Effectiveness of Matrix Rhythm Therapy with Traditional Physiotherapy for Child
with Spastic Diplegic Cerebral Palsy from 13 Months to 7 Years Age: A Case Report
Sonali S1 and Edwin Dias2*
1Senior Research Scholar, Srinivas University, India
2Head of Pediatric Department, SIMS, Mangalore, India
*Corresponding Author: Edwin Dias, Head of Pediatric Department, SIMS,
Mangalore, India.
Received: July 22, 2021; Published: September 24, 2021
Abstract
This case study shows the effectiveness of matrix Rhythm therapy for 13 month old girl with Cerebral palsy. The aim was to find
out the effectiveness of matrix rhythm Therapy when combined with traditional physiotherapy to improve gross motor function..
Before starting physiotherapy treatment the girl had lots of impairments on gross motor function and GMFCS level was 3. On Denver
developmental scale evaluation she was 8 month behind in two subgroups of gross motor and fine motor. MACS level was 3. CFCS
level 1. The child still continues Physiotherapy session at the age of 7 years once a month. After receiving intensive Physiotherapy
she improved in gross motor function specially sitting standing walking stair climbing and jumping. As well improvement was seen
in balance and posture. The modified Ashworth scale, goniometry evaluation, GMFM-88, MACS, CFCS, Pediatric Berg balance scale
were used as outcome measure. There was drastic improvement seen in GMFM SCORE after Matrix Rhythm therapy combined with
traditional physiotherapy for this type of cerebral palsy.
Keywords: Matrix Rhythm Therapy; Cerebral Palsy; Gross Motor; Fine Motor
Introduction
Cerebral palsy is one of the most challenging motor orders in children. Cerebral palsy describes a group of permanent disorders of development, of movement and posture causing activity limitation that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The motor disorders of cerebral palsy are often accompanied by disturbances of sensation, perception, cognition, communication and behaviour, by epilepsy and by secondary musculoskeletal problems. Spastic diplegia Cerebral palsy is amongst the most common types.
Matrix rhythm therapy
It is developed by DR. U.G. Randoll in Earlangen’s university Germany. This therapy is based on the research in cell biology. Our cells are pulsating in frequencies of 8-12 hertz in normal healthy condition. During unhealthy situation these movements are slowed down. Marhythe The provides populations in same frequency to synchronize and reset the disturbed cell rhythm that helps to reestablish extra cellular logistics that is removal of waste products and improve microcirculation of with oxygenated blood. It relaxes soft tissues.
Outcome measures
- GMFCS -ER (Gross Motor Functional Classification System The functional classification system is used to classify cerebral palsy child. GMFCS classifies the gross motor function according to age group. This system has five age bands comprising of 0 to 2 years, 2 to 4 years, 4 to 6 years, 6 to 12 years, 12 to 18 years. Each group has 5 level. Level 1 is the least problem where as level 5 has the most problems.
- MACS (Manual ability Classification System) It assess the child's ability to handle object in important daily activities, exercise, play, leisure, eating, dressing. It describes how children handles the object in school and community. The classification is designed to reflect the child's typical manual performance, not the child's maximal capacity. It classifies the collaborative use of both hands together.
- CFCS (Communication function classification system) Methods of communication used are speech, gesture, behaviour, facial expression, eye gaze, augmentative and alternative communication. Level 1 describes effective sender and receiver with unfamiliar and familiar partner communication occurs easily and at a comfortable pace with both familiar and unfamiliar place. Communication misunderstandings are quickly repaired and do not interfere with the overall effectiveness of persons communication.
- Pediatric balance scale - The Pediatric Balance Scale (PBS), a modification of Berg’s Balance Scale, was developed as a balance measure for school-age children with mild to moderate motor impairments. Examination of balance is an important element of a physical therapy evaluation for a school-age child. The clinician must predict the ability of the child to safely and independently function in a variety of environments (i.e., home, school, and community)
- Gross Motor Function Measures: The Gross Motor Function Measure (GMFM) is the instrument most commonly used to measure gross motor function in children with cerebral palsy.
Case details
Child was born on 7 August 2014. First Physiotherapy evaluation was done on 5th September 2015. History revealed that child was born full term through LSCS as healthy child. Child had cried loudly and was not admitted to NICU. She didn’t had any respiratory distress or any other high risk factors. Mother was considered at risk of developing hypertension. MRI revealed changes in bilateral cerebral hemisphere with volume loss and mild ex-vacuo prominence of bilateral cerebral white matter. There is prominence of bilateral cerebral sulcus space. Thinning of Corpus callosum was seen. Small focus of gliosis was found in left cerebellar white matter. The evidence revealed history of hypoxic ischemic encephalopathy.
Child was assessed thoroughly. Assessment was done at consecutive ages still 7 years. Treatment was given one hour daily 5 days a week from 13 months to 2 years. Bi weekly sessions were given from 2 years age still 3 years. Follow up was done every month from three years to seven years of age.
Goals of treatment
Functional goals- Independent dressing, eating, bathing, grooming transfers.
Treatment strategies
- Matrix Rhythm Therapy (Every session Matrix Rhythm Therapy was given for minimum half hour to maximum 1 hour, each site was repeated after 48 hours, all muscles were treated)
- Hot water fomentation
- Vestibular training - Daily
- Balance training - Daily
- Proprioceptive neuromuscular facilitation- 4 times Daily 30 repetition each side
- Weight bearing activities- daily
- Coordination training. Thrice a week
- Gait training (With variety of tracks) thrice a day after 2 years
- Posture training with Visual cues, mirror and oral commands. Daily
- Weight cuff training (For Strengthening of Lower limb and upper limb muscles) daily 10 reps thrice two times a day… initially assisted then gradually active movements were trained.
- Hand function training with activities like Painting with broad brushes, Beads, marbles, tying knot, buttoning, writing.
- Aquatic therapy was given twice a month.
Observations
- Child can do reach out activities more efficiently when goal of reaching is placed displaying the output (example touch and play drum, hit me toy)
- Helping the child in repetition of activity helps self organisation and also creates more permanent motor patterns out of the continual activity
- Transition training is the phase which takes maximum time to achieve accomplishment example crawling to standing, kneeling to standing, standing to jumping. These are the phase where new patterns, new forms of movements more likely occur
- Effective control of musculoskeletal system results from decrease in degrees of freedom which are assembled into functional patterns and not by the direction given by the nervous system by organisation of body system motor behaviour is the end product of self organisation among the many element comprising a system including but not only limited to CNS.
Findings
- Matrix Rhythm therapy decreased the co-contraction of muscles which assisted in easy movements.
- Matrix Rhythm therapy decreased hypertonicity instantaneously. The time taken to optimise the muscle tone was minimal relative to traditional approaches.
- Matrix Rhythm therapy never tired the child during activities rather child was more encouraged to perform activities happily.
- Matrix Rhythm therapy in combination with other traditional therapeutic strategies developed the child globally from the beginning of Physiotherapy session.
- Self involvement of child encouraged the family members and therapist to give more priority to advanced movement skill, finer movement.
- At school based setting learning was at high performance as well as leisure activities.
- With the assistance of Matrix Rhythm therapy the higher mental function development was excellent at the age of 3 years when child started going school.
- Follow up sessions of matrix Rhythm therapy keep the residual fluctuating tone at optimal level, thus further increasing balance and kept... decreased trick movement pattern.
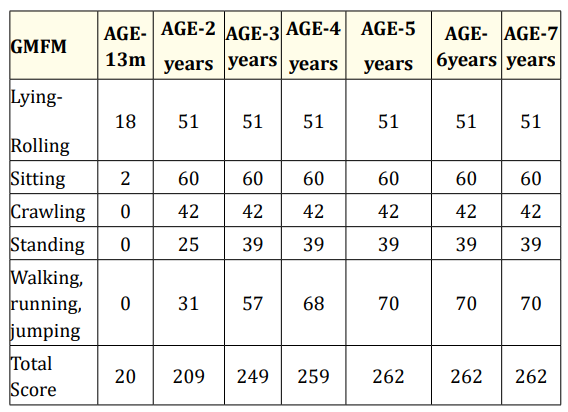
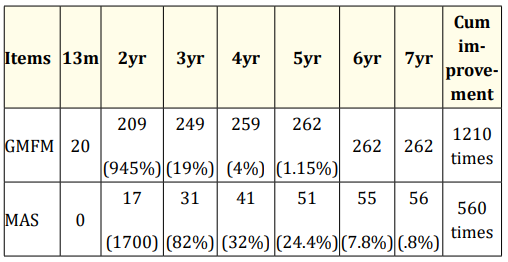
- GMFM 88 score showed improvement.
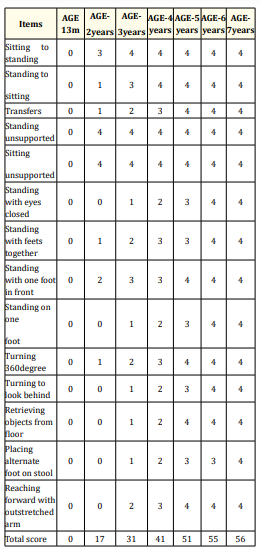
- Balance was improved drastically from 13months to 2 years.
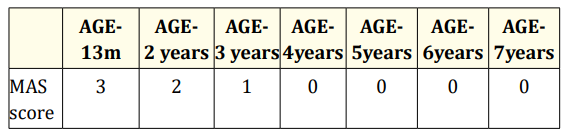
- Modified Ashworth scale showed decline in hypertonicity.
- Learniability and higher mental function was excellent after therapeutic intervention with familial support.
Discussion
Multisystem is affected which includes tone, alignment, posture, balance, coordination. In child with cerebral palsy independence in functional skills depends upon some or all developmental areas as motor, sensory, cognitive, communication behaviour. The child also needs to recognise the social needs. GMFCS level was achieved to Level 1 at the age of two and half years. It was level 5 at the age of 13 months. GMFM score improved from 0 to 209 (2 years) and was maximum after 5years. Pediatric Balance score improved from 0 at the age of 13month to 17 at the age of 2 years. The maximum score was achieved after 6 years. Table 4 clearly depicts changes in GMFM and MAS score proving maximum improvement was seen between 13months and 2 years. The overall effect was 1210 times at the age of 7 years in GMFM score. The MAS score showed improvement by 560 times at the age of 7 years [1-7].
Table 1: Gross motor function measure scores at various age of
child.
X
![]()
Table 2: Modified ash worth scale at various ages of child.
X
![]()
Table 3: Pediatric berg balance score at various ages of child.
X
![]()
Table 4: Improvement analysis in Gmfm and mas score across the
age till 7 years.
X
![]()
Conclusion
Matrix rhythm therapy effectively optimised the muscle tone of cerebral palsed child in less than expected time duration. The combined therapeutic approach kept child and family motivated to continue efforts till goals were achieved completely. The child’s overall performance is appreciated as above average in school, home and community settings.
Financial Support and Sponsorship
Nil.
Conflict of Interest
No conflict of interest.
Bibliography
- Peter Rosenbaum., et al. “The definition and classification of cerebral palsy”. Developmental Medicine and Child Neurology s109 (2007): 1-44.
- Eliasson AC., et al. “The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability”. Developmental Medicine and Child Neurology7 (2006): 549-554.
- Compagnone E., et al. “Functional classifications for cerebral palsy: Correlations between the gross motor function classification system (GMFCS), the manual ability classification system (MACS) and the communication function classification system (CFCS)”. Research In Developmental Disabilities 35.11 (2014): 2651-2657.
- “Matrix Rhythmus Therapie” (2010).
- Sonali Shrivastava. “Matrix rhythm therapy: a new dimension in pain management and restricted mobility- “birth injuries”. International Journal of Advance Research in Science and Engineering1 (2015).
- Sonali Shrivastava and Arif K S. “An Overview of Matrix Rhythm Concept and Efficacy of Matrix Rhythm Therapy in Pathological Conditions”. International Journal of Health Sciences and Pharmacy (IJHSP)1 (2019): 25-30.
- Annika Lundkvist Josenby., et al. “Longitudinal Construct Validity of the GMFM-88 Total Score and Goal Total Score and the GMFM-66 Score in a 5-Year Follow-up Study”. Physical Therapy 89.4 (2009): 342-350.