Gunjan Baweja* and Dr. Rajdeep Singh
Department of Pediatrics, J. P. Medical Centre, Chandigarh, India
*Corresponding Author: Gunjan Baweja, Department of Pediatrics, J. P. Medical Centre, Chandigarh, India.
Received: October 24, 2022; Published: April 28, 2022
Citation: Gunjan Baweja and Dr. Rajdeep Singh. “Persistent Sinus Tachycardia as an Early Marker in Kawasaki Disease”. Acta Scientific Paediatrics 6.5 (2022): 24-25.
Kawasaki Disease (KD) causes coronary artery lesions which can be prevented if KD is diagnosed and treated early. We present a 6-month-old child with persistent sinus tachycardia who evolved to develop KD. Persistent sinus tachycardia must not be disregarded as can be an early marker of Kawasaki Disease.
Keywords: Kawasaki Disease; Sinus Tachycardia; Coronary Artery Lesions.
Kawasaki Disease is the most common cause of vasculitides in children. Coronary artery involvement (dilation, aneurysm, and stenosis are common complications that can be prevented if diagnosed and treated early [1]. Persistent sinus tachycardia, disproportionate to fever, in a child can be an early marker in Kawasaki disease.
We present a 6-month-old child, known case of small muscular ventricular Septal defect (VSD), presented with a history of cough, cold and fever for a day and at presentation was febrile, Fever (101oF), had tachycardia (HR- 190/min), tachypnoea (RR- 56/min) and hypoxia ((SpO2- 95% in room air). He had bilateral wheeze on chest examination and a harsh pan systolic murmur parasternal. The liver was not enlarged and no evidence of congestive heart failure. He was thus admitted with a provisional diagnosis of bronchiolitis. Investigations done showed Hemoglobin - 8.8gm/L, TLC - 20500/mm3, ANC - 12710/ mm3, Platelet- 380x109/L. Blood cultures were sterile. X-ray chest was normal. initiated on intravenous amoxicillin and clavulanic along with other supportive measures. His tachypnoea settled and wheeze improved on day 2, though fever and tachycardia persisted. Sinus tachycardia with a heart rate between 180-220 beats/min persisted despite being apyrexial. Electrocardiogram as shown in (Figure 1). Echocardiography showed a small VSD (SIZE), with a left to right shunt, normal ejection fractions no vegetations, or no coronary artery dilatation. Serum Calcium was normal. On day 3, the child was noted to have red eyes. Tachycardia persisted. On day 4, the child developed a truncal rash and, thus with a possibility of Kawasaki Disease, inflammatory parameters were assessed. CRP, ESR were 45mg/L and 115mm/in the first hour respectively. The urine routine showed 10 - 15 pus cells with sterile culture. The child received intravenous immunoglobin (2g/Kg) the same day. Tachycardia subsided and he became well. On follow-up, echocardiography done showed no coronary artery involvement.
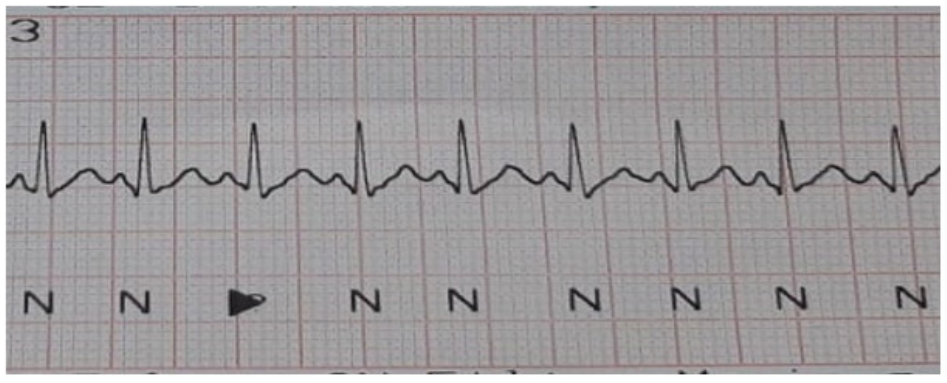
Figure 1: ECG of the Child in the early phase.
Sinus Tachycardia.
Suzuki., et al. [2] in 1999 reported tachycardia as a potential risk indicator for coronary artery disease. They studied 26 patients with Kawasaki Disease and recorded their mean 24-hour heart rate and its correlation with the coronary artery involvement and concluded that the mean heart in the group with coronary artery involvement was higher than in the group with no coronary artery involvement. Another case report by Sheybani., et al. [3] in 2015, presented a patient with persistent tachycardia in the acute phase who did not meet the other criteria of Kawasaki Disease and was clinically stable and was discharged from the hospital. He later developed coronary artery lesions and presented with shock. They emphasized recognition of this subtle clinical feature, which can appear early in the course of KD. Our child developed features of KD like rash and red eyes during hospitalization, but persistent tachycardia was recognized from the first day of presentation.
The index child had many other risk factors for coronary artery involvement like age less than 1 year, male sex, high WBC count but due to early recognition, diagnosis, and prompt treatment, no complications were noted.
To conclude persistent sinus tachycardia can be the early marker for Kawasaki disease and clinicians must be aware of this so that early diagnosis can be established and coronary artery involvement can be prevented.
No conflict of interest.
Copyright: © 2022 Gunjan Baweja and Dr. Rajdeep Singh. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.