± 4.7 min vs. 10.79 ± 4.2 min, P < 0.01). Hemodynamic changes (HR, SBP and DBP) during operations between the two groups were similar before intubation and at the beginning of the operation (P > 0.05). During the traumatic moment of the operation, the average heart rate in group II (general anesthesia + caudal block) was significantly lower than in group I (general anesthesia) (130.72 ± 17.74 versus 115.28 ± 16.19, p = 0.010), but there are significant differences in SBP or DBP between the two groups.
Conclusion: General anesthesia in combination with a caudal block is an effective, safe method of anesthesia for complex surgical interventions for anorectal malformations in newborns and young children. This technique allows to reduce the duration of the operation and improves the postoperative period.
Keywords: General Anesthesia; Caudal Block; SEVOFLURAN.
The frequency of anorectal malformations worldwide is 1:2000-1:5000 in newborns [1]. Surgical correction for anorectal malformations is a significant operation, accompanied by severe pain. Patients who undergo such operations are usually newborns and young children with a special reaction to pain. According to statistics, 1.5 million newborns undergo surgery every year, requiring anesthetic support [2]. Currently, the Crickenbeck classification of congenital anorectal malformations is used, according to which the main clinical group is distinguished (perineal fistula, rectourethral fistula (bulbar and prostatic)), vestibular fistula, cloaca, anorectal malformation without fistula, anal stenosis) and rare anomalies (rectal sac, atresia or rectal stenosis, rectovaginal fistula, H-shaped fistula, and other malformations). Surgical interventions cause various endocrine, immunological, and neurovegetative changes in the patient’s body. The totality of endocrine, inflammatory and metabolic changes in response to surgical intervention is a surgical stress response. Sympathetic nervous system activation, pituitary hormone secretion, insulin resistance, cytokine production, and neutrophilic leukocytosis form the basis of the surgical stress response.
Consequently, the surgical stress response causes intra- and postoperative dysfunction of various organs and systems, which increases postoperative complications and prolongs the rehabilitation period. Caudal blockade significantly reduces the increase in cortisol and glucose in the blood plasma during traumatic operations for anomalies of the anorectal region. Newborns exposed to the intense pain of these surgeries are at high risk for neurodevelopmental disorders and changes in pain sensitivity. Despite the increase in the frequency of colorectal operations performed in newborns and their severity, the choice of optimal anesthetic support is still relevant and the subject of discussion. Until relatively recently, anesthesia using opioids has been the gold standard. Currently, regional anesthesia is becoming more widespread, which is increasingly becoming a routine method of analgesia in young children with colorectal malformations.
The anesthetic allowance impacts the course and outcome of the postoperative period. Insufficient analgesia in the perioperative period can lead to the development of encephalopathy in the future [3].
Drugs used for general anesthesia have a specific effect on the newborn’s body. Newborns and young children are characterized by increased sensitivity of the respiratory system to opioids. One of the reasons that increase the sensitivity of newborns to opioids, with the exception of remifentanil, is the reduced rate of their excretion in children during the first three months of life, especially in premature infants. A similar effect was not found in children aged 3-6 months of life [2].
Currently, the issue of the advantages and disadvantages of using total intravenous anesthesia as an alternative to inhalation anesthesia remains debatable. It has not been fully resolved which drugs for intravenous anesthesia were optimal in newborns and young children - propofol, midazolam or dexmedetomidine.
An important place in the modern anesthetic management of anorectal malformations belongs to regional methods, caudal anesthesia has become widespread. The high risk of death during general anesthesia is associated with possible respiratory complications in the postoperative period. The use of regional anesthesia in combination with general anesthesia not only reduces the incidence of adverse outcomes, but is also characterized by high economic efficiency by reducing the length of the patient’s stay in the hospital. The reduction of perioperative pain in patients operated on for anorectal malformations is achieved using minimally invasive laparoscopic technologies.
Caudal block reduces the stress response to surgery and provides excellent postoperative pain relief with no or minimal need for narcotic analgesics, thereby reducing the risk of postoperative hypoventilation and apnea. Newborns tolerate high levels of regional blockade up to the level without hemodynamic compromise. A caudal block is ideal for surgery because infants with anorectal anomalies may have concomitant spinal cord anomalies. Caudal block is one of the preferred regional anesthetics for anorectal malformations, and its advantages include prostate safety, prostate safety, and a low complication rates. Caudal blocks can reduce the excitability of sympathetic nerves and have the same obvious effects as analgesics and muscle relaxants, facilitating surgery and promoting postoperative recovery. Currently, little research is available on the use of caudal block for anorectal malformation surgery. We hypothesized that general anesthesia combined with a caudal blockade could effectively relax the anal muscles, significantly reducing the operation’s complexity and shortening the operation’s duration. In this study, we evaluated the effect of caudal blockade on the duration of the operation and postoperative pain relief.
Thus, anorectal malformations are an actual problem of modern pediatric surgery. Despite the significance of the problem, at present, the tactics of anesthetic management, the choice of the optimal anesthetic method still needs to be fully defined, which requires further research.
The research work was carried out in the surgical clinic of the AMU. The study included 65 children aged 0 to 3 years at risk of ASA class II anesthesia. The structure of surgical pathology in which multimodal combined anesthesia was performed was: atresia or stenosis of the rectum, rectourethral fistula, vestibular fistula, rectovaginal fistula, etc. Depending on the method of anesthesia, the patients were divided into two groups: group I - patients with general anesthesia and group II - general anesthesia in combination with caudal blockade. The study protocol was approved by the AMU ethics committee prior to the start of the study. The anesthesia protocol was the same for patients of group I: premedication was carried out only in children aged 1-3 years with midazolam at a rate of 0.4 mg/kg per os 20 minutes before surgery, anesthesia was induced with sevoflurane according to the “step” method using the Drager Fabius apparatus according to semi-closed circuit at 5-6 vol% (MAS 1.5-2.5 vol%) for 3-5 minutes, followed by tracheal intubation with rocuronium bromide 0.6 mg/kg, fentanyl 5 µg/kg, and sevoflurane 3 vol% (MAC 1.2-1.5%). And in patients of group II - general anesthesia in combination with caudal blockade, the protocol of anesthesia was as follows: induction of anesthesia was carried out with sevoflurane according to the “step” method using the Drager Fabius apparatus in a semi-closed circuit at 5-6 vol% (MAC 1.5-2.5 vol. %) for 3-5 minutes, followed by tracheal intubation without the introduction of muscle relaxants and the supply of sevoflurane 3 vol% (MAC 1.2-1.5%). Then, a puncture of the caudal space was performed with a bolus injection of 0.25% ropivacaine at a rate of 1.0 ml/kg in combination with dexamethasone 0.1 mg/ kg. There were no complications during the caudal block. The hypnotic effect of anesthesia throughout the operation was achieved by using 0.8% sevoflurane. In the intraoperative period, almost no analgesics and muscle relaxants were used. The duration of the surgical intervention averaged 94 ± 10 minutes. Intraoperatively and in the postoperative period, heart rate, blood pressure (systolic, mean, and diastolic), SaO2, gas exchange parameters, glycemia, and cortisol concentration were monitored). After waking up, the pain syndrome was assessed using visual analog, verbal and mimic scales for assessing pain intensity. Hemodynamic changes (including heart rate, systolic blood pressure (SBP), and diastolic blood pressure (DBP)) were recorded before induction of anesthesia, at the beginning of the operation, at the most traumatic moment of the operation, and at end of the operation. Postoperative pain intensity was assessed using the Face, Legs, Activity, Cry, Comfort Scale (FLACC), which assesses pain intensity by valuating five types of behavior (face, legs, activity, comfort, cry) to give a score range of 0 to 10 and each score on the scale has a possible value from 0 to 2. When assessing the intensity of pain on a scale, 10 indicates maximum pain, 0 indicates relaxation/comfort, 1-3 indicates mild discomfort, 4-6 indicates moderate pain, and 7-10 points - for severe discomfort. Pain assessment using the FLACC scale was also performed 1, 6, 12, and 24 hours after surgery. The incidence of side effects after extubation, including laryngospasm, restlessness, nausea and vomiting, was compared between the two groups. The obtained quantitative and qualitative data were subjected to statistical processing by biostatistical methods: variational (t-Student, U-Mann-Whitney, KU-Kruskal-Wallis), dispersion (test ANOVA, FFisher) and discriminant (Pearson Chi-Square) analyzes using statistical packages EXCEL-2013 and SPSS-21.
Of the 65 children included in the research, 30 were assigned to group I (general anesthesia) and 35 children to group II (general anesthesia + caudal block). Patient demographics are shown in table 1.
Figure 1-3: Transanal endorectal bowel relegation in Hirschsprung disease.
Figure 4-7: Caudal anesthesia for atresia with vestibular fistula.
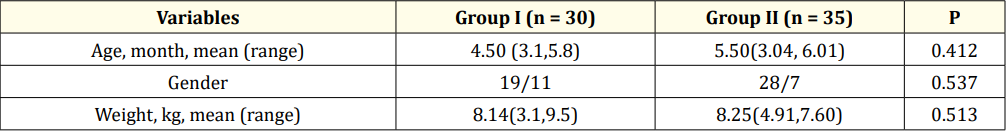
Table 1: Demographic characterizes.
Patients in both groups were comparable in age, sex and weight.When comparing the duration of the operation, it was found that II group (general anesthesia + caudal block) had a significantly shorter operation time (94 minutes vs. 84 minutes P = 0.040). The recovery time after extubation in the general anesthesia + caudal block group was considerably shorter than in the general anesthesia group (17.05 ± 4.7 min vs. 10.79 ± 4.2 min, P < 0.01). Hemodynamic changes (HR, SBP and DBP) during operations between the two groups were similar before intubation and at the beginning of the operation (P > 0.05). During the traumatic moment of the operation, the average heart rate in group II (general anesthesia + caudal block) was significantly lower than in group I (general anesthesia) (130.72 ± 17.74 versus 115.28 ± 16.19, p = 0.010), but there are significant differences in SBP or DBP between the two groups. Thus, hemodynamic parameters during surgery in the general anesthesia + caudal block group were more stable than in group I (general anesthesia) (Table 2). There was no significant difference in the incidence of side effects (including laryngospasm, restlessness, nausea and vomiting) between the two groups I (33%) vs. II (24.2%,) (P > 0.05). When assessing postoperative pain using the FLACC scale, it was found that in the group of general anesthesia + caudal block, pain appeared only 6 hours after surgery than in the group of general anesthesia (1 hour after surgery), still there were significant differences between the two groups after 12 and 24 hours after the operation was absent (P > 0.05).
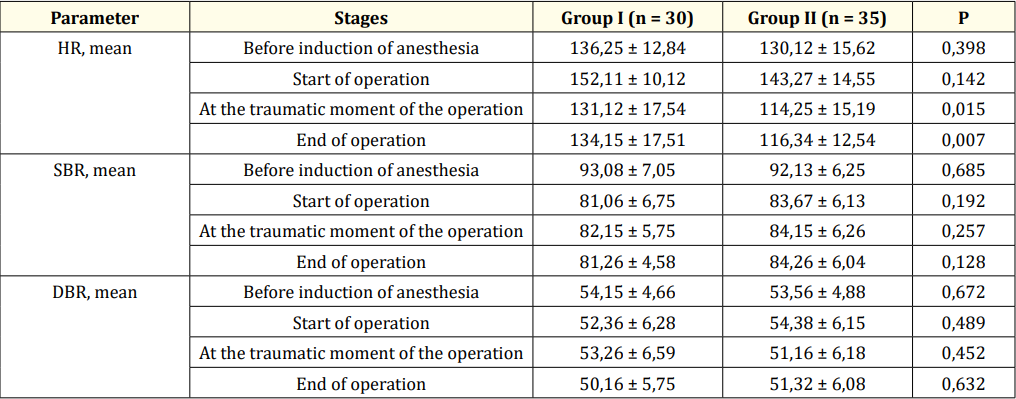
Table 2: Dynamics of changes in hemodynamic parameters.
The present study shows that caudal blockade in combination with general anesthesia can be successfully used in surgical interventions for anorectal malformations in newborns and young children. General anesthesia can cause hemodynamic and respiratory complications during the perioperative period, as well as potential neurotoxicity [4,5]. The combination of general anesthesia and caudal block reduces the neurohumoral response to surgery, alleviates intraoperative inhalation and consumption of opioid agents, and accelerates early mobilisation and recovery [6]. The high incidence of life-threatening respiratory complications after general anesthesia decreased after awaking regional anesthesia.
Suresh., et al. investigation of 18, 650 children who received caudal block showed that the incidence of complications was 1.9% (1.7%-2.1%), demonstrating that the procedure is safe and should be widely used [7,8].
On the other hand, general anaesthesia is regarded to be safe, still the risk of postoperative apnoea and hypoxaemia is not negligible in infants born preterm and operated upon before 46 weeks of post-conceptual age. The probability of apnoea in these patients may be up to 20%, especially in infants with a post-conceptual age - 45 weeks. The rate of apnoea in our patients was very low, and no difference between infants, born preterm or operated upon before 46 weeks of post conceptual age, and children was observed.
The spinal column of children is straight, while epidural adipose tissue, lymphatic vessels, and vascular plexus are abundant, and the sacral canal volume is small. The anesthetic injected into the sacral canal easily spreads to the thoracic epidural space, and the block area can reach the level of 6-8 thoracic vertebrae. The analgesic and muscle relaxant effects of anesthetics satisfy the requirements of transanal operation, reduce the draw reaction during laparoscopic surgery, and provide more stable hemodynamics. An optimal analgesic effect can avoid the stimulation of the sympathetic adrenal medulla reduce the release of catecholamine, and reduce the irritation caused by tracheal intubation, skin incision and transanal operation. Šabanović Adilović., et al. found that caudal block with analgosedation provides better control of intraoperative hemodynamic conditions, postoperative emergence delirium, and postoperative pain compared with general endotracheal anesthesia [9]. In our study, the II group received general anesthesia combined with caudal block, and the hemodynamic changes during transanal operation were more stable than those in the I group.
The FLACC scores at 1 h and 6 h after surgery and the mean dose of sufentanil were lower, suggesting that general anesthesia combined with caudal block can provide a better analgesic effect. The duration of operation, particularly that of transanal operation of the II group were significantly shorter, and we don’t use rocuronium than that in the I group, indicating that the caudal block could effectively relax the anal muscles.
Alizadeh’s study [10] indicated that caudal block, in addition to general anesthesia had, a favorable effect on reducing blood loss during operation, operation duration, and analgesic use, in agreement with our findings.
Kim., et al. found that caudal block significantly reduced the sevoflurane concentration for a smooth laryngeal mask airway removal in anesthetized children, reduced airway complications and led to faster recovery [11]. In the II group, the recovery time was shorter, possibly to due to the lower mean doses of rocuronium. A previous study found that caudal block could provide a more effective and lasting analgesic effect but was associated to more side effects than general anesthesia [12]. Another study suggested that caudal block was not associated with postoperative side effects [13]. However, in our study we found no differences in the incidence of complications between the two groups.
In combination with a caudal block, general anesthesia is an effective, safe method of anesthesia for complex surgical interventions for anorectal malformations in newborns and young children. This technique reduces the operation’s duration and improves the postoperative period.
Copyright: © 2022 Nasibova EM., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.