Jumbi T* and Lessan J
Paediatric Surgery Unit, Department of Specialized Surgery, Kenyatta National Hospital, Nairobi, Kenya
*Corresponding Author: Jumbi T, Paediatric Surgery Unit, Department of Specialized Surgery, Kenyatta National Hospital, Nairobi, Kenya.
Received: September 13, 2021; Published: October 18, 2021
Citation: Jumbi T and Lessan J. “Paediatric Bladder Stones in Kenya. A Single Institution Study". Acta Scientific Paediatrics 4.11 (2021): 33-37.
Objective: This study describes the patterns of etiology and presentation of bladder stones in children managed at tertiary facility in Kenya with an aim of highlighting the magnitude of disease.
Materials and Methods: A retrospective review of 20 patients with bladder calculi was done between 2013 and 2020. Data that was collected from the patients’ medical records included age and sex distribution; seasonal and geographical distribution; patterns of presentation and etiology.
Results: All patients recruited were male with a mean age of 4.85 years. There was no significant trend in the seasonal and geographical distribution of bladder calculi. Patients with acute urinary retention presented the earliest. Notably, the patients with hematuria in the background of lower urinary tract symptoms presented earlier than those without hematuria. The majority of bladder stones were primary in etiology (n = 12), However 7 patients had secondary bladder stones, resulting from Vesico-ureteric reflux (n = 4), posterior urethral valves (n = 1) and anorectal malformations with recto-urethral fistulas (n = 2).
Conclusion: This study reveals a general inclination towards delayed diagnosis in children presenting with bladder stones especially in the absence of acute urinary retention and hematuria. Additionally, congenital anomalies of the urinary tract should be suspected in patients with bladder stones particularly in presence of urinary tract dilatation.
Keywords: Etiology; Presentation; Bladder Stones; Paediatric; Urolithiasis; Kenya
LUTS: Lower Urinary Tract Symptoms; KUB: Kidney Ureter Bladder; VCUG: Voiding Cysto-urethrogram; KNH: Kenyatta National Hospital; PUV: Posterior Urethral Valves; ARM: Anorectal Malformation; UTI: Urinary Tract Infection; VUR: Vesico-Ureteral Reflux
In developed countries, the prevalence of stone disease is 10 - 15% and bladder calculi account for 5% of the stone burden which is reported to be higher in developing countries [1]. Bladder stones are more prevalent in males with a reported ratio of 10:1 and peaks at about three years of age [2]. Bladder calculi can be classified as primary, secondary, or migratory [3].
Primary or endemic bladder calculi are defined as those which occur in the absence of other urinary tract pathologies. The determinants for primary bladder stones are nutritional deficiencies especially that of animal protein, poor hydration mainly due to inadequate intake and recurrent diarrhea. Secondary bladder stones are defined as those which occur in the presence of other urinary tract abnormalities. The determinant for secondary bladder stones include conditions causing functional and mechanical bladder outlet obstruction and conditions causing recurrent urinary tract infections. Migratory bladder stones are defined as those originating from the upper urinary tract [4].
In children bladder stones may cause lower urinary tract symptoms, recurrent infections, pain and hematuria. In the long term, bladder calculi are associated with a risk of damage to the upper tracts and risk of bladder cancer [4]. This study describes the patterns of etiology and presentation of bladder stones in children managed at tertiary facility in Kenya with an aim of highlighting the magnitude of disease.
This is a retrospective review of 20 patients managed with bladder calculi between 2013 and 2020 at Kenyatta National Hospital which is the largest teaching and referral hospital in Kenya with a well-established Paediatric surgical unit. Data was collected from the patients’ medical records included age and sex distribution; seasonal and geographical distribution; patterns of presentation and etiology.
All patients were managed according to the hospitals management protocol on bladder calculi which includes clinical assessment; laboratory panel including serum electrolyte measurements and urine analysis; imaging including KUB ultrasound and VCUG; cystoscopy and open cystolithotomy.
Continuous data was analyzed and summarized as mean, median and standard deviations while categorical data was analyzed and displayed in charts by use of frequencies and proportions. Institutional approval to conduct the study was sought and granted.
All the patients recruited were male. The mean age in years was 4.85 while the median age was 5. The youngest patient was 1 year while the oldest patient was 11 years.
The distribution according to month of presentation is shown in figure 1. The dry seasons in the country are marked in red while the rainy seasons are marked in blue, there was no seasonal trend noted in this distribution. The highest recorded occurrence was in the month of march with 4 patients.
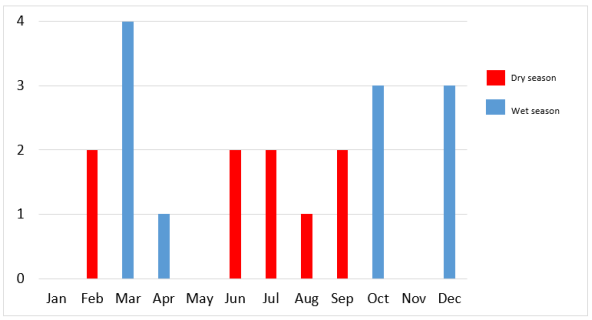
Figure 1: Seasonal distribution of bladder stone occurrence.
The geographical distribution is shown in figure 2. Most patients reside in central and rift valley of Kenya n = 13 with a few patients distributed in the arid and semi-arid lands n = 7.
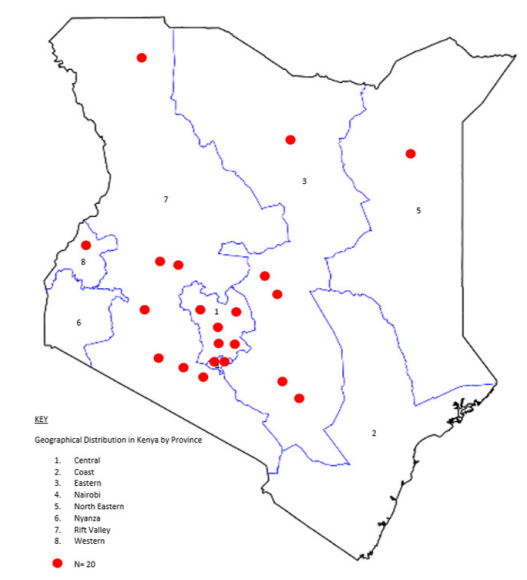
Figure 2: Geographical distribution of bladder stone occurrence.
The average duration of symptoms was 1 year. The main presenting complaints included acute urinary retention, hematuria and LUTS such as frequency, urgency, dribbling, strangury and dysuria. Patients with acute urinary retention presented earlier (less than 5 days). Notably, the patients with hematuria in the background of LUTS presented earlier than those without hematuria. This distribution is seen in table 1.
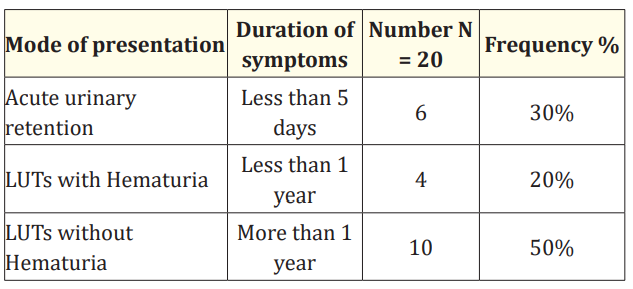
Table 1: Patterns of presentation.
The majority of bladder stones were primary in etiology (n = 12), However 7 patients had secondary bladder stones, the underlying urinary tract pathology in these patients included with Vesicoureteral reflux (n = 4), posterior urethral valves (n = 1) and Anorectal Malformations (ARM) with recto-urethral fistulas (n = 2). This distribution is shown in figure 3.
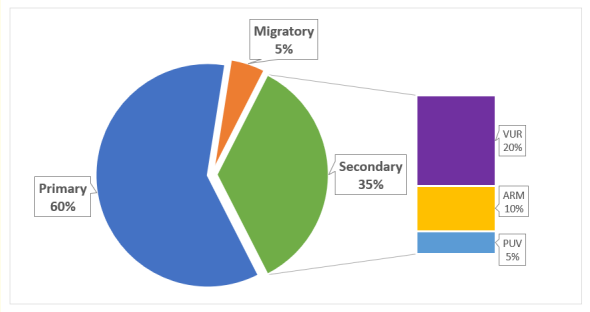
Figure 3: Patterns of etiology.
VUR- Vesico-Ureteric Reflux.
ARM- Anorectal Malformations.
PUV- Posterior Urethral Valves.
Epidemiologic studies have shown an increase in the prevalence pediatric bladder calculi. The true nature of epidemiologic trends may be difficult to study due to under diagnosis and under reporting. Additionally, the detection of risk factors for formation of bladder calculi requires additional investigation to establish the precipitation events in either primary, secondary or migratory stones [1,2]. In this study we highlight the various trends including a propensity of late diagnosis for patients with vague urinary symptomatology and the association of bladder calculi with congenital disorders such as Anorectal malformations, posterior urethral valves and Vesicoureteral Reflux.
In this study all patients presenting with bladder calculi were male. The male to female ratio of bladder calculi is 10:1. The main risk factor for this distribution is the urethral anatomy with girls having short, non-tortuous urethras which allow passage of calculi debri without retaining nuclei which is otherwise retained in the male bladders [2]. The peak age of bladder calculi occurrence is 3 years in children, in this study the average age was 4.85 years however the average duration of symptoms was 1 year making it difficult to conclude on the accurate age of presentation.
Endemicity of bladder stones in Africa has been described previously in relation to the famous afro-asianic stone-belt. This belt stretches from Morocco, Mauritania, Algeria, Tunisia, Libya, subSaharan Africa (Mali, Chad, Rwanda, Ethiopia, Cameroon, Niger), Sudan, Egypt, Turkey, Saudi Arabia, the United Arab Emirates, Iraq,
Iran, Afghanistan, Pakistan, India, Nepal, Myanmar, Thailand, and Indonesia to the Philippines [1,5]. Kenya in particular is not included in this belt, however local published literature have noted stone disease in arid and semi-arid lands in Kenya associated with scarcity of drinking water and hot climate with a predisposition to dehydration [6,7]. In this study, a geographical distribution is seen around the central part of Kenya with a few patients scattered in the arid and semi-arid areas. The main catchment for the study setting is central Kenya and may explain the observed distribution. Similarly, the seasonal distribution did not conform to any predisposition of occurrence as there is no much difference in frequency between the wet and dry seasons of the year. This has been documented in previous local literature where the distribution of urolithiasis was evenly distributed throughout the seasons in a six-year period [7].
The presentation of bladder calculi includes presence of Lower Urinary tract symptoms such as frequency, urgency, dribbling, strangury and dysuria. In addition, there may be reports of hematuria, turbid sandy urine or passing of actual stones per urethra. If complete obstruction ensues the presentation will be that of acute urinary retention, this may be accompanied by other symptomatology of straining including rectal prolapse and conjunctival hemorrhages. Finally, bladder calculi may only present with recurrent UTI and may be an incidental finding in upto 10% of patients [1,5,8]. This study revealed an interesting pattern of presentation with an average duration of symptoms of upto 1 year. This delay in presentation was more in patients without hematuria and without complete urine retention. On the other hand, patients with LUTs and hematuria presented much earlier. Logically, the patients with acute urinary retention presented the earliest. This pattern conforms to the poor health seeking behavior seen in developing countries, in particular a local study carried out in Kenya shows that caregivers who delay in taking their children to the hospital immediately after symptomology usually perceive the illness as mild and self-limiting [9].
The majority of primary/endemic stones notwithstanding, the occurrence of secondary bladder stones and their pattern of distribution in this study is worth discussing. Secondary bladder stones contributed to almost one third of calculi. Majority of these had Vesico-ureteric reflux (VUR), a condition which is documented to predispose to stone formation through several mechanisms. VUR is linked to urinary stasis, bacteuria and recurrent urinary tract infections which are known to predispose to stone formation [10]. Secondly, studies confirm that there is an association between hypercalciuria and hyperuricosuria with VUR which leads to urinary stone formation [10,11].
The association of Posterior Urethral Valves and vesical calculi has been reported in various published case reports. The highlighted objective in these reports is to have clinical awareness of the existence of such an association which may otherwise lead to delayed diagnosis of posterior urethral valves [12,13]. In one of our patients, this association was detected and the patient was treated by both valve ablation and open cystolithotomy.
A rare but possible association is the presence of bladder calculi in patients with anorectal malformations [14]. ARM is a common pediatric surgical condition that presents with recto-urinary fistulas such as recto-bulbar, recto-prostatic and recto-vesical fistulas [15]. One factor that predisposes occurrence of urinary calculi in patients with ARM is incomplete fistula resection with posterior diverticulum lithiasis [15] Additionally, the communication of the urinary tract to the rectum in patients with such fistulae predisposes the urinary tract to infections which may form a nidus to bladder stone formation [16].
We acknowledge that data was collected from patient records, consequently any errors of documentation during initial recording of these details contribute to our study limitations. Additionally, the study population is small and therefore not representative of a true epidemiological study. To this effect the study herein may not make conclusive statements on epidemiological statistics rather the study has made inferences that can be tested in larger study populations.
This study reveals a general inclination towards delayed diagnosis in children presenting with bladder stones especially in the absence of acute urinary retention and hematuria. Additionally, congenital anomalies of the urinary tract should be suspected in patients with bladder stones particularly in presence of urinary tract dilatation. Finally, ARM presents a unique and rare association with bladder calculi in children.
Kenyatta National Hospital, Department of Specialized surgery, Paediatric Surgery Unit.
University of Nairobi, School of Medicine, Thematic Unit of Paediatric Surgery.
No funding or grant support.
The following authors have no financial disclosures: T.J, J.L.
Copyright: © 2021 Jumbi T and Lessan J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.