Manfred Mortell RN*
Department of School of Nursing and Allied Health Professions, University of the Bahamas, Bahamas
*Corresponding Author: Manfred Mortell RN, Department of School of Nursing and Allied Health Professions, University of the Bahamas, Bahamas.
Received: June 13, 2022; Published: June 28, 2022
Citation: Manfred Mortell RN. ““Failure to Rescue” Is Your “Crash Cart” Prepared? A Paediatric Case Study?”. Acta Scientific Paediatrics 5.7 (2022): 58-67.
“Failure to rescue” is a matter that fosters patient morbidity and mortality related to medical errors. The inquiry confronted in this short communication is, “why are patients “failing to be rescued” by healthcare professionals (HCP)?” This short communication examines and discusses the concept of “Failure to rescue” as an indication of the quality of care which also assumes that, while problems may reflect the seriousness a patient’s illness, there are related health care factors which must be considered. The capacity to “rescue” patients once complications occur is closely linked with the quality of health care being provided. This article highlights the concept of failure to rescue with a case paediatric case presentation which underscores the consequences of sub-standard care, and risk incidents which are often associated with “failure to rescue” states. One such “failure to rescue” and hazard concerns non-compliance by HCP when substantiating and documenting equipment checks on “crash carts”. Failure to do so, not only compromises patient safety, but creates conceivable harm for all patients, due to a failure of crash cart preparedness. Crash carts are tools which are utilised for emergency procedures, such as cardiopulmonary arrest and must be checked and prepared in the event of a life-threatening situation. If crash carts are not reliable due to ineffective checks, then failure to rescue will be inevitable. Research into the causes of “failure to rescue “reveals the complexity of the problem, with parallels that reflect insight such as organisational failure, deficiency of knowledge and skills, a deficit of supervision and inadequate staffing levels which together with excessive workloads created time demands for healthcare providers making it problematic to prioritise their responsibilities. However, despite these circumstantial facets, it is the author's opinion, that “failure to rescue” related to false checking and documentation of equipment on “crash carts” by HCP involves a “failure in ethics.” That failure being a deficit in a HCP’s moral duty of care which ensures that patients are safe and protected from harm if emergency care is required. There is a crisis of ethics where theory and practice integrate, and consequently, malfeasance, and we as HCP are forsaking our duty as patient advocates.
Keywords: Case Study; Crash Cart; Ethics; Failure to Rescue; Medical Error; Practice; Theory.
How many times in my 40 year nursing career, regardless of the setting, have I heard the words, "I need help", "Call Code Blue", "Get the Crash cart", "Quick bring the, Code cart" and when the rapid response team, Code blue team or crash cart" arrived the crash cart was not prepared, and as a consequence, the infant or child who required rescuing, was not rescued and subsequently harmed.
Look closely at your departmental or organizational “crash carts” and decide if they are prepared for a life-threatening emer gency. Countless “crash carts” have hidden issues that could contribute to a patient safety event [1].
While considerable research literature on crash cart-related safety events concentrates on medication errors [1,2], this short communication will focus on “failure to rescue” and pediatric patient safety threats in regard to non-compliance by HCP when validating and documenting equipment checks on “crash carts”. It is therefore worthwhile to remember that the objective of a “crash cart” is to ensure that the authorized emergency equipment, medications, and supplies are immediately available for any emergency[1].
Patient harm in healthcare, is a patient safety concern and a primary source of morbidity and mortality worldwide [3]. The World Health Organization (WHO) defines patient harm as “an incident that results in harm to a patient such as impairment of structure or function of the body and/or any deleterious effect arising there from or associated with plans or actions taken during the provision of healthcare, rather than an underlying disease or injury, and may be physical, social or psychological” [4]. The health burden and patient experiencing healthcare-related patient harm has been reported to be comparable to chronic diseases such as multiple sclerosis and cervical cancer in developed countries, and tuberculosis and malaria in developing countries [2].
Patient safety has been defined as “the avoidance, prevention and amelioration of adverse outcomes or injuries stemming from the process of health care” 5 Patient safety is related to quality of care, but these two concepts are not synonymous. Safety is a principal element of quality [5]. Quality of care incorporates other components such as effectiveness, patient focus, timeliness, efficiency, and equity [6].
Care can be of poor quality, and still be safe, but unsafe care can never be considered of good quality [7]. Patient safety in health care related to medical errors were made blatantly transparent by the publication of the Institute of Medicine’s report “To Err is Human”: Building a safer health system [6]. Subsequently strategies to enhance clinical practice and policies were targeted as a method to improve safety and quality of patient care, which preceded the creation of regulatory associations such as the Nationwide Alliance of Patient Safety Organization (NAPSO). The aim of NAPSO was to eliminate preventable harm and improve quality of care in healthcare systems [8]. However, since the testament “To Err is Human”: Building a safer health system [6], it is nowadays generally accepted that medical errors cannot be eliminated and therefore the emphasis is on minimising its impact [8-12].
Escalating mindfulness focuses on identifying and modifying dysfunctional systems to sponsor patient safety, with approaches to safety being targeted within entire organisations. Studying the underlying causes of error and near misses is deemed central for promoting both ‘single loop’ learning, that is, correcting problems within existing structures and processes and the less common ‘double loop’ learning, which studies assumptions and goals, reconfigures structures, and processes [13]. Identifying and challenging dysfunctional systems are perceived to be priorities [13]. It was Dr. Lucian Leape’s article, “Error in Medicine,” which introduced the concept of systems rather than individual-based failures as the cause of medical errors. His labors regarding patient safety have advanced the diffusion of the concepts related to human factors and systems reasoning, which has provided meaningful understanding and advancement within the sphere of health care [14].
However, it is the author's belief, that conceptions accompanying human factors and systems, cannot be held entirely responsible for the medical errors incurred within the sphere of health care. A unique paradigm the “theory-practice-ethics gap” conveys an explanation to consider, as to why HCP may not perform their patient advocacy role, and as such, an additional factor called ‘Ethics’ must be reflected on, when evaluating some of the medical errors in health care practice [15]. One such medical error, and patient safety dereliction is the “failure to rescue” an infant or a child who requires basic or advanced life support as a patient, in a hospital. “Failure to rescue” is a concern that impacts patient safety and promotes patient morbidity and mortality from an iatrogenic etiology related to medical errors. The question with justification from a case study, presented in this short communication for reader consideration, is, why are patients “failing to be rescued” by HCPs?
As the provision of health care becomes more complex, there is evidence that a patient’s passage through the health care system, can be problematic. This is particularly so when healthcare professionals, promote failure to rescue occurrences, which affect the quality of care and subsequently patient safety. Patient safety and high quality of care are essential aspects of all healthcare practices. When people are admitted to hospital, they expect to have their illness or disease treated effectively, and to receive safe, high-quality care. They do not expect to be put at risk or be harmed [15]. The primary goal of healthcare is to maximize safety and wellbeing, and so optimize the quality of people’s lives [16,17].
Risks to patient safety can be in the spheres of the ‘task’ or the ‘team’, or in terms of ‘situational’, ‘organisational’ or ‘institutional’ factors [18,19] Origins of incidents are multifaceted and can be embedded in factors such as insufficient training, ineffective communication or information disparities, equipment design, management systems and work processes [5]. The IOM report (2000) ‘To Err Is Human: Building a Safer Health System’ generated subsequent questions about patient safety and an obligation for healthcare providers to deliver high quality, safe healthcare [20,21] Over the last 20 years, this assurance has been a strategy and policy target for healthcare organizations around the world. The Joint Commission International (JCI) is one such organization that labors to improve patient safety and quality of care for the international community. However, despite the awareness which was created by the IOM report and strategies by organizations such as JCI; patients continue to experience preventable harm and substandard care [16,22]. Disturbingly, Makary and Daniel, (2016), concurred that the medical errors were still prevalent and stated that they were the third leading cause of death in the USA, after heart disease and cancer [23].
However, despite the 2 decades since the IOM report (2000), the strategies and policy targets to address preventable harm and substandard care by international healthcare organizations appear to have remained ineffective, with patient harm in healthcare deemed as severe or life-threatening [24]. Which as Makary and Daniel, (2016) stated continues to make medical error the third leading cause of death, after cancer and cardiovascular disease [23-25].
The concept of “rescue” has conventionally been associated with surgical patients and the need to recognize and treat postsurgical problems successfully [26]. Numerous of the ethics of rescue, such as advocacy, quality, safety, early recognition, teamwork, communication, organizing, and culture apply to all patients generically [27,28].
In contrast, “Failure to rescue” then, is the inability to prevent a clinical deterioration, such as death or permanent disability, from a complication of an underlying illness or a complication of medical care and was first defined in a study that examined competence when managing complications after surgery [29]. It is considered an indication of the quality of care and presumes that, while complications may reflect both, the severity of the patient illness and the associated health care factors [30]. The ability to “rescue” patients once problems arise is intimately associated with the quality of health care being provided. Sub-standard care, and risk incidents are often associated with “failure to rescue” situations [31]. One such “failure to rescue” and risk incident relates to non-compliance by healthcare professionals when verifying and documenting accurate and truthful equipment checks on “crash carts” [32]. Failure to do so, not only compromises patient safety, but also creates the potential to harm patients. Research into the causes of “failure to rescue “reveals the intricacy of the problem, with parallels that reflect acumen into contextual facets such as organisational failure, deficiency of knowledge and skills, a deficit of supervision and inadequate staffing levels which together with excessive workloads created time demands for healthcare providers making it problematic to prioritise their responsibilities [33]. To comprehend the magnitude of “failure to rescue” in the context of life support, emergency situations and accurate and truthful equipment checks on “crash carts”, the concept of a crash cart and associated prerequisites will be explained.
Simply, a crash cart is a mobile filing cabinet on wheels that contains all the equipment and medications required for an emergency cardio-pulmonary resuscitation. They are typically individualized and segregated for pediatric and adult populations. Crash carts are conveniently located throughout healthcare facilities so that they can be accessed rapidly in the event of an emergency.
A crash cart is typically located in a setting where a patient may unexpectedly experience a medical emergency. This could include, a severe allergic reaction, cardiac or respiratory arrest, or both, and conditions with an unexpected sudden deterioration of vital signs. This would require equipment and medications located on and in the crash cart which would be provided by a credentialled life support provider, such as the American Heart Association. While crash carts can vary depending on their location, operating theatre, emergency department, ICU, clinics, and the population, neonatal, pediatric, adult, geriatric, the fundamentals for the crash cart will contain similar equipment and medications.
Although the organization of requirements for a crash cart is not generic, this is an example, as there is a fundamental standard which provides effortless access to emergency medical equipment and medications. Note that all these organizational points are checked, dated, and signed by the staff member who performed the daily routine inventory and inspection.
The top section of all crash carts typically has the most frequently used equipment employed in a resuscitation event such as the following
The sides and back of the crash carts are typically allocated the following equipment, but can vary depending on the setting
RCUK 2022, AHA 2021: Follow manufacturer guidelines on use of the organization’s equipment.
RCUK 2022, AHA 2021: Follow organizational guidelines for medications.
RCUK 2022, AHA 2021: Follow organizational guidelines for crash cart maintenance
The purpose of a “crash cart” inventory is to organize a schedule of when to check for expiration dates of equipment, supplies and medications, and as such to replace items as required (Figure 1).
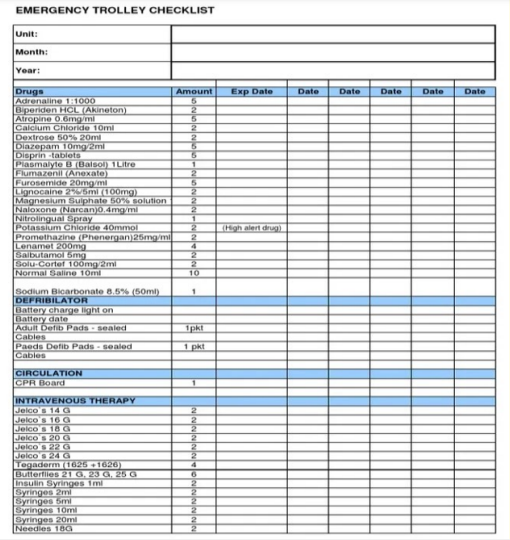
Figure 1: Example: Crash cart inventory.
Also, to check that equipment if operating as required in the event of an emergency. In addition to recording who performed the inventory checks, with dates, times, and signatures. There should also be a record of what was replaced and when. An alarming situation for healthcare personnel requiring a “crash cart” is to find unusable equipment or expired medications in an emergency. Ensuring that an up-to-date, accurate, and truthful inventory record can avoid potential patient safety situations such as absence of equipment such as laryngoscope blades or handles, equipment failure due to expired batteries, expired or missing medications, empty oxygen cylinders.
As stated previously, the objective of this short communication is to highlight the patient safety risk incident which relates to “failure to rescue” which is perpetrated by healthcare professionals when they do not check a “crash cart “accurately. In the hospital setting, standards for checking may vary, but are governed by hospital policy and procedure. Failure to do so, not only compromises patient safety, but also creates potential to harm patients, as underscored by the Patient Safety Authority, (2010), who revealed that contributing factors to patient safety and crash carts included, but were not limited to missing, expired, damaged, contaminated, and unavailable equipment and/or medications, empty or defective oxygen tanks, depleted batteries on equipment or equipment failure, unsecured carts or carts that had been tampered with, incorrect size of equipment, which ultimately indicated that crash carts were not checked, inspected or documented according to organizational policy and procedure which resulted in delays getting equipment and medications and as such “failure to rescue” [3,5].
The “failure to recue” dilemmas which will be reviewed in the following 2 case studies illustrates events that placed both patients at risk. The case studies focus on the reality that health-care professionals [HCP] are provided with knowledge, such as organizational policies and procedures for “crash cart” checking which can be simplified and called “Theory” and HCP are also required to demonstrate competence and organizational compliance, with check lists before allocated this routine, yet critical task, which can also be made simpler and called “Practice”. However, HCP continue to sponsor an attitude of non-compliance or unethical practices which create “failure to rescue” medical errors and place the patients’ safety at risk [1,2,15,31,32].
A 10-year-old male child was brought into the emergency department (ED) of a hospital in the Middle East by his parents. The father informed the nursing staff that his son had been sick with a persistent cough and fever for 3 days. The ED nursing staff documented following concerning observations and vital signs: The child was alert, anxious, had a fever with a core temperature of 38.8 °C, rigor-like shivering, tachypnea 32 breaths/minute, a pulse rate of 115 beats/minute, SpO2 88% on room air, chest retractions, shallow breathing, and was fatigued. During the succeeding history-taking by the ED physician, when asked about allergies, the father stated that his son did not have any allergies. The allergy status, no known allergies (NKA) of the child was documented in the child’s hand-written and electronic medical records.
Subsequent laboratory investigations included, nasopharyngeal bacterial swabs, blood cultures, and a complete blood count, which highlighted a high white cell count of 14000/mm³; neutrophils 70%, bands 15%, lymphocytes 15%. An anterior-posterior chest X-ray was also recorded (Figure 2). The child was commenced on oxygen therapy, which elevated the SpO2 to 94% and was subsequently transferred to the pediatric intermediate care ward (PICW) for specialist care, close monitoring, and the commencement of prophylactic antibiotic therapy.

Figure 2: Right middle lobe pneumonia.
The physical examination on admission to the PICW, disclosed that the child was now drowsy, had a pulse rate of 128 beats per minute, a blood pressure of 115/63mmHg, a respiratory rate of 48 breaths per minute with associated shortness of breath, and an SpO2 of 90% on oxygen 40% non-rebreather mask. Pulmonary auscultation revealed wheezing and decreased air entry on the right side of the chest. The chest X-ray confirmed right-sided middle lobe atelectasis and a possible diagnosis of pneumonia.
Once the child was settled, the PICW physician prescribed IV Amoxicillin as the antibiotic of prophylaxis until the culture and sensitivity report from the laboratory was available to commence a specific antibiotic regimen. The IV amoxicillin was prepared for administration and connected to the child’s IV site by the primary nurse caring for the child. Following the commencement of the IV amoxicillin, the child had an anaphylactic reaction, and the nurse could not get a response from him, the child was pulseless. The hospital emergency medical response was activated, a pediatric ‘code blue’ (PCB) was announced over the public address system and cardiopulmonary resuscitation (CPR) was commenced.
The “crash cart” was brought to the scene, the child was connected to the defibrillator’s ECG monitor by the nursing staff, and a sinus tachycardia, as pulseless electrical activity (PEA) was established (Figure 3).
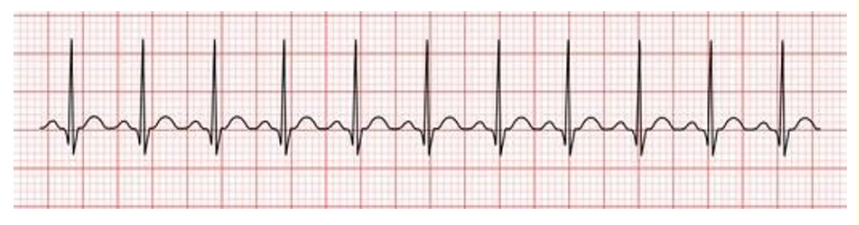
Figure 3: Sinus tachycardia with pulseless electrical activity (PEA).
The pediatric code team arrived within 2 minutes, and the team leader requested that CPR continue, then estimated the child’s weight at 30 kg, following which he prescribed IV Epinephrine 3 mils 1:10,000, to be given stat. However, the medication provider stated the ordered medication could not be given as there were no emergency medications in the crash cart. CPR continued until a medication tray was obtained, from another department, this required 10 minutes. When the medication tray arrived at the code scene, CPR was stopped and a rhythm check was performed, the child was now in asystole, and despite maximum attempts by the code team, the 10-year-old male child could not be resuscitated (Figure 4).
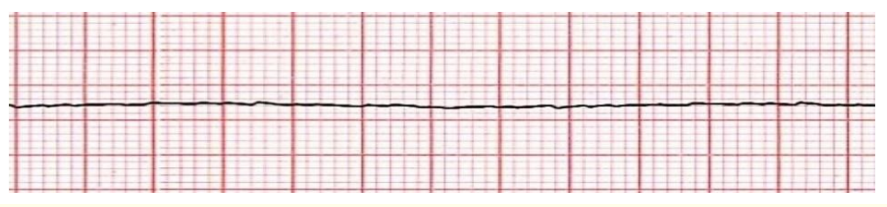
Figure 4: Cardiac asystole.
The CPR committee review board in the healthcare organization concerned, performed a multidisciplinary root cause analysis (RCA), to determine the events that contributed to the 10-year-old male child’s untimely death. Those events centered on, the missing medication tray on the crash cart, which caused the delay in the administration of IV Epinephrine ordered by the team leader, and a potential positive outcome for the child being resuscitated. Additional information obtained from the root cause analysis revealed that the “crash cart” had been checked that morning by the responsible staff member and all equipment, supplies and medications had been confirmed and checked as available and operating on the “crash cart” checklist.
The RCA recommendations from CPR committee review board were based on the frequency of an emergency occurring in a known clinical area, and the risk to patient safety associated with “failure to rescue”. The RCA findings related to the staff checklist knowledge and incorrect use, also the false documentation regarding the missing medication tray on the “crash cart”. These findings signified that staff were not adequately prepared to perform the crash cart check and required further training, as well as continuing education. In the opinion of the RCA committee, such staff training, when used effectively, creates responsibility and accountability among both clinical and nonclinical staff members and can encourage a positive and proactive team approach. In addition, periodically auditing checklists at scheduled intervals may also prevent the in incidence of faulty equipment, missing items, or outdated medications on “crash carts” and reduce “failure to rescue” situations.
This case study reveals two issues of major concern which relate to patient safety, the first a medical dilemma, which involved “failure to rescue” a patient due to missing emergency medications on the “crash cart” which had been checked and confirmed as available. The second, a conflict of professional ethics and a duty of care within a paradigm called the ‘theory-practice-ethics gap”15 This paradigm acknowledges that all HCP are provided with theoretical knowledge (How, why and when to check the crash cart) and practical skills (How to check and document the crash cart), yet these same HCP continue to be ethically non-compliant with organizational policy and procedure which places patients in harm’s way. Without adherence to organizational policy when performing essential procedures such as a “crash cart” check, it creates a situation which promotes “failure to rescue” events and as such compromises patient safety. This case study also serves as a prudent reminder that everything we do to or for the patient has potential complications associated with it. Ultimately the goal of all professional HCP is to provide safe, evidence-based quality care because all patients regardless of their religion, race, culture, age, or gender are entitled to safe, quality care.
Healthcare has consistently treated medical errors as deficiencies on the part of individual providers, which have exposed inadequate knowledge or skill. The modern field of systems analysis that was pioneered by the British psychologist James Reason, whose analysis of errors revealed that safety failures are almost never caused by isolated errors committed by individuals. Instead, most accidents result from multiple, smaller errors in environments with serious underlying system flaws. [36].
Reason introduced the Swiss Cheese model to describe this phenomenon, errors made by individuals result in outcomes due to flawed systems, the holes in the cheese, not by individuals (Figure 5) The model compares human systems to layered slices of Swiss cheese, that are stacked side by side [36]. In the Swiss cheese model, an organization's defenses against failure are modeled as a series of barriers, represented as slices of cheese. Holes in the slices represent weaknesses in individual parts of the system and are continually varying in size and position across the slices. The system produces failures when a hole in each slice momentarily aligns, permitting "a trajectory of accident opportunity", so that a hazard passes through holes in all of the slices, leading to a failure [37] Although the Swiss cheese model is respected and considered to be a useful method of relating concepts, it has been subject to criticism that it is used too imprecisely [44]
![Figure 5: The Swiss Cheese model (Reason 2000) [37].](https://actascientific.com/ASPE/images/IJMCR/ASPE-05-0540-fig5.PNG)
Figure 5: The Swiss Cheese model (Reason 2000) [37].
Since the IOM report “To Err is Human”: Building a safer health system [6], it is accepted that medical errors cannot be eradicated and therefore the emphasis is on moderating the impact [6,8,9,33,38].
Which endorses Reason’s fundamental conjecture was that human error is inevitable, especially in systems as complex as health care, and to expect a faultless performance from human beings in multifaceted, high stress setting such as healthcare is unrealistic. However, it is the author’s belief that in an idyllic world, healthcare would happen in a highly reliable system where no one is hurt, and everyone gets the care they need. But, in reality, patients continue to be harmed with the experts opting out by stating that “we're all human” and, of course, to “Err is Human” [39-43].
In actuality, health-care professionals [HCP] are provided with evidence-based healthcare information, such as organizational policies and procedures, and are expected to demonstrate evidence-based practice [EBP] which validates competence and organizational compliance [15]. Evidence-based healthcare practices, ensures patient safety, and prevents potential patient harm [44]. There are no routine medical procedures in healthcare, every intervention could place the patient at risk and/or in harm’s way. This case study involved a 10-year-old boy who was “failed to be rescued”, a child who could not be resuscitated due to missing emergency medications on a “crash cart” which had been previously certified as “dependable” by the HCP who was deemed to be trustworthy, a patient advocate. The patient in this case study was a 10year-old boy who was taken an ED in a Middle eastern general hospital by his parents. He was anxious, and probably scared because he was seriously ill and could not breathe effectively. Once admitted to the hospital, the author speculates that the patient and his parents were comforted and reassured that the hospital would provide the required care, endorsed by the ethics of rescue. Those ethics being, advocacy, quality, early recognition, teamwork, communication, organizing, and a culture of safety which applies for all patients generically [27,28]. However, following the patient admission to the hospital, a medical and an ethical dilemma occurred that involved an event of “failure to rescue” where the patient could not be resuscitated due to missing emergency medications which were supposed to be available on the “crash cart”.
In a perfect world, health care would occur in an exceedingly reliable system where no one is hurt, and everyone receives the quality care they need. But, in reality, patients continue to be harmed with the academics choosing to state that ‘We’re all Human’ and ‘To Err is Human’.
Health care miscalculations, medical errors, blunders, oversights, booboos, faults, or slip-ups, whatever term attached to these patient safety consequences. The concept of a “theory-practice-ethics gap”, recognizes that HCPs are prepared with theoretical knowledge and realistic skills to practice competently and safely. However, HCP continue to be non-compliant towards patient safety issues which is an ethical dilemma. An obligatory objective for HCP is to deliver safe, evidence based high quality care. Why? Because all patients, no matter what their race, culture, religion, gender, or age are entitled to be provided with safe, high-quality care. Measures must be taken to inspire and urge HCP to reflect on their ethical behaviors, and to eliminate this ‘theory-practice-ethics gap’. If we as HCPs and patient advocates don’t care or act ethically, who will. Only by creating a culture of ethical care can we hope to decrease morbidity and mortality from medical error.
Do onto others as you would have them do unto you; Jesus Christ (Matthew 7:12)
For this short communication and case study, formal consent was not required, as it does not identify the organization, or the individuals involved.
The author declared no conflicts of interest in respect to authorship, and/or publication of this article.
Copyright: © 2022 Manfred Mortell RN. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.