Edwin Dias1, Deepak K2* and Sandeep Gada3
1Professor and HOD, Department of Paediatrics, Srinivas Institute of Medical Science and Research Centre, Mangalore, India
2Junior Resident, Department of Paediatrics, Srinivas Institute of Medical Science and Research Centre, Mangalore, India
3Assistant Professor, Department of Paediatrics, Mahaveer Institute of Medical Science, India
*Corresponding Author: Deepak K, Junior Resident, Department of Paediatrics, Srinivas Institute of Medical Science and Research Centre, Mangalore, India.
Received: June 03, 2021; Published: August 27, 2021
Citation: Deepak K., et al. “Bacterial Profile in Children Admitted with Septicaemia in a Semi Urban Hospital in South India”. Acta Scientific Paediatrics 4.9 (2021): 06-09.
Background: Antibiotics resistance is an important reason why the bacterial profile of PICU is mandatory. Here we are studying the bacterial profile of PICU in a semi urban hospital in South India.
Objective: Is to study the bacteria and the culture and sensitivity reports in PICU.
Conclusion: The commonest organism causing sepsis in PICU is Coagulase negative Staphylococcus and this organisms have shown sensitivity to Amikacin.
The pathogenic bacterial aetiology of septicaemia is vast, thus every PICU should emphasize on the importance of a routine periodic testing of microbial bacterial spectrum and their sensitivity to drugs in order to formulate a selective antibiotic regimen for PICU.
Keywords: PICU; Coagulase Negative Staphylococcus; Septicaemia; Amikacin
Fever is the most common symptom in a healthy young child to be brought to a paediatric emergency department [1,2]. The evaluation and management of a young child with fever is a common problem. It has been estimated that nearly 35% of unscheduled ambulatory visits are for fever in children [2]. Bloodstream infection has been a primary concern of physicians for over 80 years. Blood cultures are usually done for the evaluation of sick children with or without evidence of a focus of infection [3]. Many serious infections are associated with bacteraemia and the blood culture may be positive even when cultures of the specimens taken from the local area of infection (cerebrospinal fluid, tissue aspirate, synovial fluid) are negative. A report of a positive blood culture without apparent site of infection usually prompts a clinical re-evaluation and search for a primary focus.
Septicaemia is a condition with a high mortality rate varying from 30-70% depending on virulence and pathogenicity of the organism and its host factors [4,5]. Blood infection is an important cause of death, giving a rate of 25 - 50% [6]. More recently Bloomberg., et al. (2007) [7] reported a mortality of 40% in paediatric patients with laboratory confirmed bacteraemia. Bacterial pathogen isolation in blood culture is often associated with high morbidity and mortality among children [8]. In recent years, septicaemic infections due to Gram-positive cocci have increased antimicrobial resistance and frequency of cases seen [9]. Since the progressive increase in health care problems are related to bacteraemia in children, we attempted to investigate the incidence and pattern of bacteraemia and to determine the bacteriological profile and antibiotic sensitivity pattern in children aged weeks to years admitted to the PICU.
This study was conducted by analysing the blood culture and their sensitivity to antimicrobials, reports obtained during October 2017 to October 2020 from 100 children admitted to the PICU with suspected septicaemia. The patients were divided into two age groups 1month to 6 years and 6 years to 12 years. A second sample was collected on the same day to rule out contamination with the skin flora. Approximately 2cc of blood was drawn under aseptic precautions and inoculated into Brain Heart infusion broth, incubated at 370C for 24 hrs. Subcultures were made on blood agar and MacConkeys agar after 24hrs and 48hrs.Negative cultures were followed up by examining the broth daily for 10 consecutive days. Growth if any was identified by standard bacteriological techniques including gram staining, colony characteristics and biochemical reactions. Antibiotic sensitivity was tested as per recommended guidelines.
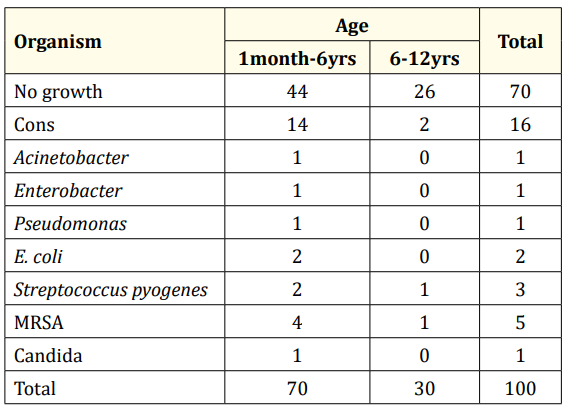
Table 1: Growth of organisms in Blood culture.
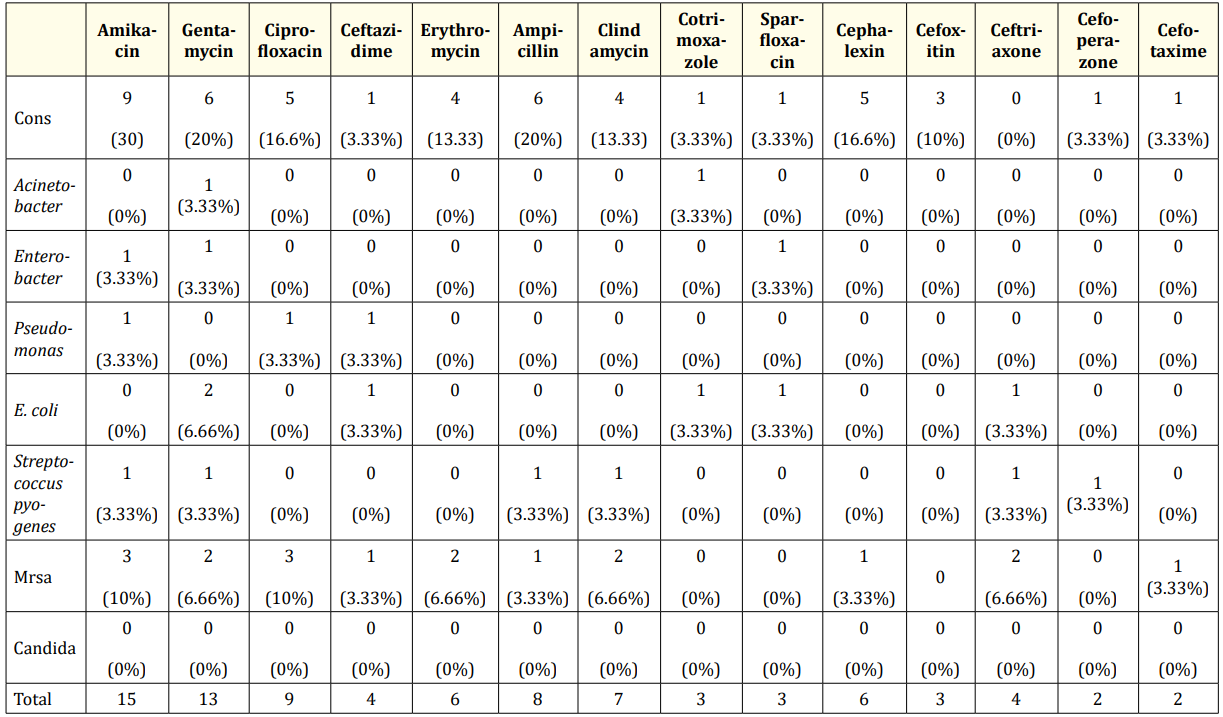
Table 2: Results of antibiotic sensitivity.
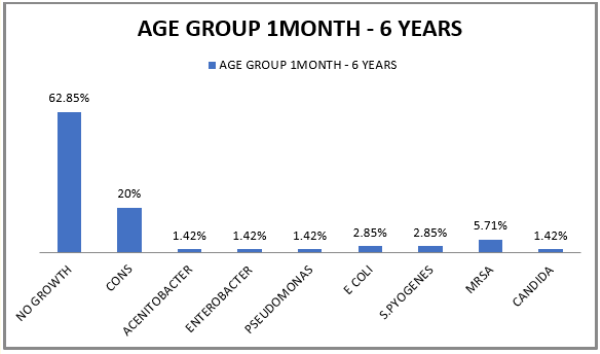
Figure 1: Growth of organisms in Blood culture.
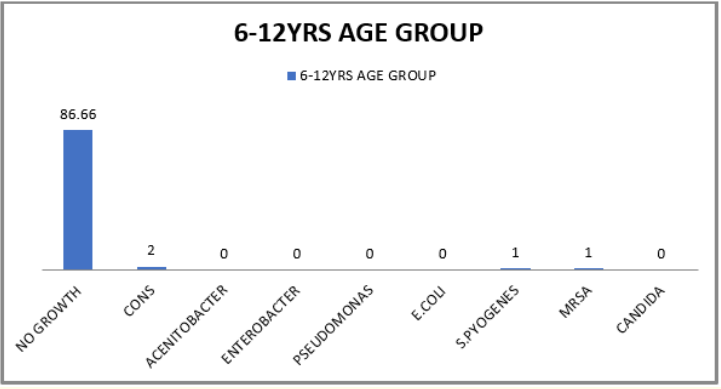
Figure 2: Predominant organisms in Age group 6 years to 12 years.
Of the 100 patients 30 (30%) patients showed culture positivity.70 patients were from 1 month to 6 years out of which 26 (37.14%) showed culture positivity in whom Coagulase negative Staphylococcus (CONS) was the predominant organism 14 (20%), followed by Methicillin resistant Staphylococcus aureus (MRSA) 4 (5.71%), followed by E. coli 2 (2.85%) and Streptococcus pyogenes 2 (2.85%) (Table 1 and figure 1). 30 patients were from the age group 6 years to 12 years out of which 4 (13.33%) were culture positive in whom Coagulase negative Staphylococcus (CONS) was the predominant organism 2 (6.66%) followed by Streptococcus pyogenes 1 (3.33%) and Methicillin resistant Staphylococcus aureus (MRSA) 1 (3.33%) (Table 1 and figure 2).
The results of the antibiotic sensitivity testing (Table 2) revealed that most of the isolates were sensitive to Amikacin.
This study was conducted in order to determine the predominant organisms causing septicaemia in the two age groups and their antibiotic sensitivity pattern in our hospital.
Coagulase-negative staphylococci are now being recognized as a common cause of nosocomial infections in intensive care units, even though not all positive blood cultures of CONS represent true septicaemia because CONS in the skin flora commonly causes contamination of blood cultures [10]. In the present study gram positive bacteria were the most predominant isolates, among which Coagulase negative Staphylococcus (CONS) [1 month to 6 years 14 (20%) and 6 years to 12 years 2 (6.66%)] however similar results were noticed by others [10-12]. Paediatric oncology patients (mainly leukaemia and lymphoma), bone marrow transplant recipients, and children with burns are at high risk for acquiring CONS bloodstream infections [13,14]. CONS infections represent 35 to 40 per cent of all bacteraemia in febrile neutropenic cancer patients undergoing treatment [14,15]. Patients with an indwelling medical device such as a central venous catheter (CVC), ventriculoperitoneal shunt, peritoneal dialysis catheter, prosthetic valve, prosthetic joint, vascular graft and prosthesis, haemodialysis shunt, pacemaker, or scalp electrode are prone to develop CONS infections. Though CONS is usually considered as a skin contaminant the presence of this bacteria in blood in critically ill children should be treated especially 3 days after admission with an indwelling catheter in place [16].
The antibiotics which were used were based on the standard protocol of the hospital and our department policies, which are changed regularly pending the culture reports and infectious committee recommendations. The other causative organisms were MRSA 4 (5.71%), E. coli 2 (2.85%) and Streptococcus pyogenes 2 (2.85%) in children between 1month to 6 years. MRSA 1 (3.33%) and Streptococcus pyogenes 1 (3.33%) in children between 6 years to 12 years. The antibiotic sensitivity varies at different times in the same hospital due to the emergence of resistant organism as a result of unregulated use of antibiotics. This can be avoided by the usage of a drug to which the organism is susceptible. From this study, it was suggested that the empirical treatment should consist of Amikacin until the findings of culture and sensitivity are done, as most of the organisms found in our PICU were sensitive to Amikacin.
The commonest organism causing sepsis in PICU is Coagulase negative Staphylococcus and this organisms have shown sensitivity to Amikacin.
The microbial aetiology of septicaemia is diverse. Thus, every PICU in charge should emphasize the mortal importance of a regular periodic testing of the microbial bacterial spectrum and their sensitivity to drugs in order to formulate a standard antibiotic regimen for PICU.
Copyright: © 2021 Edwin Dias., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.