Assumpta Udechi Chapp-Jumbo1, Nneka Chioma Okoronkwo2* and Stella Nnenne Ijeoma3
1Consultant Paediatrician, Professor of Paediatrics, Department of Paediatrics, Abia State University Teaching Hospital, Aba, Abia State, Nigeria
2Consultant Paediatrician, Associate Professor of Paediatrics. Department of Paediatrics, Abia State University Teaching Hospital, Aba, Abia State, Nigeria
3Senior Registrar, Department of Paediatrics, Abia State University Teaching Hospital, Aba, Abia State, Nigeria
*Corresponding Author: Nneka Chioma Okoronkwo, Consultant Paediatrician, Associate Professor of Paediatrics. Department of Paediatrics, Abia State University Teaching Hospital, Aba, Abia State, Nigeria.
Received: August 24, 2021; Published: September 09, 2021
Citation: Assumpta Udechi Chapp-Jumbo., et al. ““Tongue Tie” in South East Nigeria- The Practice, The Myths, The Rip Offs”. Acta Scientific Paediatrics 4.10 (2021): 13-18.
This cross sectional study sets out to elucidate the myths and practices surrounding ankyloglossia also known as ‘Tongue tie’ among mothers in an immunization clinic in south East Nigeria.
The prevalence of frenotomy was 27.3% and the reasons for the procedure were mainly concerns about delay in speech, problems with quality of speech or coercion by health workers who put fear of possible speech problems in the mothers.
The level of education or the place of delivery did not affect the prevalence of the practice. Complications of frenotomy like bleeding was found in 13.3% of those that had the procedure.
A call is made for health education of mothers, health workers and those caring for newborns to prevent the unnecessary use of this procedure so as to avoid serious complication. It will also help mothers to seek attention for suspected ankyloglossia from those who have the skills to make proper diagnosis and intervention.
Keywords: Ankyloglossia; Tongue Tie; Myths; Practice; Rip-Off; Frenotomy
The tongue is involved in speech, feeding, and taste. It also plays a role in the way a person is perceived especially with respect to articulation of speech.
The normal tongue is freely mobile within the mouth and can also be protruded outside the mouth at will, especially during processes like cleaning the lips, kissing and licking (e.g. ice cream).
The normal tongue has a frenulum which attaches its underside to the floor of the mouth [1]. The attachment of the frenulum to the tongue should normally be approximately 1 cm posterior to the tip of the tongue [2]. The frenulum’s attachment to the inferior alveolar ridge should be proximal to, or into the genioglossus muscle on the floor of the mouth.
Developmentally, this frenulum may be too short and therefore restrict the movement and mechanical activities of the tongue [3]. The presence of such short frenulum leads to ankyloglossia (Tongue tie).
Evaluation for the diagnosis of ankyloglossia (AG) may be difficult. It is not always apparent by looking at the underside of the tongue, but is often dependent on the range of movement permitted by the genioglossus muscles [1]. For infants, passively elevating the tongue tip with a tongue depressor may reveal the problem. For older children, making the tongue move to its maximum range will demonstrate the restriction of the tip of the tongue. In addition, palpation of genioglossus on the underside of the tongue will aid in confirming the diagnosis [1,5,6].
Ankyloglossia has many proven complications and in the newborn the major effect is with the interference with proper latching on and suckling and this can have negative effects on exclusive breastfeeding [4].
Treatment options such as observation (wait and watch), speech therapy, frenotomy without anesthesia, and frenectomy under general anesthesia have all been suggested in the literature [7,8]. In the 19th century, midwives were ardent at clipping the lingual frenulum as a routine and even had to reserve a sharp fingernail for the procedure [1].
The frenotomy procedure is defined as the cutting or division of the frenum when a child is less than 4 months old and this procedure when indicated, can be done in the outpatients’ clinic without anaesthesia [2]. The discomfort associated with the release of thin and membranous frena is brief and quite minor, although some schools of thought recommend anaesthesia no matter the age. This may be by use of conscious sedation or at least some anaesthetic gel applied topically.
The tongue is lifted gently with sterile gauze and stabilized, exposing the frenum. This may be achieved by the placement of 2 gloved fingers of the clinician’s left hand below the tongue on either side of the midline, retracting the tongue upwards towards the palate and exposing the frenum [2].
The frenum is then divided with small sterile scissors by approximately 2 to 3 mm at its thinnest portion between the tongue and the alveolar ridge, into the sulcus just proximal to the genioglossus muscle. The incision begins at the frenum’s free border and proceeds posteriorly, adjacent to the tongue. This is necessary to avoid injury to the more inferiorly placed submandibular ducts in the floor of the mouth [5].
The frenum is poorly vascularized and is poorly innervated, allowing the clinician to accomplish the procedure without complications. Usually, there is minimal blood loss (i.e. no more than a drop or two, collected on sterile gauze). If need be, bleeding can be controlled easily with a brief period of pressure applied with gauze. The incision is not sutured. In the hands of the untrained with minimal or no knowledge of anatomy, this procedure can be hazardous.
Complications of frenotomy include infection, excessive bleeding, excessive scarring which may lead to a recurrence or worsening of the ankyloglossia, new speech disorders developing postoperatively, and glossoptosis (tongue “swallowing”) due to excessive tongue mobility [2].
Frenectomy is the preferred procedure for patients with a thick and vascular frenum and involves excision or removal of the frenum and severe bleeding may be expected. In young children it is performed under general anaesthesia. Older children or adults, however, may tolerate the procedure with the use of local anesthesia alone [5].
A viable alternative to surgery for children with ankyloglossia is to take a ‘wait-and-see’ approach [3]. Ruffoli., et al. report that the frenulum naturally recedes during the process of a child’s growth between six months and six years of age [7].
Literature from Nigeria suggests that the reasons for requesting for ligation of the frenulum is based on myths about its effect on speech delay [9-11]. Also, that most of those who coerce mothers into having it done on their babies do not even know how to make a diagnosis of ankyloglossia and are not trained to perform the procedure. This inability to perform the procedure leads to high occurrence of severe complications [9-11].
Requests and suggestions for evaluation of the tongue and subsequent interventions in our environment are borne more out of fear of future problems with speech than any relevance to feeding problems.
Mothers attending the Immunization clinic of the Abia State University Teaching Hospital (ABSUTH), Aba, Nigeria, were interviewed. This Teaching Hospital is one of the tertiary health institutions located in the metropolis of Aba. ABSUTH serves as a general/ referral centre for patients resident in Aba metropolis, and adjoining cities and communities in Abia state, including some parts of Akwa Ibom, Rivers and Imo states respectively.
The immunization clinic is part of the under-5 Well Child Clinic of ABSUTH. It is used by mothers in Aba irrespective of their place of delivery.
Aba metropolis is made up of five Local Government Areas (Aba North, Aba South, Osisioma, Ugwunagbo, and Obingwa). It also houses about 4 tertiary institutions. The population though of mixed ethnicity, is made up mostly of those of Igbo extraction of the South South, and South East Geopolitical zones. Mothers in Aba patronize all levels of government owned health institutions as well as private, orthodox, traditional birth places and even churches for delivery and care of their newborns.
Mothers who brought their babies for immunization within a one month period (November 2019) had the questionnaires administered to them by an interviewer. The decision to conduct the interviews within a one month period was to reduce the chances of interviewing a mother more than once since most immunizations are done every 4 weeks starting from the 6th week of life. Questionnaires were answered in the presence of any of the investigators who also assisted those that could not read and write. For this group, the questionnaire was interpreted into their most familiar language. The raw data was analyzed using simple statistical methods.
Ethical clearance was obtained from the Ethical Committee of the Abia State University Teaching Hospital, Aba, Nigeria.
Inclusion criteria: All babies presenting at the immunization clinic within the stated period of one month.
Exclusion criteria: Mothers who declined from being interviewed.
159 respondents aged between 20 and 48 years who came with their babies (165 in number because of 6 sets of twins) to the immunization clinic were interviewed using questionnaires. The babies were 81 males and 84 females.
45 (27.3%) babies had frenotomy procedure done giving a prevalence rate of 27.3%. Thirty-three (20.0%) had the frenotomy before their mothers were discharged from the hospital postpartum, while 12 (7.3%) were discharged but told to come back after a few days to check for tongue tie and eventually had it cut.
Thirty two (20.1%) mothers believed that tongue tie was related to speech delay and should be treated immediately while 13 (8.2%) of them think that treatment for tongue tie is part of routine childcare practice for newborn babies.
Whereas 36 (22.6%) had the frenotomy procedure suggested to them by health workers, family pressure to check for tongue tie was the reason given by 9 (5.7%) of the mothers.
Those who had frenotomy had the procedure done by a nurse as a private arrangement whether in the hospital, health centre or at home, with a fee charged.
Six (13.3%) of the babies who had frenectomy had severe enough bleeding that warranted hospital admission and transfusion as complications. Feeding difficulties was not found to be a reason for frenotomy in any baby.
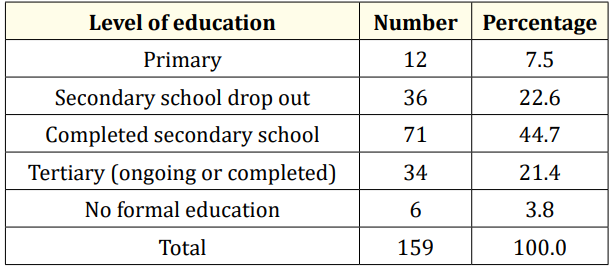
Table 1: Level of education of respondents.
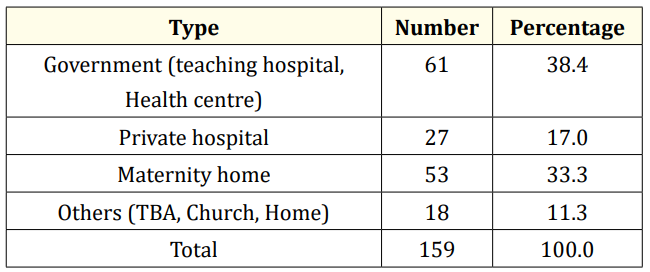
Table 2: Place of delivery.
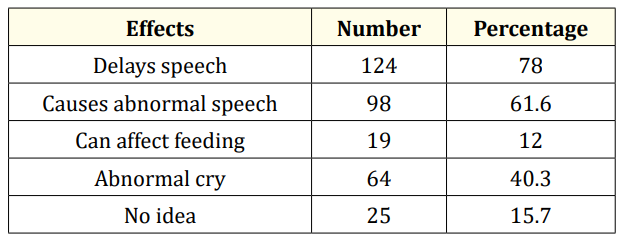
Table 3: Care givers knowledge of effect of tongue tie*.
*: Some care givers gave more than one response on the possible
effect of tongue tie.
![Table 4: Factors influencing institution of frenotomy among those
who had the procedure [i.e. the 45 women whose children had
frenotomy*]. <br>
*: Some mothers gave more than one reason for allowing frenectomy on their baby.](https://actascientific.com/ASPE/images/IJMCR/ASPE-04-0449-table4.PNG)
Table 4: Factors influencing institution of frenotomy among those
who had the procedure [i.e. the 45 women whose children had
frenotomy*].
*: Some mothers gave more than one reason for allowing frenectomy on their baby.
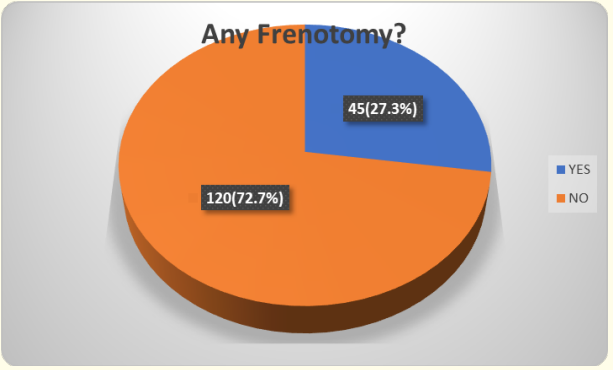
Figure 1: Pie chart showing the number of patients that had frenotomy.
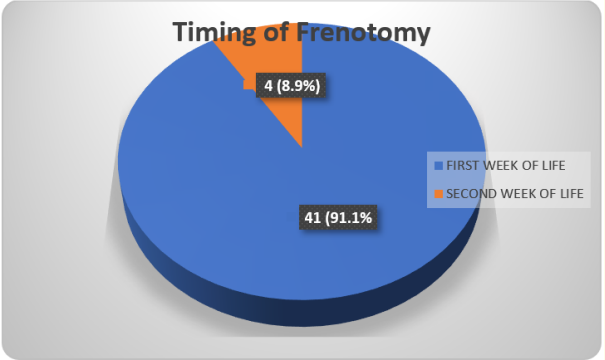
Figure 2: Pie chart showing the timing of frenotomy.
![Figure 3: Source of information about frenotomy. <br>
*[Some respondents had more than one source of information].](https://actascientific.com/ASPE/images/IJMCR/ASPE-04-0449-fig3.PNG)
Figure 3: Source of information about frenotomy.
*[Some respondents had more than one source of information].
The documented prevalence of ankyloglossia (Tongue tie) in literature ranges from 0.3% to 10% [2,12]. It is however higher (20%) in clinics being run for children with feeding difficulties [2].
The prevalence of the practice of frenotomy in this study was 27.3%. Most research article did not document the prevalence of frenotomy in neonates. However, a study from East England reviewed 41 patients (aged 3 - 48 years) that had frenotomy at a dental clinic [13]. In that study, 93% of the patients were children aged 16 years and below [13].
Again, 30 (51.7%) out of 58 babies with ankyloglossia received frenotomy in a study from Portsmouth Virginia [14].
The above studies show that the prevalence of frenotomy among children is very high. This is far higher than the actual prevalence of ankyloglossia among children. This, therefore, highlights the overuse of this procedure. To buttress the fact of overuse of frenotomy, there is no observed difference in the sex of the patients offered the procedure in contrast to studies that found higher incidence of ankyloglossia in males [3,8,15,16].
The number of mothers that had the procedure introduced to them by health care workers in orthodox health facilities is alarming and the reasons also put forward are worrisome. For instance, telling mothers that frenotomy was a routine procedure in the newborn and casting the fear of delayed baby’s speech in them should they reject frenotomy.
Few mothers in this study were worried about the possible effect of ankyloglossia on speech later in life and would rather be proactive towards intervention. This is not unfounded as ankyloglossia is known to cause articulation difficulties in later life and possibly cause embarrassment to the affected [2]. The crux of the matter here is that there was no protocol followed to make a diagnosis of ankyloglossia.
The implication of this high rate in the belief that tongue tie delays speech is that this might leads to rip offs by health care personnel. The later exploit the fear of speech delay to coerce mothers into carrying out the procedure for personal gratification not related to hospital fees.
This attitude may also delay institution of proper intervention in children who have speech delay as caregivers tend to be seen requesting specifically for tongue to be checked or out rightly requesting for frenotomy, when there are other reasons for speech delay. Occurrence of severe life-threatening complications like haemorrhage treated by admission and transfusion as found in this study is also widely documented in literature [1,3,10].
Mothers should be given regular health education on care of their newborn. They should also be granted access to health workers knowledgeable in assessment of Tongue tie and effective intervention if present. This will prevent complications like haemorrhage, haematoma formation, infection and actual abnormal tongue movement that can arise from such procedures in untrained hands.
There is also the need to educate health personnel who come in contact with mothers and their newborns, on diagnosis of AG, the right technique for frenotomy, as well as counseling of anxious mothers.
Medical doctors who own maternity facilities should educate their health staff on the issue of ‘tongue tie’ and ensure that frenotomies are not a routine procedure for newborns, rather a medical intervention for a confirmed diagnosis.
Use of electronic media and education of women groups will go a long way towards stemming the tide of ripping patients off (because of ‘tongue tie’) or even putting the lives of newborns in harm’s way.
The authors have nothing to declare.
None.
Copyright: © 2021 Assumpta Udechi Chapp-Jumbo., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.