Kahra Christy E Jumawan, Anabella S*, Maribeth M Jimenez and Joy A Bueno
Department of Pediatric Medicine, Government Celestino Gallares Memorial Hospital, Philippines
*Corresponding Author: Anabella S, Department of Pediatric Medicine, Government Celestino Gallares Memorial Hospital, Philippines.
Received: March 24, 2022; Published: June 13, 2022
Citation: Anabella S., et al. “Suicide Ideation and Behavior Among Adolescents Admitted in Governor Celestino Gallares Memorial Hospital in the Midst of the Covid-19 Pandemic”. Acta Scientific Paediatrics 5.7 (2022): 17-27.
Objective: To determine the incidence and risk of suicide ideation and behavior of adolescents admitted in Governor Celestino Gallares Memorial Hospital (GCGMH) in the midst of the COVID-19 pandemic.
Design: This is a descriptive cross-sectional study.
Participants: This study involved adolescents 10 to 17 years and 364 days who were admitted at the pediatric and surgical wards of GCGMH from November 11, 2020 to November 10, 2021 excluding those discharged against medical advice or per request, and those diagnosed with neurodevelopmental disorders. Total population enumeration was utilized.
Methodology: A one-on-one guided interview using the Columbia-Suicide Severity Scale (C-SSRS) screener version was conducted in a vacant room without the parents around after an informed consent from the parents and an informed assent from the adolescent were obtained. The interview was conducted on the day of patient’s discharge. The data that were gathered were duly recorded and tabulated.
Results: There were 7 out of 35 (20%) adolescents who wished to be dead. Suicidal thoughts were seen in 4 adolescents (57.1%) who wished to be dead. Of these 4 adolescents, 3 (75%) had thoughts of the method by which to commit suicide. Two of the 4 adolescents (50%) had suicidal intent without a specific plan and 2 adolescents had suicidal intent with a specific plan. All the 4 adolescents with suicidal intent had suicidal behavior (100%). Six of the 7 adolescents are girls 16 to 17 years old, and 1 was a 16-year-old boy. All the 4 adolescents with suicidal thoughts and behavior were girls. All these 4 adolescents were considered to have high suicide risk according to C-SSRS. All the other 31 adolescents were considered to have low suicide risk.
Conclusion: Suicidal ideation is seen in 20% of hospitalized adolescents during the COVID-19 pandemic. A vast majority of adolescents with suicidal ideation is females. Adolescents at high-risk for suicide are females aged 16 - 17 years.
Keywords: Suicide Ideation; Adolescents; Covid-19.
Suicide is the termination of one’s life. It most often results from an underlying mental illness [1]. The World Health Organization (WHO) reported that almost 800,000 people die from suicide annually. Suicide contributes more deaths than does malaria, breast cancer, or war and homicide. Such is the magnitude of the burden of suicide that the WHO prioritized the reduction of suicide mortality as a global target. Furthermore, suicide mortality rate was included as an indicator in the United Nations Sustainable Development Goals (SDGs) target 3.4 which is that by 2030, premature mortality from non-communicable diseases should be reduced by one-third through prevention and treatment and promotion of mental health and well-being [2].
In 2016, the age standardized suicide rate varies between regions. It is 12.0 per 100,000 population in Africa, 12.9 per 100,000 population in Europe, and 13.4 per 100,000 in Southeast Asia. The age standard suicide rate in the Philippines is relatively low at 3.7 per 100,000 population; however, in a country with approximately 108,000,000 population, this translates to approximately 4,000 suicides per year [3].
Suicide rates in children is known to be increasing nowadays. As reported by the National Center for Health Statistics, suicide is the second leading cause of mortality in childhood and adolescence. From year 2007 to 2017, suicide rate nearly tripled among children aged 10 to 14 years old and increased by 76% in adolescents aged 15 to 19 years old [4].
The suicide rate in the Philippines has augmented since the start of the new millennium. From year 2000 to 2016, suicide rate of Filipino males increased from 4.5 to 5.2 and from 1.8 to 2.3 in females. A total of 237 children aged 10 to 14 years committed suicide in 2016 [5]. A retrospective cross-sectional study on suicide in the Philippines reported that suicide is high in females and the most common method is chemical ingestion [6].
Suicide cases are likewise emerging in the province of Bohol. Based on the data obtained from the City Health Office in Tagbilaran City, six cases of suicide deaths among adolescents aged 10 to 17 years were recorded in 2019 wherein five of them were males and one was a female. In addition, there were six anecdotal suicide attempts in one of the public schools in Tagbilaran City, one of which was an 11-year-old female and five were 11-year-old males. The manner of suicide attempts was wrist incisions using a paper cutter. The common factor among these children was family problem, specifically parental infidelity.
There is no specific cause that can be singled out as the etiology of suicide. It may be a product of a mental disorder, i.e., depression, ADHD, aggression, or parental psychopathology, relationship problem, and abuse [1,7]. Studies conducted in both developed and developing countries revealed a prevalence rate of 80 to 100% of mental health problems among individuals who successfully initiated suicide. Moreover, a lifetime estimated risk of suicide in persons having a mood disorder is 6 - 15%, those with alcoholism is 7 - 15%, and in persons with schizophrenia is 4 - 10% [8]. Suicide has been linked to poverty in a research conducted by the Boston Children’s Hospital. Data showed a 37% increase in suicide rate among children and adolescents in countries with high poverty level [9].
Data regarding childhood suicide is scarce because it is presumed that children are not capable of killing themselves [10]. Suicide occurs in susceptible children usually resulting after a brief period of stress most likely triggered by family and school problems. It is possibly due to cognitive immaturity and age-related impulsivity [11].
The coronavirus disease (COVID-19) pandemic impacted almost every individual’s daily life. The call for social and physical distancing imposed a major disruption especially on adolescents who are in that developmental period when social relationships are quite important [12]. Several studies have reported the negative impact of COVID-19 pandemic on the mental health of children. It was reported in an article written by Joyce Lee that in Hongkong, 20% of secondary education students who were surveyed claimed that their stress level was at maximum 10/10. The stress arose from uncertainties on whether the exams will proceed or be postponed, the fear of contracting the virus and inability to take the exam, and even from the thought of staying healthy [12]. Leeb., et al. reported that emergency room visits for mental health reasons in the United States have increased by 24% in children 5 to 11 years old, and by 31% in adolescents 12 to 17 years of age from April to October, 2020 [13]. In another study on adolescents in the United States, it was reported that in February 21 to March 20, 2021 emergency room visits for suspected suicide attempts increased by 50.6% among girls aged 12 to 17 years, and by 3.7% among boys 12 to 17 years old [14]. The increased statistics may be a reflection of how the COVID-19 pandemic disrupts a multitude of intersecting domains that include academic, interpersonal, financial, and health [12]. This translates to loss of meal access, academic instruction, social interaction, and more importantly mental health services [15]. Intrafamilial violence, and overuse of the internet and social media and consequent rise in psychiatric disorders may also partly explain the high statistics [16].
What is notable is around 83% of children attempting suicide are not recognized by most of the healthcare providers, and screening for suicide risk is not routinely done at the outpatient department or in hospital settings. To date, there are several screening tools to evaluate risk of suicidal thoughts in children that can be utilized in schools, clinics, and hospitals. It is the most effective strategy for early identification and prevention of suicide [17]. Suicide is also included in the psychosocial assessment of adolescents during history taking of physicians at the Emergency Department using the HEADSSS assessment tool which stands for Home, Education/Employment, Activities, Drugs, Sexuality, Suicidality, and Safety [18]. Other screening tools specific for suicide include Suicide Assessment Five-Step Evaluation and Triage (SAFE-T), Ask SuicideScreening Questions (ASQ), Patient Safety Screener (PSS-3), and the Columbia - Suicide Severity Rating Scale (C-SSRS) [19].
The Columbia - Suicide Severity Rating Scale (C-SSRS) was created by the researchers of Columbia University, University of Pennsylvania, University of Pittsburgh, and New York University. It is one of the simplest tools used for initial screening or as part of a full assessment. It is supported by the National Institute of Mental Health (NIMH) and is available in 103 country-specific languages which include a Cebuano translation. Training is recommended before administering the tool except for those who are in clinical practice [20]. This tool has been successfully implemented in various institutions including schools, clinical areas, military, fire departments, justice system, and scientific research. It has four versions, namely, Lifetime/Recent version, Since Last Visit version, Screener version, and Risk Assessment Page. This can be used in different age groups including the very young children. There are six areas that are asked in the tool and include (1) wish to be dead, (2) suicidal thoughts, (3) suicidal thoughts with method, (4) suicidal intent without specific plan, (5) suicidal intent with specific plan, and (6) suicide behavior. The level of suicide risk is identified according to the participant’s response to the questionnaire. The participant is considered high risk if he answers “yes” to questions 4, 5, or 6; medium risk if he answers “yes” to question 3; and low risk if he answers “yes” or “no” to questions 1 or 2 and “not” to question 6 [21]. The C-SSRS is a comprehensive measure of suicidal ideation and/or behavior. It has already been used by previous researchers and they have found an increased predictive validity for suicidal behavior [22,23]. The data gathered can be used as comparison in both research and clinical populations which show trends over time and will serve as guide for the treatment regimen and suicide prevention strategies [24].
Suicide in children is a highly sensitive topic. However, it is an issue that needs to be addressed because suicide death is tragic but is highly preventable. Questions about suicide ideation or suicide plan does not provoke the person to perform a suicide act [25]. Furthermore, the knowledge about the children gained after screening them for suicide, and the knowledge imparted to them about suicide prevention can in fact result to less suicide behaviors [26].
Due to the conservative culture of Filipinos, limited studies have been conducted on suicide in the Philippines. To address this research gap, the authors tried to identify and address the alarming issue on suicide in the pediatric population using the Columbia - Suicide Severity Rating Scale (C-SSRS) Screener version.
This research aimed to benefit the following
This study embodies the institution’s vision and mission to become a premier research facility in Region 7. The data gathered in this study will serve as a steppingstone for future research. This will also increase the awareness of those who are working in the hospital regarding mental health.
This study will help the clinicians to become aware of the existing mental health problem and will serve as a guide in identifying children at risk for suicide. This study will also fortify the department’s commitment to help the pediatric population, not only with physical health but also with mental health.
The study will help identify adolescents who are at risk for suicide. This will promote early referral to proper channels and provision of treatment.
To determine the incidence and risk of suicide ideation and behavior of adolescents admitted in Governor Celestino Gallares Memorial Hospital.
Specific objectives
Operational definition of terms
To promote objectivity and eliminate possible factors that could influence the child’s answer, the researcher conducted the one-onone interview prior to the adolescent’s discharge to ensure that the child has sufficiently recovered from the disease condition and is already in good physical and mental health. The interview was conducted in a vacant room available in the pediatric or surgical ward without the parents or guardian around.
Voluntary participation was assured. An informed consent was sought from either parent or from the de facto guardian in cases where both parents are absent or not the one taking care of the child. The parents or guardian were provided with the questionnaire for them to know the content and to help them decide whether they will allow the child to participate in the study or not. Aside from the informed consent, an assent was also obtained without coercion from the child himself. Information regarding the study was explained in the simplest manner for the child to fully understand. The child was given the liberty to refuse to participate and to discontinue participation at any time.
Confidentiality and anonymity were upheld. However, if the patient was at risk of harming himself, the researcher was obliged to take the necessary action to prevent harm. The mother was informed of the child’s risk and a referral to the psychiatrist was done for prompt intervention. The psychiatric consultation fee was waived as the psychiatrist was one of the co-authors of the study.
The study commenced on November 11, 2020 and ended on November 10, 2021.
After the approval from the hospital Technical Review Board (TRB) and the Institutional Review Board (IRB) was granted, the researcher started to gather data. Recruitment was facilitated by reviewing the daily admissions for adolescents admitted to the pediatric and surgical ward. These patients were followed up daily for the possibility of discharge. Once a discharge order was made by the resident-in-charge, the researcher approached the parent or the guardian initially to explain the study, gave them a copy of the questionnaire and asked for an informed consent. Once an informed consent was given, the researcher then approached the adolescent to explain the study to him and to ask for an assent.
Once the adolescent gave his assent, the researcher provided him with both the English and Cebuano version of the C-SSRS questionnaire and asked him to choose the version he was comfortable with. The researcher then conducted a one-on-one interview with the adolescent using the questionnaire that the adolescent chose in a vacant room available in the pediatric or surgical ward in the absence of the parent or the guardian. The questions were answered by either a “yes” or “no”. The researcher asked the first and second question successively, regardless of the answer to the first question. If the answer to question 2 is a “yes”, the researcher proceeded to ask questions 3, 4, 5, and 6. If the answer to question 2 is a “no”, the researcher went to ask question 6 directly. The responses to the questions were used to assess the suicide risk of the adolescent basing on the criteria mentioned in the C-SSRS.
The data gathered were duly recorded and tabulated.
There were 135 adolescents admitted at the pediatric and surgical ward of Governor Celestino Gallares Memorial Hospital from November 11, 2020 to November 10, 2021. All 135 adolescents are non-COVID-19 patients. Of these, only 35 were eligible for inclusion in the study and gave consent.
Table 1 shows the sociodemographic profile of the subject population. There are no adolescents aged 10 years old who were admitted during the study period. The majority of the admitted adolescents are 16 years of age, accounting for 31.4% of the subjects. Female adolescents accounted for 54.3% and male adolescents for 45.7% of the subject population.
Figure 1 shows the distribution of adolescents with or without suicide ideation and behavior. Out of 35 adolescents interviewed, 7 (20%) wished to be dead, and the remaining 28 (80%) did not have any suicidal ideation or behavior.
Figure 2 shows the distribution of adolescents with suicidal ideation. There were 4 (57.1%) of the 7 adolescents who wished to be dead that had suicidal thoughts. Of these, 3 (75%) had thoughts of the method by which they would commit suicide. Two of the adolescents with suicidal thoughts had suicidal intent without a specific plan (50%), and 2 (50%) had suicidal intent with a specific plan. All the 4 adolescents with suicidal intent had suicidal behavior (100%).
Table 1: Sociodemographic Profile of Adolescents Admitted in GCGMH.
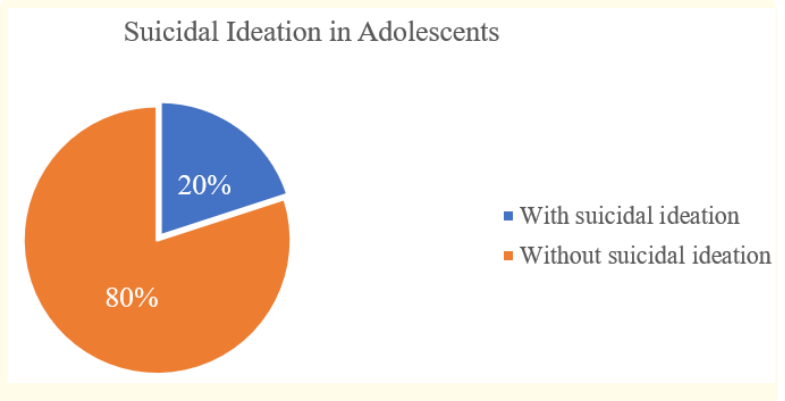
Figure 1: Distribution of Adolescents with Suicide Ideation.
Table 2 shows the responses of the adolescents admitted in GCGMH to the questions in the Columbia-Suicide Severity Rating Scale (C-SSRS) in relation to the sociodemographic profile. Six of the 7 adolescents who wished to be dead are girls 16 and 17 years old, and 1 was a 16-year-old boy. All the 4 adolescents who had suicidal thoughts, suicidal intent with or without plan, and suicidal behavior are girls. One of these is a 16-year-old, and the remaining 3 are aged 17 years.
Figure 3 shows the distribution of suicide risk among adolescents admitted in Gov. Celestino Gallares Memorial Hospital. Based on the C-SSRS criteria, all 4 (11.4%) adolescents who had suicidal thoughts, intent and behavior are considered high risk.There is no adolescent who is at medium risk for suicide. All the rest of the adolescents interviewed in the study are at low suicide risk.
Table 3 shows the suicide risk of adolescents admitted in Governor Celestino Gallares Memorial Hospital according to sociodemographic profile. All the adolescents considered high risk based on the C-SSRS are females aged 16 and 17 years old.
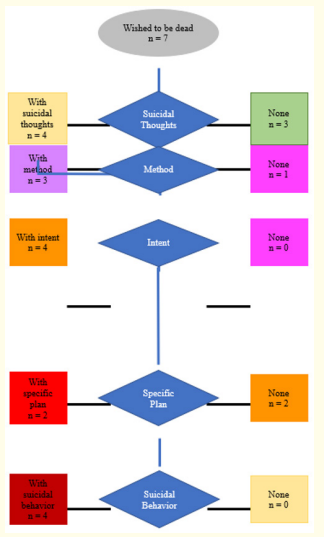
Figure 2: Distribution of Adolescents with Suicidal Ideation and Behavior According to C-SSRS.
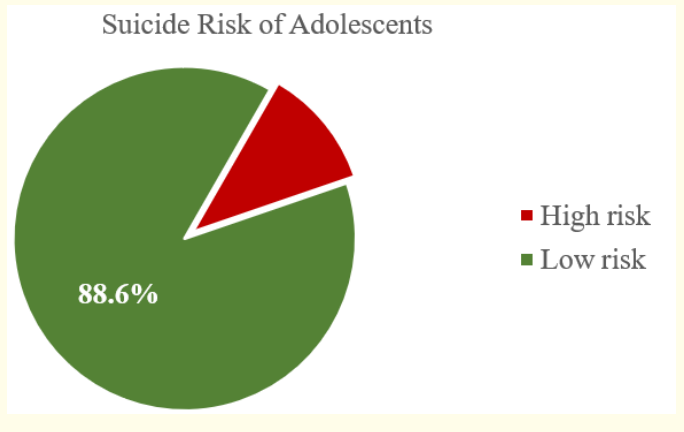
Figure 3: Distribution of Suicide Risk of Adolescents Admitted in GCGMH.
This study shows that the prevalence of suicidal ideation in hospitalized adolescents is 20%. This is much higher than the World Health Organization (WHO)-reported suicidal ideation prevalence rate of 11.6% among Filipino adolescents 13 to 17 years old [31]. The difference in the prevalence rates may be attributed to the subject population and the number of subjects in the study. This study is conducted in hospitalized patients and included a small number of adolescents while the WHO survey was conducted in school-aged children and involved a total of 8,761 students. A review of the prevalence of suicidal ideation from studies conducted in other countries provides a comparison against the result of this local study. Countries with a lower suicidal ideation prevalence include Brazil (14%) [32], Guyana (18.4%) [33], and Thailand (8.8%) [34]. In contrast, Zambia has a higher suicidal ideation prevalence rate of 32.2% among adolescents [35]. The differences in these statistics may lie mainly on the differences of subject population. Data from countries abroad are gathered from studies on school-aged children before the COVID-19 pandemic while this local study is on school-aged children during the COVID-19 pandemic.
Table 2: Suicidal Ideation and Behavior According to Sociodemographic Profile of Adolescents.
There is a scarcity of literature on the incidence of suicidal ideation and behavior among adolescents admitted for non-psychiatric problems before and during the COVID-19 pandemic. Most studies that can be found are report on emergency room encounters and hospitalizations for psychiatric disorders. For instance, in Korea, 23.7% of adolescents 18 years and younger who have psychiatric problems visited the emergency room at least once for suicidal attempts and/or non-suicidal self-injury [36]. This incidence is notably close to that found in our own subject population. It is surprising considering that the Korean study was conducted on adolescents with psychiatric problems while this local study was conducted on non-psychiatric adolescents. In the United States, a cross-sectional study that utilized the National Hospital Ambulatory Medical Care Survey (NHAMCS) Emergency Department database reported that from 2007 to 2015, 2.8% of emergency room visits by children younger than 18 years old were for suicide attempts and/or suicide ideation [37]. In a study conducted in another emergency room in the United States by Horowitz., et al. it is reported that 5.7% of children who visited the emergency room in for non-psychiatric complaints reported clinically significant suicidal ideation [38]. The varying degrees of discrepancy between these international studies and this local study may be due to the differences in the sample population. The Korean study had 194 subjects, the US NHAMCS study had 59,921 cases of emergency room visits, and the Horowitz study had 106 patients. Nevertheless, these studies have highlighted the important role of the Emergency Room as a screening venue for suicidality.
The COVID-19 pandemic has imposed a background filled with stressors that triggered concerns about the potential increase in suicide rates. Stressors include social isolation, economic stress, inaccessible mental health care, interpersonal conflict, and reduced access to religious and community support have been identified to increase the risk for suicide [39]. A survey on adolescents admitted to a psychiatric inpatient unit in the US reported that 47.2% claimed to have suicidal ideation in relation to COVID-19 [12]. This incidence is quite high compared to that seen in the local study; however, it is not also surprising considering that the subject population is composed of adolescents with psychiatric problems. Mayne and colleagues conducted a cross-sectional analysis of electronic health record data from the Children’s Hospital of Philadelphia (CHOP) primary care network. The electronic health record data are from all preventive visits by adolescents aged 12 to 21 years from June 1, 2019, to December 31, 2020. In their study, they found that there are more adolescents positive for depressive symptoms during the pandemic (6.2% vs 5.0%), and that there is a higher positive suicide risk screens in 2020 (7.1%) than in 2019 (6.1%) [40]. These results give weight to the concern about COVID-19’s impact on the mental health of adolescents.
Passive suicidal ideation, characterized by the wish to be dead, accounted for 7 (20%) cases of suicidal ideation and is the most common type of suicidal ideation reported in the subject population. However, 4 (57.1%) of these adolescents with passive ideation also reported non-specific active suicidal thoughts. These results are similar to those reported by Estrada., et al. in their study conducted on adolescents enrolled in the Alternative Learning System in Manila (ALS). In their ALS study, passive ideation is also the most frequently reported type of suicidal ideation among adolescents enrolled in ALS [41]. Burke., et al. conducted a survey on 143 adolescents admitted to a psychiatric inpatient unit in the US to investigate the presence of suicidal behavior by means of intentional COVID-19 exposure as well as the incidence of passive and active COVID-19 specific suicidal ideation. They reported that COVID-specific passive suicidal ideation predominates over COVID-specific active suicidal ideation (38.8% vs 23.1%) [42] just like the results of this local study.
Adolescents aged 11 to 15 years exhibited no suicidal ideation or behavior in contrast to adolescents 16 to 17 years old. This result affirms the finding of the ALS study which also reported that adolescents aged 16 to 17 years are more likely to hold suicidal ideation [41]. The preponderance of suicidal ideation in older adolescents has also been shown in a US study on emergency and inpatient encounters for suicidal ideation and suicidal attempt. In this study by Plemmons and colleagues, it is reported that the highest increase in the annual percentage of all visits for suicidal ideation and attempt occurs in adolescents 15 to 17 years old [43]. This propensity of suicidal ideation in older adolescents which is also the pattern seen for acts of suicide may be partly explained by increased psychosocial stress [44] as well as higher prevalence of mental health problems [45] in older adolescents. Moreover, younger children and early adolescents may not yet be able to fully comprehend the concept of death [46]; this may also partly explain why the younger adolescents showed no suicidal ideation or behavior.
This study shows that 6 out of 7 adolescents with suicidal ideation are females. This female preponderance is also reported by Campisi., et al. [47] and by Sadanand, Rangiah, and Chetty [48]. Additionally, this study also shows that adolescents who had active suicidal thoughts and behavior are all females who are 16 and 17 years of age. This is similar to the findings in the study conducted by Zygo., et al. in Eastern Poland. In this Polish study, there is a significant proportion of girls than boys who had suicidal thoughts and plans as well as suicide attempts (p =< 0.001) and the largest group of these female adolescents with suicidal ideation are aged 17 to 18 years [49]. The female predominance in terms of suicidal ideation and behavior has been reported in a cross-sectional study by Ridout., et al. to be existing even before the COVID-19 pandemic [50]. The higher incidence of suicidal ideation among females is congruent with the phenomenon called gender paradox of suicidality wherein suicidal ideation and behavior are higher in females than in males but the suicide mortality rate is lower in females than in males [51]. Kaess., et al. attempted in their study to explain why suicidal ideation is more prevalent in older female adolescent. They found out that female adolescents showed higher levels of internalizing problems, i.e., depressive disorders, anxiety disorders, or somatic complaints, compared to male adolescents, and are more likely to show auto-aggressive manifestations [52]. This may be related to the significant difference in the emotional development among same-aged female and male adolescents. In a study by Cyranowski., et al, the mechanisms by which changes in circulating gonadal hormones during puberty, as well as social mechanisms, increase the affiliative needs for pubertal females are discussed. Furthermore, how the interaction between the increased affiliative need and the transition difficulties during adolescence creates a predisposition to depression in at-risk females is also discussed [53]. Other authors support the theory that females are more likely to cogitate about the difficulties they encounter and this may cause gender differences in internalizing problems [54]. Another theory to explain the gender-gap in psychopathology is postulated by Schneider., et al. who found that there is sex-dependent lateralization of amygdala activation that suggests a sex-dependent differences in human emotion processing [55].
There are 4 high-risk adolescents seen in this study. These are adolescents who harbor suicidal thoughts and show suicidal behavior. All these adolescents were referred to and attended by a psychiatrist. In the study by King., et al, 16% of adolescents aged 13 to 17 years who sought pediatric and psychiatric emergency services screened positive for elevated suicide risk. Furthermore, 98% of these adolescents with suicide risk reported severe suicide ideation or a recent suicide attempt. Nineteen percent of these adolescents visited the emergency room for nonpsychiatric reasons [56]. This highlights the need for a stronger advocacy for suicidality screening and prevention. This is very important because according to Nock and colleagues, a large proportion of adolescents with a lifetime history of suicide ideation and attempt meet lifetime criteria for at least one of various DSM-IV disorders that include fear/ anger disorders, distress disorders, disruptive behavior disorders, and substance abuse [57]. Thus, a comprehensive investigation on the suicidal ideation of an adolescent may lead to the discovery of an underlying mental health problem and the treatment of such may help in the prevention of suicide. Suicidality screening is also important because studies by Mars., et al. [58], and Scott., et al. [59] reported that individuals who reported both suicidal thoughts and non-suicidal self-harm at baseline are more likely to make a suicide attempt.
Suicidal ideation is seen in 20% of hospitalized adolescents during the COVID-19 pandemic. A vast majority of adolescents with suicidal ideation is females. Adolescents at high-risk for suicide are females aged 16 - 17 years.
One of the major limitations of the study is the reduced number of admitted patients in Governor Celestino Gallares Memorial Hospital during the COVID-19 pandemic. It is recommended therefore to conduct a related study that will involve a broader population that includes healthy children, children attending face-to-face schooling, teenaged mothers, and children seen in the Women and Children Protection Unit (WCPU). Since children per se, and teenaged mothers as well as children in the WCPU are vulnerable subjects, the highest level of ethical consideration should be provided and followed. Another way to broaden the subject population may be the conduct of a multicenter study.
A study on the predisposing factors to suicidality may be conducted in the future. Data such as residence, socioeconomic status, level of education and family dynamics may be included to establish a possible correlation on the risk of suicide. This will help in the creation and establishment of policies that can prevent suicide.
Screening of children coming into the Emergency Room may be a good practice to establish. It has been shown by previous studies that it is feasible and acceptable to both parents and adolescents.
Needless to say, the utmost care to uphold anonymity and confidentiality should be observed. This practice can help the pediatricians to catch adolescents with suicidal ideation and behavior earlier and enable them to refer these adolescents to experts so that appropriate intervention may be performed early on.
There is a stigma on suicide. This was palpable during the preparation of this research proposal. This may partly explain the dearth of studies on suicide ideation and behaviors among pediatric patients despite the increasing incidence of suicide cases. It would be best if the Department of Pediatric Medicine could promulgate and implement programs or activities that will break the stigma and promote open discussion about suicide and provide an environment conducive for help-seeking behavior, as well as easy access to mental health professionals that can help prevent the progression from suicidal ideation to behavior.
Copyright: © 2022 Anabella S., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.