Ali Raza Brohi*, Naseem Mengal, Ali Raza Brohi, Imran Ali Bajwa, Muhammad Saleh Khaskheli and Rafia Tabbasum
Professor and Chairman Paediatric Surgery, Dean Faculty of Surgery and Allied Sciences, Peoples University of Medical and Health Sciences, Nawabshah, Sind, Pakistan
*Corresponding Author: Ali Raza Brohi, Professor and Chairman Paediatric Surgery, Dean Faculty of Surgery and Allied Sciences, Peoples University of Medical and Health Sciences, Nawabshah, Sind, Pakistan.
Received: July 05, 2022; Published: July 13, 2022
Citation: Ali Raza Brohi., et al. “Laparoscopic Inguinal Hernia Closure is Safe and Effective Technique in Children”. Acta Scientific Paediatrics 5.8 (2022): 03-06.
Introduction: Inguinal hernia is a common pediatric surgical problem in children having an incidence of 0.8% to 4.4%. Open herniotomy is still the procedure of choice even after the advent of minimal invasive surgery due to anesthetic considerations, increase recurrence rates in laparoscopic hernia repairs. Laparoscopic inguinal hernia repair has obvious advantages like cosmetically better outcome, shorter operative time, early recovery, dealing of unidentified opposite site hernias with decrease risk of damage to spermatic cord in males and wound infections.
Material and Methods: We reviewed the medical records of the 175 patients who underwent laparoscopic inguinal hernia closure from January, 2015 to December, 2021 at Peoples University of medical health sciences, for women. We reviewed the demographic data, laparoscopic findings, operative time, hospital stay, post-operative complications and follow-up.
Results: During this six-year study period 175 patients were operated by laparoscopic technique. The mean age of presentation was 1.6 years (range 1~ 3, with ± 0.73 SD). 83% were boys and 17.1% were girls. The mean operative time for unilateral hernia was 22.5 mins (± 10.394 SD) and 45mins (± 6.93SD) for bilateral hernia. The hospital stay was 24hrs in most cases except in few where there was gut involvement.
Conclusion: Laparoscopic inguinal hernia repair is a safe technique in an expert hand and have an advantage of ligating sac without dealing the cord in male patients, assessing contralateral PPV and simultaneously dealing the contralateral site preventing the future metachronous hernia.
Keywords: Laparoscopic Inguinal Hernia; Closure; Children.
Inguinal hernia is a common pediatric surgical problem in children having an incidence of 0.8% to 4.4% [1]. Patent processes vaginalis is the main reason of inguinal hernias, especially more common in males then females. Open herniotomy is still the procedure of choice even after the advent of minimal invasive surgery due to anesthetic considerations, increase recurrence rates in laparoscopic hernia repairs [2]. In early 1990s, the laparoscopic inguinal hernia repair evolved since then different techniques had been introduced with variable outcomes for e.g., single port vs three port technique either extracorporeal suturing or intracorporeal suturing [3].
Laparoscopic inguinal hernia repair has obvious advantages like cosmetically better outcome, shorter operative time, early recovery, dealing of unidentified opposite site hernias with decreased risk of damage to spermatic cord in males and wound infections [46]. The aim of this study is to assess the feasibility and success rate in terms of technique and post-operative complications.
We reviewed the medical records of the 175 patients who underwent laparoscopic inguinal hernia closure from January 2015 to December 2021 at Peoples University of medical health sciences, for women after approval from ethical board review. In our study we included those patients who were above 6 months till 12 years in age, large hernias, bilateral hernias, having positive history of swelling in inguinal region, hernias in both gender. The exclusion criteria was if there is history of incarcerated hernia, association with connective tissue disorders or syndromes, age less than 6 months. All the cases were done by single surgeon and parents were counselled about the procedure and its related problems. We reviewed the demographic data, laparoscopic findings, operative time, hospital stay, post-operative complications and follow-up. The patients were followed for 6 months, initially the follow-up was weekly based for one month, then every month till 6 months to observe the surgical complications.
All statistical analyses were done by using IBM SPSS 25 version. Categorical variables were expressed in frequency and percentages. Quantitative data were expressed as mean ± standard deviation (SD).
We did with three port technique, 5mm port at umbilicus for 00 camera and two working ports of 3mm on right and left of camera port and the position of working ports variable depending on which side to be operated and also if there is bilateral hernia (Figure 1 and 2). After identification of internal ring without dissecting sac, the suture (Ethibond 2/0 or vicryl 3/0) was inserted direct through the abdominal wall and taking the peritoneum
fold bit by bit in a purse string fashion all around ring taking care of vas deferens and vessels and then tied around ring. In some cases, second stitch of peritoneum taken to strengthen the repair.
In female patients, majority of the patients we did purse string closure of the ring but in few cases where sac was large laparoscopic inversion and ligation (LIL) technique was done where after the inversion of the sac and ligating at the ring the redundant sac was excised.
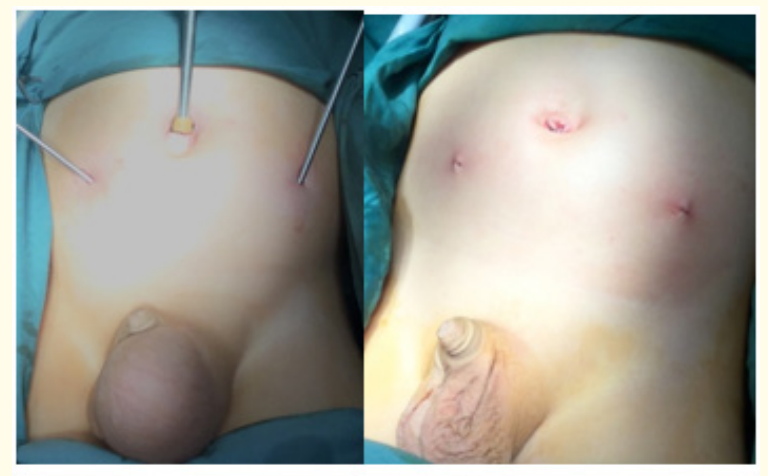
Figure 1 and 2: Port Position and Post-Operative.
During this six-year study period 175 patients were operated by laparoscopic technique. The mean age of presentation was 1.6 years (range 1~ 3, with ± 0.73 SD). 83% were boys and 17.1% were girls. In 175 patients, 75(42.9%) patients had right side, 48(27.4%) patients had left side, 35 (20%) had bilateral and 17 (9.7%) had only history of swelling. The laparoscopic findings in 175 cases are listed in (Table 1a and 1b). The mean operative time for unilateral hernia was 22.5 mins (± 10.394 SD) and 45mins (± 6.93SD) for bilateral hernia. The hospital stay was 24hrs in most cases except in few where there was gut involvement. Out of 175 patients, only 7 (4%) patient developed recurrent hernia. In 145 male patients, we observed hydrocele in only 6 (4.1%) cases and hematoma in 4 (2.7%) cases. None of the case had testicular atrophy and testicular ascent.
Minimal invasive surgery is the demand of time because of its improved aesthetic effect. Initially laparoscopy was used to identify the contralateral patent processes vaginalis but nowadays laparoscopic inguinal hernia repair is a routine throughout the world with a modifications in technique [6,7]. In our study, 83% are males and 84.5% were below 6yrs in age that is consistent with other studies and the commonest side is right side [8].
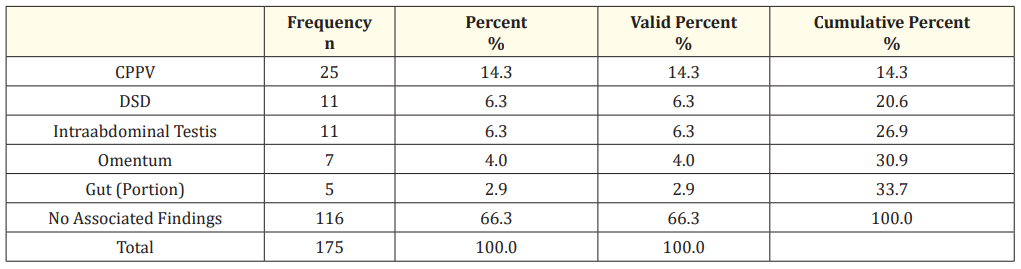
Table 1a: Laparoscopic Findings.
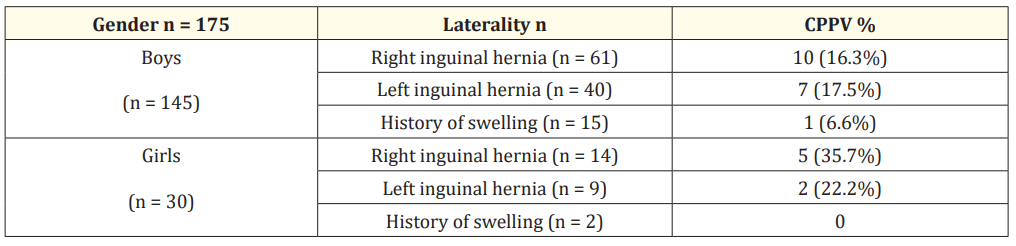
Table 1b: Laparoscopic Findings.
Besides its cosmetic advantage, laparoscopy can determine the contralateral PPV and the other associated findings which can’t be delineated by open surgery [9]. But still it is controversial that it should be ligated or not at the same time [10], as some scholars interpreted that 10% of contralateral PPV will develop hernia in future and some believe that it should be ligated to prevent future hernia development and hospitalization [11,12]. In our study what we observed that 14.3% patients had contralateral PPV and in all cases we closed it to prevent future hernia development that is comparable with other studies [13].
Igwe., et al. reported in his prospective study that there is no significant difference between operative times of open vs laparoscopic hernia repair [14]. In our study, there is significant difference between the times of laparocscopic hernia repair and more prolong in cases of bilateral as it’s technically difficult to apply intracorporeal knotting taking care of spermatic cord structures in cases of male compared to the female patients where there is no danger of cord.
A recurrence rate of 0.8% to 4.3% has been reported in literature for laparoscopic repair vs open repair [15] Alzahem., et al. in their meta-analysis observed higher recurrence rate after laparoscopic inguinal hernia repair [5]. A meta-analysis by Yang., et al. conducted in 2011 in which he observed that few studies show higher and few show lower recurrences after laparoscopic repair [16]. Multiple reasons have been suggested for these recurrences including large hernias, closure of internal inguinal ring in tension, technical problems.
In our study, we observed recurrence in 7 patients and that recurrence occurred those who were having large hernia sac. Initially we use to apply single purse string suture, after these recurrences now we apply double purse string when the hernial sac is large and most of these recurrences were in male patients.
Besides all that one thing more we noted in our study was DSD in 11 patients, which we could have missed it out in open techniques and the overall complication rate in both genders is about 9.7% and in males overall complication rate is 7% which is quite less than open techniques. Luckily in our study, we haven’t seen testicular atrophy, testicular ascent except hydrocele in 6 patients in male patients nor we have observed surgical site infection that is comparable to other studies [13,17].
One of the benefit of laparoscopy is early recovery and yes it’s quite true as majority of our patients remained in hospital for 24 hours except few where gut was involved but they discharged after 48hrs.
Laparoscopic inguinal hernia repair is a safe technique in an expert hand and have an advantage of ligating sac without dealing the cord in male patients, assessing contralateral PPV and simultaneously dealing the contralateral site preventing the future metachronous hernia formation, re-hospitalization and general anesthesia.
Copyright: © 2022 Ali Raza Broh., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.