Surender S Kajla and BS Karnawat*
Department of Pediatrics, JLN Medical College, Ajmer, Rajasthan, India
*Corresponding Author: BS Karnawat, Department of Pediatrics, JLN Medical College, Ajmer, Rajasthan, India.
Received: October 20, 2021; Published: November 30, 2021
Citation: Surender S Kajla and BS Karnawat. “Follow Up of High Risk Neonates Discharged from SNCU Up to 1 Year Period”. Acta Scientific Paediatrics 4.12 (2021): 62-68.
Objective: This study was undertaken to follow and assess growth, neurodevelopment, immunization status, dietary pattern, morbidity and mortality in high risk newborns successfully discharged from Special/Sick Newborn Care Unit (SNCU) till one year period.
Method: This prospective study was conducted in SNCU of department of pediatrics, JLN medical college and hospital Ajmer. All neonates admitted and successfully discharged from SNCU during the period April 2018 to September 2018 were enrolled for the study and prospectively followed up to one year period.
Results: Out of total 1011 neonates successfully discharged, 618(61.1%) infants were followed up to 1 year. Out of 618 infants, 18% infants had weight <3rd percentile, 8.2% infants had length <3rd percentile, 9.7% infants had head circumference <3rd percentile. Developmental delay and increased muscle tone was found in 13.1% and 10.2% infants respectively. Most (72.2%) infants were on exclusively breast feeding up to 6 months while complimentary feeding was started in 98.5% infants by age of 1 year. Majority (93.4%) of infants were immunized. Abnormal BERA was found in 18 (2.9%) infants while retinopathy of prematurity was found in 6 (0.9%) infants. Diarrhea, respiratory infections, seizure disorder and Congenital Heart Disease (CHD) were major causes of morbidity while 45 (4.4%) infants expired before attaining 1 year age, mostly due to sepsis, respiratory infections and CHD.
Conclusion: High occurrence of growth failure and faulty feeding practices were documented. Most common morbidities were found to be diarrhea, respiratory infections, and seizure disorders. Other co morbidities observed were developmental delay, hearing difficulties, retinopathy of prematurity, cerebral palsy etc. Major causes of mortality were found to be sepsis, respiratory infections and congenital heart disease.
All high risk neonates should be followed up and assessed periodically to identify growth failure and neurodisabilities so that early intervention can be done.
Keywords: High Risk Infants; Follow Up; Growth Failure; Neurodevelopment; SNCU
Close obstetric-neonatal collaboration, better management of neonatal problems and technological advances in neonatal care all have contributed to increased survival of high risk newborns. These improvements have been most dramatic in infants born with extreme low birth weight (ELBW) (<1000 gm) and at extremes of viability (22-25 weeks) [1-4].
Numerous studies have shown that despite substantial improvements in the neonatal mortality, the incidence of chronic morbidities like cerebral palsy and adverse outcomes among survivors has not declined much [5,6]. This is also associated with reports of increasingly high incidence of neuro-sensory impairment (blindness and deafness), cognitive, learning disabilities and behavioral problems. This highlights the need for a follow up care service that would ensure systemic monitoring of practically all sick newborns after discharge from hospital, specially following infants are at moderate to high risk to develop neuromotor disability and must be followed in accordance with set protocol [7].
At follow-up infant should be specially assessed and monitored for - Feeding and dietary adequacy, Growth, Development, Immunization, Ongoing problem, Neurological, Eye and Hearing evaluation [8].
Since the launch of Janani Shishu Suraksha Karyakram (JSSK) in 2011, follow up of newborns successfully discharged from SNCU has been integral and important component of this programme, but so far only a few studies on follow up of sick newborns are available in literature, and none from this part of country, hence present study was planned.
This prospective study was conducted in sick newborn care unit (SNCU) of department of pediatrics, JLN medical college and hospital, Ajmer from April 2018 to September 2019 (i.e. 18 months).
All neonates admitted and successfully discharged from SNCU during period of April 2018 to September 2018 were enrolled for the study and prospectively followed up till one year in well baby clinic and details were recorded on institutional follow up performa as developed by UNICEF for National Health Mission (NHM). It includes five visits in follow up schedule i.e. 8 days, 1 month, 3 months, 6 months, and 1 year from time of discharge.
Physical growth assessment was done by measuring weight by electronic weighing machine with ±5 gm accuracy, length by using infantometer and head circumference by non stretchable measuring tape. WHO growth charts were used to assess growth by plotting changes in weight, length and head circumference at 1 month, 3 months, 6 months and 1 year from discharge [9]. For preterm infants data were recorded on WHO growth charts after 40 weeks of gestational age.
Neurodevelopment assessment was done by using revised
Trivandrum Development Screening Chart (2013) at 6 months and 1 year [10].
To assess neurologic deficit, tone assessment was done by using Amiel Tison method [11] and accordingly classified as normal or increased tone.
Hearing assessment was done with help of audiologist by Brainstem Evoked Response Audiometry (BERA) screening for all infants within 3 months post- natal age and was repeated at 6 months, if initially abnormal.
Retinopathy Of Prematurity (ROP) screening was done by ophthalmologist for premature infants, following the standard timing schedule based on postnatal age.
Data were recorded in pre-structured proforma and compiled in master chart. Data entry and statistical analysis was performed with the help of Microsoft Excel and SPSS version 25 (IBM SPSS Statistics inc. Chicago, Illinois, USA). Categorical variables were presented as number and percentage. Chi-square test was used to compare differences in categorical variables and independent ttest, p value < 0.05 (at 95% confidence interval) was considered to indicate statistical significance.
Prior approval for the study was taken from institutional ethical committee of JLN medical college Ajmer. Informed consent was taken from mothers.
A total of 1011 neonates discharged from SNCU were included in this study, 618(61.1%) infants were followed up to 1 year, 348(34.4%) infants were lost to follow up and 45(4.4%) infants died during follow up. Most of deaths occurred within 1 month period (Table 1 and Figure 1).

Table 1: Follow up pattern.

Figure 1: Follow up pattern.
Growth of 618 infants followed up to 1 year. 82% infants had normal weight while 18% infants had weight <3rd percentile, 91.8% infants had normal length while 8.2% infants had length<3rd percentile, 90.3% infants had normal head circumference while 9.7% infants had head circumference <3rd percentile at age of 1 year (Table 2).
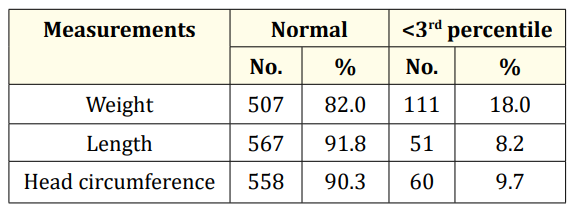
Table 2: Growth of infants during follow up at 1 year (n = 618).
13.1% infants had developmental delay while 86.9% infants had normal development at 1 year of age. 10.2% infants had increased muscle tone while 89.8% infants had normal muscle tone at 1 year of age (Table 3).

Table 3: Neurodevelopment of infants during follow up at 1 year (n = 618).
At 6 months follow up 72.2% infants were given exclusive breast feed while 16.7%, 9.7% and 1.4% infants were on mixed feed, animal milk and formula feed respectively (Table 4).
Complementary feeding was given in majority of infants (98.5%) while in 1.5% infants, no complementary feeding was started up to age of 1 year (Figure 2).
Majority of infants (93.4%) were completely immunized up to age while 6.6% infants were found to be partially immunized (Table 5).
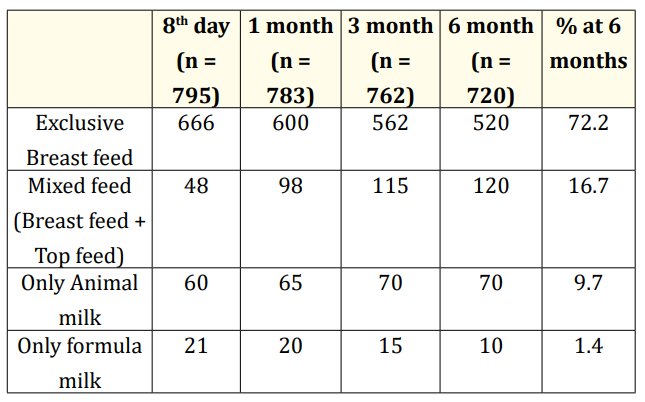
Table 4: Feeding status of infants after discharge from SNCU till 6 months.

Figure 2: Feeding status of neonates after discharge from SNCU at 1 year.

Table 5: Immunization status of neonates after discharge from SNCU at 1 year.
Initial Brainstem Evoked Response Audiometery (BERA) test was abnormal in 39(6.3%) infants while persistent BERA abnormality was found in 18(2.9%) infants in repeat examination (Table 6).
Retinopathy Of Prematurity (ROP) was found in 6(0.9%) infants (Table 7).

Table 6: Hearing assessment of neonates after discharge from SNCU till 1 year.

Table 7: Ophthalmic assessment of neonates admitted in NICU.
Most common morbidities after discharge from SNCU were found to be Diarrhea (38.0%), Respiratory infections (30.1%) and Seizure disorders (14.3%) while Congestive heart failure (6.4%), Sepsis (4.8%), Convulsion and cerebral palsy (4.8%) were other causes of readmission.

Table 8: Morbidity during first year of life after discharge from SNCU (n = 189).
Out of 1011 neonates after discharge from SNCU, 45(4.4%) infants died within 1st year. Majority of infants (73.3%) died within 1 month after discharge (Table 9).
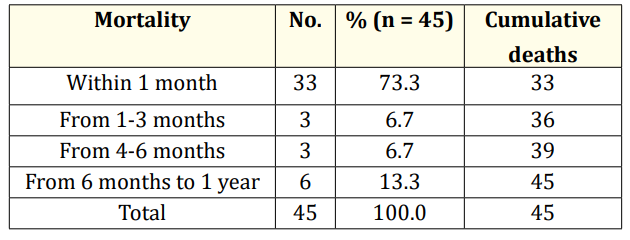
Table 9: Mortality distribution after discharge from SNCU (n = 45).
Major causes of mortality within 1st year of discharge from SNCU were found to be Sepsis (40%), Respiratory infections (33.3%) and Congestive heart failure (13.3%) (Table 10).
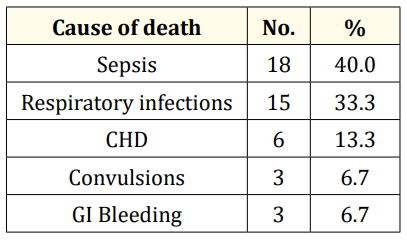
Table 10: Cause of death of infants after discharge from SNCU (n = 45).
A total of 1386 neonates were admitted in NICU during 6 month of period. Of whom 846 neonates were successfully discharged, 336 neonates expired during treatment, 39 neonates were referred, mostly for surgical interventions, and 165 neonates left against medical advice LAMA). Thus a total of 1011 infants were followed up. Out of these 618 infants (61.2%) were followed up to 1 year, 348 infants (34.4%) were lost to follow up and 45 infants (4.4%) died during follow up.
The drop-out rate was 34.4% in our study whereas it was 35.2% in the study by Padmaja D., et al. [12], 9.6% in study by Das S., et al. [13]. Budden S., et al. [14] described that infants with normal weight and normal development often have high attrition rate from follow up programmes. Other causes for drop out may be attributed to residence in far-off rural areas, lower parental education and lower socioeconomic status.
In the growth assessment of infants during follow up at the age of 1 year, out of 618 infants 111 infants (18%) had weight < 3rd percentile, 51 infants (8.2%) had length <3rd percentile and 60 infants (9.7%) had head circumference <3rd percentile. Studies by Modi M., et al. [15], Westerberg A C., et al. [16] and Boo NY., et al. [17] showed that chances of postnatal growth failure were more in preterm infants. Other factors associated with growth failure in infants were faulty feeding, developmental delay, comorbidities like recurrent diarrhea, recurrent respiratory illness, cerebral palsy, seizure disorder, congenital heart disease etc.
This study revealed that at the age of 1 year 63(10.2%) infants had increased muscle tone (hypertonia) and 555(89.8%) infants had normal muscle tone. Study by Baburaj., et al. [18] found tone abnormalities in 8.5% infants while higher prevalence of tone abnormalities were found in study by Das S., et al. [13] 37.4% and Choudhari S., et al. [19] 35.2%.
Developmental delay was present in 81(13.1%) infants at 1 year of age. The incidence of developmental disability in NICU survivor was described to be 10-20% by Budden., et al. [14], 15% by Paul., et al. [20], 15.6% by Sukumaran., et al. [21], and 22% by Das S., et al. [13].
Our study has shown that neonatal hypoglycemia, meningitis and birth asphyxia are most decisive factors of adverse neurodevelopmental outcome later on in life. Similar results have been found in studies by Das., et al. [13], Luo YF., et al. [22], and Kumar M., et al. [23].
Feeding assessment in this study revealed that 72.2% infants were on exclusive breast feed, 16.7% infants were on mixed feed (breast feed and top feed), 9.7% infants were on exclusive animal milk and 1.4% infants were on formula milk at the age of 6 months. At age of 1 year, 98.5% infants were given complementary feeding while in 1.5% infants complementary feeding was not started. Study by Gaur A., et al. [24] revealed that 69.3% infants were on exclusive breast feed, 19.3% infants were on mixed feed.
As far as immunization status is concerned, 93.4% infants were fully immunized and 6.6% infants were partially immunized up to age of 1 year. According to NFHS-4 [25], 54.8% children were fully immunized in Rajasthan. Higher immunization rate in our study indicates importance of continuous follow up, proper counseling and awareness about vaccination in parents.
Initial Brainstem Evoked Response Audiometry (BERA) was abnormal in 39(6.3%) infants while in repeat examination 18(2.9%) infants have persistent BERA abnormality. Study by Choudhari S., et al. [19] and Gaur A., et al. [24] revealed sensorineural hearing loss in 1.5% and 1% infants respectively.
Retinopathy of prematurity (ROP) was observed in 6(0.9%) infants. Incidence of ROP was 1.1% and 0.3% in study by Sukumaran., et al. [21] and Choudhari S., et al. [19] respectively.
After discharge from SNCU, 189(17.2%) infants were rehospitalized in first year of life. Common causes of admission were – diarrhea (38.0%), respiratory infections (30.1%), seizure disorder (14.3%) congestive heart failure (6.4%), sepsis (4.8%), cerebral palsy (4.8%), anaemia (1.6%). Rehospitalization rate in study by Choudhari S., et al. [19] and Harding JE., et al. [26] were 23.5% and 30% respectively. Common causes of readmission in study by Gaur A., et al. [24] were respiratory infections (23%), diarrhea (19%), growth failure (12.2%).
Mortality rate was 4.4% (45 infants) in first year of life after discharge from SNCU. 73.3% of deaths occurred during first month, 13.4% of deaths were from 1 month to 6 months of life while 13.3% of deaths occurred from 6 month to 1 year of life. Major causes of deaths were sepsis (40%), respiratory infections (33.3%) and congestive heart failure (13.3%). In Study by Padmaja D., et al. [12], 1st year mortality rate was 12.04% while 80% deaths occurred in first month of life. Study by Choudhari S., et al. [19] revealed that 1st year mortality rate was 9.4% and 72.7% deaths were due to infections (gastroenteritis, septicemia, pneumonia etc).
During follow up high occurrence of growth failure and faulty feeding practices were documented among the infants discharged from SNCU. Most common morbidities were found to be diarrhea, respiratory infections, and seizure disorders. Other co morbidities observed were developmental delay, hearing difficulties, retinopathy of prematurity, cerebral palsy etc. Major causes of mortality were found to be sepsis, respiratory infections and congenital heart disease. Majority of post discharge death occurred during 1 month period.
This study reemphasizes the need for regular follow up and assessment to identify growth failure and neurodisabilities for early interventions, thereby ensuring that high risk children maximize their potential and become productive and valued members of society. At the same time mothers should be sensitized to seek early medical attention if baby develops any danger signs so that infant mortality can be reduced specially during post-discharge one month period.
Nil.
Copyright: © 2021 Surender S Kajla and BS Karnawat. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.