Victoire Kouakou*
C.O.P Cabinet d’Odontologie Pédiatrique, France
*Corresponding Author: Victoire Kouakou, C.O.P Cabinet d’Odontologie Pédiatrique, France.
Received: November 24, 2021; Published: December 31, 2021
Citation: Victoire Kouakou. “Screening for Children's Obstructive Sleep Apnea Syndrome as Part of the French Dental Prevention Program M’T Dents "LuvUrtheeth"”. Acta Scientific Paediatrics 5.1 (2022): 25-30.
To screen Obstructive Sleep Apnea Syndrome in a population of preventive-conscious children in a private paediatric dentistry practice, within the French dental health prevention program called “M’T dents” LuvUrtheeth.
Parents of children aged 3-6 years answered a 20-item questionnaire collecting symptoms of OSAS, from January 2015 to July 2019 for a prospective, mono-centric, observational study. A questionnaire, developed and made available to parents during the dental prevention visit, collected self-reported information on the identification of at least three symptoms of OSAS. This approach made the screening legal. The polysomnography, allowed to confirm the diagnosis and to indicate the severity of OSAS.
103 children were screened with a mean of the Obstructive Apnea Hypopnea Index (O-AHI) of 5.6 for various symptoms: snoring, mouth breathing, nocturnal hypersudation, bruxism, morning fatigue, attention and concentration disorders, enuresis, eating difficulties, obesity, somniloquy, sleep-walking. To promote and improve an early detection of OSAS, the French dental preventive device “M’T dents” which is now aimed at children from 3 years old, implemented since April 2019 constitutes an interesting way to investigate paediatric population.
Keywords: OSAS; Paediatric; Early Screening; French Dental Preventive; “M’T Dents” Program.
OSAS: Obstructive Sleep Apnea Syndrome; O-AHI: Obstructive Apnea Hypopnea Index; M’T Dents: Aime Tes Dents “LUVurtheeth”.
Within the “M’T dents” program, the French National Health Insurance allows all children and adolescents aged 3, 6, 9, 12, 15, 18, 21 and 24 years to benefit from a free screening appointment with the dental surgeon and from care, if necessary [1,2]. During this oral screening visit, a relative questionnaire is associated to identify and screen children likely to have OSAS [3]. Indeed, the diagnosis of OSAS is based upon day and night clinical signs [4]. All children are invited, from the age of 3 years, since April 19, 2019 to visit their dental surgeon for a preventive appointment. This examination as well as the resulting dental care is covered by health insurance. Children with OSAS with or without maxillofacial abnormalities rarely go to the sleep specialist right away. A simplified multi-criteria screening questionnaire is proposed to parents during the M’T dents visit to look for daytime and nightime clinical signs of OSAS [5-7]. The screening of OSAS is based upon clinical elements of orientation deepened if necessary by the interrogation (parents, children, siblings).
The prevalence of OSAS is 1 to 4% more frequent between 3 and 6 years of age [8,9]. Hence the need to understand this target population in early childhood when we know the consequences of OSAS on growth, cognition, behavior, mood, cardiovascular system... etc.
The Haute Autorité de santé (HAS) has listed the clinical criteria for OSAS in children (Table 1) [3].The symptoms and clinical signs are nocturnal and diurnal, directly related to the obstruction of the upper airways with disturbances in nasal respiration as well as tonsillar hypertrophy and adenoid were found to be a risk factor of OSAS in primary school children associated with poor quality of sleep [13]. The clinical examination is an essential first step to suspect a diagnosis based on the signs, assess the severity [14] and judge the need for a polysomnography to decide on the treatment and the therapeutic follow-up [10].

Table 1: Diurnal and nocturnal signs of OSAS for screening of the M’T Dents program.
The easily identifiable nocturnal and daytime clinical signs described by parents for OSAS screening are underlying dental malocclusions which are in fact only the consequences and not the cause of dental malocclusions [11,12].
The incidence of OSAS causes functional problems with oral ventilation, swallowing, phonation, chewing and aesthetics. The maxillary hypodevelopment is accompanied by a narrow nasal cavity, an ogival palate and a low position of the tongue. Retrusion, hyperdivergence and/or insufficient mandibular development. These abnormalities are accompanied by cranio-facial signs (elongated face, recessed chin) and usually dental malocclusions coexist with well known child profiles [13-17].
Three profiles of OSA can be found [12,13]:
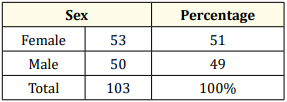
Table 2: Sex ratio.
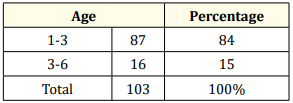
Table 3: Age of children.
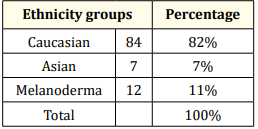
Table 4: Children’s ethnicity.
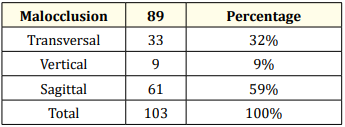
Table 5: Distribution of oro-facial growth direction.
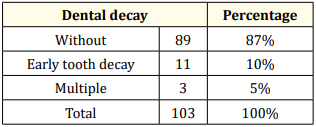
Table 6: Distribution of dental decay.
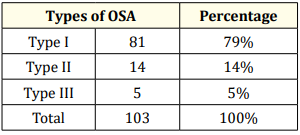
Table 7: Distribution of types of OSA.
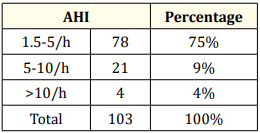
Table 8: Distribution of AHI.
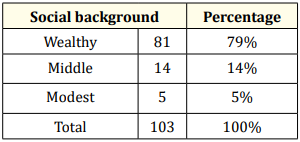
Table 9: Distribution of social environment.
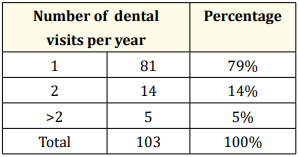
Table 10: Distribution of number dental visit.
The sex ratio is 49% for young boys against 51% for young girls (Table 2). More caucasian children have been found with OSAS type I [9] Table (4-7). Screened children have been seen earlier because more than 80% were 2 years and 6 months old, e.g. before their 3rd birthday. By lowering the age of the first visit to the dentist at the end of complete lacteal dentition and before the eruption of the 6-year-old teeth, this approach constitutes a major step in the establishment of the concept of overall health of the young children (Table 5). Indeed, it is no longer just a question of establishing a patchwork health screening for caries and oro-myo-facial malocclusions but also effectively coordinating the harmonious growth of the child through a multidisciplinary approach [15].
The treatment of OSAS being multidisciplinary, the pediatric dentist is one of the actors in this early detection because not only dental problems have been taken account [8,19,20].
Paradoxically, children whose parents consult were hardly affected by caries lesions. 87% of children are free from cavities and 3% of children have cavities affecting baby teeth (Table 6). Indeed, no permanent tooth, especially the 6-year-old tooth, has yet been affected at this stage (Table 6). This situation, although it augurs a positive development in behavior, is unfortunately biased because it is based upon a preventive conscious population who would no doubt have consulted with or without the invitation of M’T Dents from French preventive program (Table 9,10).
This is the reason why it probably does not reflect the reality of the French situation in the prevention of dental caries in view of the national figure. The benefit of the M’T Dents approach is to use this system to alert parents and offer screening to make the preventive device effective.
In children, the benefit of early detection induces coordinated multidisciplinary management [9] to avoid neurocognitive, behavioral, cardiovascular and metabolic complications [24]. The advantage of the early detection allows early treatment before the establishment of basic reading and arithmetic learning [25,26]. It avoids loss of luck and removes medically wandering children to make a positive diagnosis.
We found that the value of AHI does not always correlate with the severity of OSA. In fact, children with discreet signs could present high AHI values and vice versa. Hence the need for a screening approach based essentially on the clinic. The mean AHI of 5.6 reflects the need to take into account the clinical signs because 79% of the children screened had moderate OSA with AHI 1.5-5/h and 5% a severe OSA with AHI > 10/h within the framework genetic pathology (Table 7,8).
This examination, undertaken by a trained professional, makes it possible to prevent the installation of the deleterious effects of OSA as quickly as possible [23].
Early detection prevents children from the deleterious social and economic effects of OSA. The medical consequences in adults not detected during childhood and consequently not treated lead to heavy medical care with the social and economic repercussions of OSAS [27].
In addition to caries lesions, the majority of Angle’s malocclusions [24] as well as Dento Maxillary Disharmony (MDD) [16,17,22] are generally the first call-in situations that direct parents to the dental surgeon and not the oral ventilation situation of young children (Table 6). Any dysmorphosis of the jawbones is not always related to OSAS. Likewise, not all Angle Cl II by retromandibulia are necessarily synonymous with OSAS. On the other hand, a common notion remains by the deficit of height-weight growth induced at this age with an incidence on orofacial growth. Clinical sense, additional examinations and polysomnography values make it possible to objectify OSAS [27,28].
The diversity and multiplicity of OSAS warning signs explain the need for a multidisciplinary approach. This makes it possible to set up a therapeutic strategy aimed at increasing the volume of the upper airways by hygieno-dietetic measures, pharmacological, surgical, orthodontic and/or functional treatments coupled with oro-myo-functional re-education by speech therapists, osteopaths and physiotherapists, faced with the maintenance and stability of the resolution of functional problems [29,30].
Early detection removes children from the harmful social and economic effects of OSAS. The medical consequences in adults not screened during childhood and therefore untreated resulted in heavy medical care [28].
This early screening is all the more interesting given that parents who are aware of the problem also have siblings or even beyond children screened by involving certain parents who were unaware of the possibility of presenting an OSAS, despite the presence of obvious signs of calling, in particular of daily snoring associated with overweight [18,20,21,24].
So unexpectedly, once the child is screened, the entire extended family circle, from grandparents to parents, offers and submits to OSAS screening.
Inviting M’T DENTS health insurance program is certainly an effective public health weapon, because in the absence of this program some children aged 3 to 6 would not benefit from any followup. While the invitation sequence every 3 years seems reasonable for preventive-conscious populations. This situation loses all the advantage of preventive public health action for poor populations at risk (Table 9,10).
The advantage of using the M’T Dents program is a preventive public health approach in terms of screening and cohort. This action is based on proven targeting of the school population for which parents are invited to undertake care and if necessary to contact parents within an institutional and legal framework to strongly encourage or even force them to undertake care. Since school is compulsory until the age of 16 for each child, it is possible to monitor the children even when a parental move occurs. The results of this study were aimed at performing OSA screening in Brittany schools.
Childhood OSAS has its own characteristics. You have to know how to look for it because a child never complains about his sleep. Respiratory manifestations begin in the second part of the night. It is necessary to think about it in front of a staturo-weight delay, in front of an excessive daytime hyperactivity.
Mechanical and functional orthopedic therapies have shown their effectiveness on pediatric OSAS, in addition to adenoidectomy-tonsillectomy follow by orthodontics if it is necessary. The screening can be performed by paediatric odontologists.
The author declare no conflict of interest.
Copyright: © 2022 Victoire Kouakou. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.