Teresa Pinheiro*, Ana Torres Rebelo, Joana Monteiro and Teresa Caldeira
Department of Pediatrics and Neonatology, Centro Hospitalar de Entre-o-Douro e Vouga, Portugal
*Corresponding Author: Teresa Pinheiro, Department of Pediatrics and Neonatology, Centro Hospitalar de Entre-o-Douro e Vouga, Portugal.
Received: March 21, 2022; Published: April 28, 2022
Citation: Teresa Pinheiro., et al. “Characterization of Frequent Users of a Pediatric Emergency Department in Level II Hospital and What Changed with the COVID Pandemic”. Acta Scientific Paediatrics 5.5 (2022): 42-48.
Before the COVID pandemic, the Pediatric Emergency Department (ED) had been experiencing a progressive overload due to an increasing of visits, but this high demand for emergency pediatric care does not always translate into serious conditions requiring hospital attendance. Frequent users, defined has having eleven or more admissions per year, are often associated with inadequate emergency visits. We performed a retrospective study of admissions to a Portuguese pediatric ED during the year of 2018, and we described the characteristics of its frequent users. The aim of this study was to compare the utilization of ED by the frequent users throughout 2018 and during the first year of the COVID-19 pandemic. In 2018, we identified 123 frequent users representing 1% of the patients that sought ED care and accounting for more than 5% of the total visits. In 2020, during the first year of the pandemic (from March 1st, 2020, to February 28th, 2021) we observed a significant reduction in all ED visits, as well as frequent users. The average age of patients changed significantly in the two periods (2,44 vs 4,65; p 0,000), with no gender differences. In both years, most children didn´t have a relevant pre-existing medical condition, but 45,5% frequent users in 2018 had a least one previous hospitalization, compared to just 26,5% of the frequent users in 2020 (p < 0,05).
To our knowledge, these are the first data on frequent user’s attendance during the pandemic compared to what happened previously. And if before we had a population of small children with inexperienced parents that don´t make the correct use of primary care, during the pandemic, anxiety and psychosomatic symptoms were predominant.
Keywords: Emergency Department; Frequent Users; Pediatrics.
CHEDV: Centro Hospitalar de Entre-o-Douro e Vouga; ED: Emergency Department; FU: Frequent Users; SSH: São Sebastião Hospital
In recent decades, there has been an overuse of emergency departments (ED), both for adults and pediatrics [1]. Despite a sustained decrease in the national birth rate [2], the use of the ED has not reduced accordingly. In fact, in many cases, it has increased [1,3]. This increasing demand for ED does not always translate into an increase in the number of acute conditions that require urgent or emergent attendance, but rather an increase in inappropriate or unnecessary visits, that don´t require hospital assistance and impose a significant clinical and economical pressure [1]. Published data associate frequent use of pediatric ED to accessibility and availability of medical care, absence, or little availability of adequate primary health care [1,3], low medical literacy [1], younger children [3,4], urban residence, history of chronic pathology, noncaucasian patients [3] and existence of a public health insurance [3,4]. However, most of these studies cannot be extrapolated to the Portuguese population, mostly because we have free accessibility to health care for people under 18 years old. Therefore, relevant differences in the characterization of the group of Frequent Users (FU) are expected. There is no consensus on the definition of an ED frequent user (FU). Some authors define a child with more than three to five visits to the ED per year [4-6], others with more than ten visits per year [8]. The importance of identifying the reasons for the recurrent use of the ED is not only the overconsumption of scarce resources but also to protect children with true emergencies from not being promptly treated. Understanding demographic and clinical characteristics of FU is essential to plan interventions aimed to improve health education. Public health policies should focus on the degree of severity of various conditions and what level of medical care to use. Additionally, existing resources in the community, such as primary care, must be easily accessible, specially during off-hours [9].
Initially, the aim of this work was to identify and analyze the clinical and demographic characteristics of the FU of our Pediatric ED, but then the Covid-19 Pandemic altered dramatically the affluence to health care services and so we decided to describe and compare the group of FU who visit the ED during the first year of the COVID pandemic.
CHEDV is a secondary medical center composed by three hospitals located in three neighboring cities in the north of Portugal (São Sebastião Hospital in Santa Maria da Feria, São Miguel Hospital in Oliveira de Azeméis and São João da Madeira Hospital in São João da Madeira). It serves a population of 274.859 inhabitants, of which 50.520 are under 18 years old (Census 2011). Only HSS has a differentiated Pediatric ED; the other two hospitals have a basic emergency ward whose medical care is provided by general practitioners.
We considered our population study all children who visited the Pediatric ED of CHEDV during de calendar year of 2018. The inclusion criteria were children from 0 to 17 years old that had at least one visit to the pediatric ED during that year. Trauma in children over 2 years old are evaluated by General Practitioners in the trauma area near the adult ED and were excluded from this study.
For our definition of FU, we used as cut-off the number of visits a patient made to the ED during the time under study exceeding the 99th percentile of visits.
Patients’ medical records were consulted, containing information from each emergency episode, including children’ age and gender, parents’ age, area of residence, medical history, place of regular follow-up and previous hospitalization in our Pediatric Department. Emergency episodes were analyzed considering reasons for visit, time since onset of symptoms, forms of referral and whether it was a first or a return visit. Episodes were classified as first observation; reassessment (if the medical staff decides that the patient should be reevaluated on the following days); or recurrence (if the patient decides to return to the ED because of persisting or worsening symptoms within a seven-day period). We also analyzed triage priority level, complementary diagnostic exams required, medication administered in the ED, need for other specialties consultation, discharge diagnosis and final patient destination (return to ED, hospital out-patient clinic or primary care referral).
We carried out a retrospective study of all the visits to the pediatric ED of a secondary care Portuguese hospital (São Sebastião Hospital) occurring from January 1st to December 31st, 2018, and selected a group of patients that made 11 or more visits to the ED. We then applied the same definitions of 99th percentile of visits and defined a second group of FU, that came to the ED throughout the first year of the COVID pandemic (from March 1st, 2020, to February 28th, 2021).
For descriptive data analysis we used Pearson’s chi-square for categorical variables and Independent-samples T-Test for continue variables. A confidence level of 0.05 was considered statistically significant. Data was analyzed using SPSS version 23®.
From January 1st to December 31st, 2018, we had 31,078 visits to the Pediatric ED of SSH, corresponding to 14,949 users, with a mean of 2,08 visits per patient. FU was defined as a patient with eleven or more visits to the Pediatric ED, which corresponded to the 99th percentile of visits to the ED that year.
About half of the patients (55.58%) registered only one visit to the ED. The 90th percentile corresponded to 4 visits per year and the 99th percentile corresponded to 10 admissions per year.
The number of visits was relatively constant throughout the year, with a small peak in the winter months (December (n = 2913) and January (n = 3232)) and a slight decline in April (n = 2168), August (n = 2169) and September (n = 2124) (Figure 1).
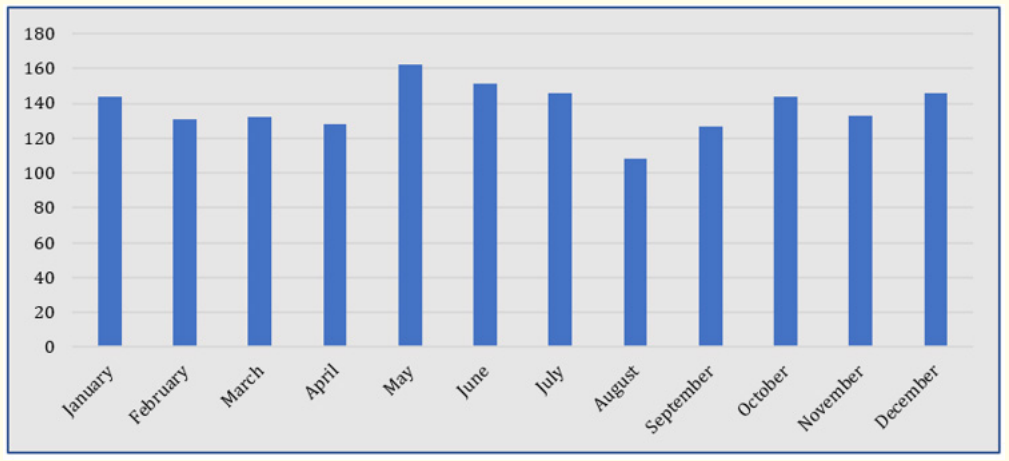
Figure 1: Number of visits to the ED during 2018.
In our study group, FU accounted for 5,3% of total visits (1658 visits during 2018) despite being only 0,82% (123 patients) of those who have used the ED. The minimum number of visits was eleven (n = 44) and the maximum was twenty-three (n = 1). The mean age was 2.4 years (SD ± 2.99); 75,6% of children were 2 years old or less; 3,3% of FU were adolescents (Figure 2). There was no significant difference between gender (50.4% were male and 49,6% female).
The mean maternal age was 31.6 years (minimum 17, maximum 48 years) and the mean paternal age was 34.8 years (minimum 20, maximum 52 years).
As for geographical origins of patients, 39,8% came from the same geographical area as the hospital (Santa Maria da Feira), and 59,5% were from other referral areas: Oliveira de Azeméis (22,0%), Ovar (13,8%), São João da Madeira (9.8%), Arouca (5,7%), Vale de Cambra (4.1%), Estarreja (2.4%), Albergaria (1.6%) and Vila Nova de Gaia (0.8%).
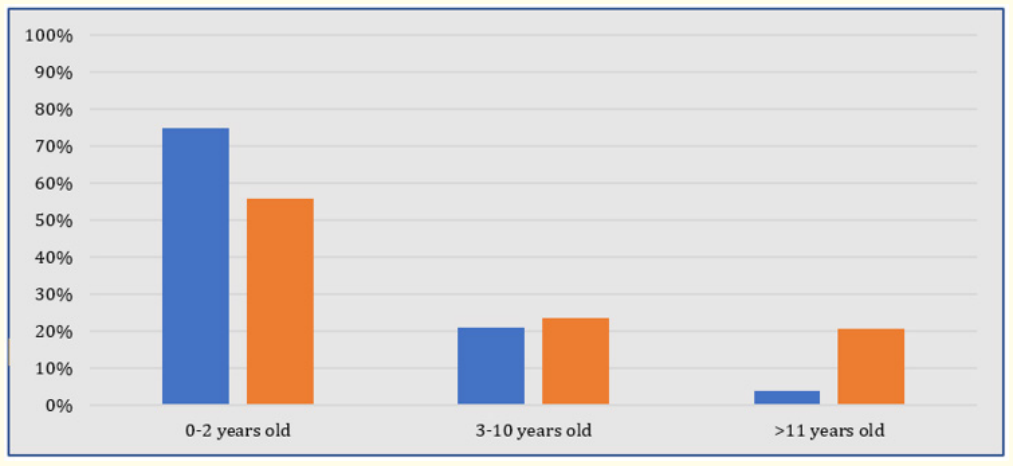
Figure 2: Age group of frequent users, during 2018 and 2020.
As for their previous medical history, 30% of patients had a chronic disease: recurrent wheezing or asthma (n = 17), prematurity (n = 13), primary immunodeficiency (n = 2), juvenile idiopathic arthritis (n = 1), urinary tract congenital malformation (n = 1), epilepsy (n = 1), mitochondrial disease (n = 1), and polymalformative syndrome (n = 1).
More than half (52.8%) had regular hospital follow-up in CHEDV and 46% had a record of at least one previous hospitalization in our department. However, most of the reasons for visiting the ED were unrelated to their previous conditions.
As in the total study population, FU’ visits were relatively constant through the year, ranging from a minimum of 107 visits in August to a maximum of 162 visits in May. There was also no significant discrepancy regarding the day of admission, although a higher frequency was recorded on Sundays (n = 272) and lower frequency on Wednesdays (n = 202) (Figure 3). Analyzing time of admission, 42,8% of FU came to the ED from 6pm to 0am (Figure 4).
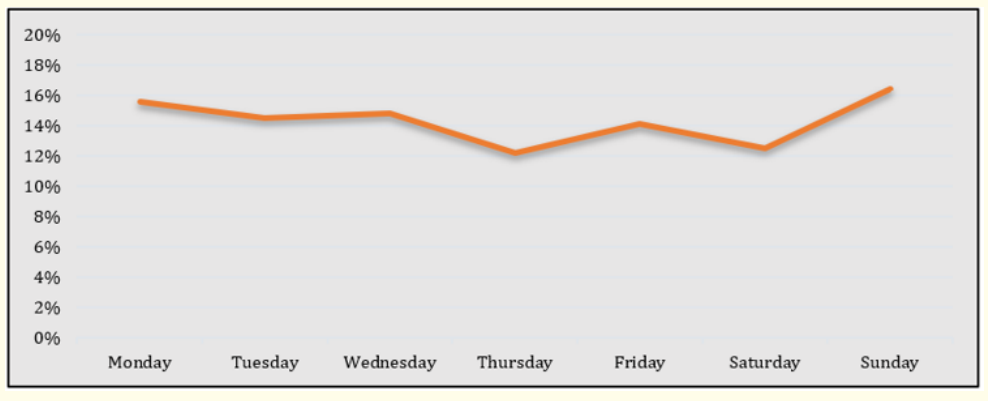
Figure 3: FU’ visits to the ED, in 2018, according to the day of the week.
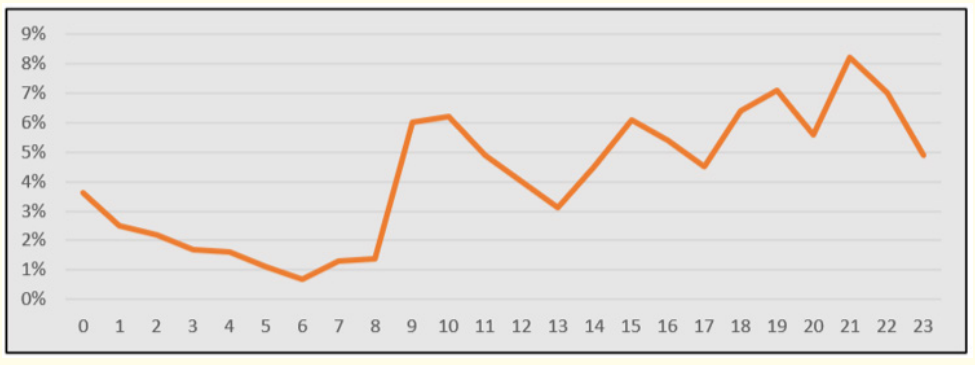
Figure 4: FU’ visits to the ED, in 2018, according to the hour of admission.
Most visits (72%) were classified as first observation; only 2% of the patients had a referral from non-pediatric basic emergency rooms or primary care, and 28% were reassessments or recurrences. Almost all episodes (91%) were triaged as non-urgent. Regarding the reasons for seeking medical care at the ED, respiratory symptoms were the most frequent (53.4%), followed by gastrointestinal symptoms (16.2%) and fever (14.7%). Considering the symptoms’ duration, 78% reported symptoms initiated within 24 hours, 33% within two to five days prior to ED visit and in 17% symptoms had been present for longer than five days.
Most of the FU visits did not require diagnostic tests (66%), or medication (78%) and only 4% needed other specialty consultation at CHEDV. In 93% of the episodes, patients were discharged home; 2,6% of them were referred to outpatient consultation at CHEDV. 2.7% of the patients were admitted to the Pediatrics Department, 3.7% stayed in for observation for 24 hours. 7 patients had to be transferred to another hospital (observation by other specialities or need for intermediate or intensive care).
The most frequent diagnosis (Figure 3) was unspecified viral infection (16.8%), upper airway infection (16.8%), acute otitis media (12%), acute recurrent wheezing (10.1%), gastroenteritis (9%) and pneumonia (6%). Only 35% of the episodes resulted in ambulatory medication.
During 2018, we recorded one death among the FU, a 4-year-old female child with a personal history of prematurity of 35 weeks and a polymalformative syndrome.
From March 1st, 2020, to February 28th, 2021, we had 11016 visits to our pediatric ED, which represented a 65% reduction compared to the year of 2018 (Figure 5). We had 7441 patients visiting the ED, which was a 50% decline in the number of patients (Figure 5) and a reduction to 1,48 visits per patient. Sixty-eight patients with six or more visits were defined as FUs. They represented 0.9% of patients and were responsible for 4.6% of total visits. None of the FU of 2018 met this criterion and 53% of them did not use the ED at all.
The minimum number of visits was 6 (n = 28) and the maximum was no more than fourteen (n = 1). The mean age was 4.7 years (SD ± 5.69). Children less than 2 years old or less were the ones that visited the ED the most in the year of 2020 (55.9%). The next most frequent users were the adolescents (19,1%) (Figure 2.). There was predominance of male patients (54,4% vs 45,6%) but with no statistical significance. As for their medical background, 44% had a previous chronic illness, of which 36.7% had mental health conditions such as anxiety disorders; 60.3% had a regular follow-up in our hospital but only 26,5% had ever been admitted to our Pediatric Department.
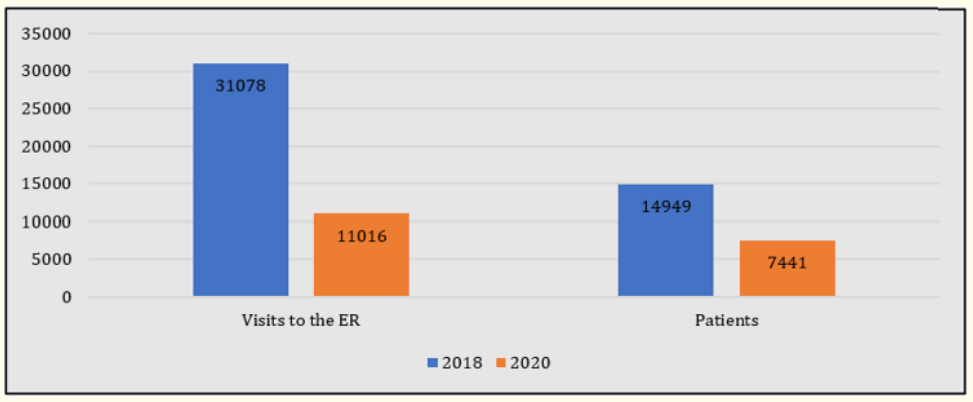
Figure 5: Number of visits to the ER and number of patients in 2018 and the first year of the pandemic.
Comparing both groups, we found that 2020 FU were older (2.44 vs 4.65 p < 0.001), with a significant higher proportion of adolescents (19,1%) compared to 2018 (3,3%). However, children younger than 12 months were the group that used the ED most frequently during the year of the Pandemic (44,6%), which also contrasted to what happened in 2018 (6,5%).
Frequent users from 2020 had less previous admissions to the Pediatric Department (26.5% vs 45.5% p < 0,01), no difference in children with follow-up consultation in our hospital (60.3% vs 50.4% p = 0.221) and more frequently a relevant medical history (44.1% vs 40.7% p < 0.001) mental health conditions being the most frequent (16.2% in 2020 vs 1.6% in 2018 p < 0.001).
This study describes the reality of a Pediatric ED in a level II Hospital within a public health system that is free of cost and universal. Primary health care for children is assure by family doctors, also public, or private pediatricians. So, in terms of accessibility and availability we found higher levels of use (2,08 visits/patient and 0,8% patients responsible for 5,3% visits) even when compared to those who have the same type of organization (1,7 to 1,88 visits/ patient) [10]. This is not only explained by proximity, because most of our patients were not from areas close to the hospital. It is probably due to availability of complementary exams caregivers think may be necessary, assurance that they’ll be seen by a pediatrician, and the 24-hour accessibility.
The fact that 75.6% of FU were children under 3 years old is consistent with what we have encountered in the literature [6,1012]. Younger children go to ED more frequently and that can be explain by parents’ inexperience and common recurrence of upper respiratory tract infections in this age group, specially in a population such as ours, with a high attendance rate of kindergarten under 12 months. That can also be inferred by the hourly distribution of FU. Most visits to the ED occur after working hours, in agreement to the results of another Portuguese Pediatric ED study [12].
The presence of a chronic disease or a relevant health condition has also been described as a risk factor in some studies [1,4] but its influence is variable [5,11] and normally associated with a more adequate use of hospital settings. The characteristics of the episodes that most frequently brought children to the ED were similar to the observations in other studies: symptoms with less than 24 hours of evolution [13], mostly respiratory symptoms [8] and only a minority of visits corresponded to true emergencies [13-15]. This is why more than two-thirds of our patients didn’t need complementary exams or medication while in the ED, and over 90% were discharged home, which was similar to the results published in the literature [1,4,12,15].
The Covid-19 pandemic had and still has a major impact on society and healthcare systems. We have witnessed a pronounced decrease in ED demand during 2020 by all users, but to what extent it also affected FU behavior was to be clarified [9]. Under the circumstances of lockdowns and fear for a new viral threat, who were the patients that continued to come repeatedly to the ED?
During 2020, annual admissions to the ED decreased considerably and the same pattern was observed among FU. There were various reasons listed in the literature to justify the decrease in pediatric admissions to the ED, some being the changing behaviors and concerns of the caregivers during a pandemic period or the decrease in transmissible infections due to social distancing [9,16,17]. However, the published results analyze all patients that visit the Pediatric ED. There are no studies that focus only on FU.
In our study the characteristics of FU compared to what was described in the literature altered significantly. Small children under 12 months were the most representative age group that even in adverse times, continued to use ED for non-urgent observation. This highlights the need for support of inexperienced parents. The development of policies directed to improve health education and promote a more effective access to primary care, are some of the measures that can increase the quality of the care provided, reduces patient’s risk of delayed diagnosis of a serious illness and increases professional´s satisfaction for not working in an overcrowded and under pressure environment. On the other hand, the second age group that we identified as being FU was the adolescents with mental health issues. We recognize that this study’s design does not allow us to make assumptions on the implications of Covid-19 Pandemic for pediatric mental health nor was that our purpose. Our analysis includes only a selected group of children using the pediatric ED. But the 10-fold increase in the number of children and adolescents with mental health issues that are recurrently using the ED may be a reflection of a larger problem that will have to be addressed. There is growing concern that a pediatric ED may not have the best conditions or trained staff to care for this special population of patients. How long the impact of the pandemic on children’s and adolescent’s mental health will last is still unknown but it is urgent to invest in prevention and early detection programs, establishing dedicated open-access centers for mental health care as alternatives to ED, and creating conditions for adequate ambulatory treatment and follow-up after discharged from ED [18,19].
Furthermore, it would be worthy to evaluate if this trend continued through the second year of the pandemic and whether the frequency of ED will resume to pre-pandemic numbers and after all public health measures are lifted.
The Pediatric ED frequent user’s profile at our institution was similar to described in the literature: children under 2 years old, without serious previous health conditions, with a preference for after-work hours, presenting with fever and respiratory symptoms, who do not need for auxiliary exams or urgent treatment and are discharged home unmedicated. During the first year of the Covid-19 Pandemic, the use of pediatric ED was more reasonable, as demonstrated by the smaller number of visits needed for the 99th percentile, but still we had a high percentage of inadequate visits of young children without serious disease. The unique and very worrisome finding in our study was the significant increase in mental health related cases. Overall, this evidence requires further studies to confirm this trend, and needs to be addressed properly in order to develop successful healthcare strategies.
The authors declare no conflict of interests.
Copyright: © 2022 Teresa Pinheiro., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.