Masroor H Sharfi*, Mohamed H Mashaly, Abdelmonem Helal, Abdullah A Al-Shehri, Osama Abdelaziz and Abdul Hadi Al-Ghamdi
Pediatric Cardiology Department, King Faisal Specialist Hospital and RC, Jeddah, Saudi Arabia
*Corresponding Author: Masroor H Sharfi, Assistant Consultant, Pediatric Cardiology Department, King Faisal Specialist Hospital and RC, Jeddah, Saudi Arabia.
Received: June 26, 2021; Published: July 14, 2021
Citation: Masroor H Sharfi., et al. “Association of Different Post-Operative Complications with Cardiac Troponin I and Cardiopulmonary Bypasses”. Acta Scientific Paediatrics 4.8 (2021): 41-46.
Background: Cardiac troponin I (cT-I) is considered as gold standard due to its increased sensitivity and specific markers for myocardial infraction and accordingly, it is used in the diagnosis of myocardial infarction in patients with acute coronary syndrome. Necrosis and myocardial damage occur as a result of conditions following postoperative myocardial ischemia.
Objective: This study is aimed to examine association between elevated cardiac troponin-I (cT-I) levels as cardiac biomarker and its association with the development of post cardiac surgery complications after cardiopulmonary bypass in paediatric population.
Methodology: This prospective study was conducted to monitor cardiopulmonary bypass post-operative complications in response to cardiac troponin-I (cT-I) levels in paediatric population to examine, particular patterns prognostic significance.
Results: A total of 190 paediatric patients with congenital heart defect were enrolled in the study. Most frequently observed cardiac lesion in CPB group was atrial septal defect (ASD) 27% and ventricular septal defect (VSD) 5% in CPB with ventricular incision group. A significant correlation was observed in both acute kidney injury incidence (P < 0.01) in both CPB and CPB with ventricular incision groups. Also, statistically significant correlation was observed in both groups in relation to hypo perfusion injuries increasing admission duration to CTICU (P < 0.03).
Conclusion: The current study confirmed that cT-I trends correlate with clinical outcome in paediatric patients with cardiopulmonary bypass specially in post-operative prognostic monitoring. The rate of morbidity and mortality in the patients diagnosed with myocardial injury can be decreased by improving perioperative management.
Keywords: Cardiopulmonary Bypass; Cardiac Troponin-I; Sensitivity
Post-cardiac period is considered as a crucial time since it is associated with bleeding, arrhythmias, heart failure, neurological disorders, infections, organ failure, decreased cardiac output, and respiratory failure. Deaths of the majority of cardiac patients occur at time of their admission into the Cardiac Intensive Care Unit (CICU) [1,2]. In open-heart surgery patients, cardiac hypothermic conditions require placement of cardiologic cold solution on a cardiopulmonary bypass (CPB) pump [3]. Various complications are associated with CPB such as inflammatory reactions caused by the spinal exertion of blood within the tubes and synthetic filters. This condition increases permeability of vascular wall, which results in the outflow of intravascular fluid in the interstitial spaces [1,4]. Systemic inflammatory response is generated as a result of tissue edema that leads to organ failure. Other complications of CPB include coagulation disorders, embolisms, electrolyte imbalances, and acute respiratory distress syndrome [3].
Troponin is a complex of three regulatory proteins: C, I, and T; it is released during the takedown of cardiomyocytes and plays and important role in the contraction of cardiac muscles [5]. Increase in troponin level in blood circulation causes mechanical damage to cell takedown because of cell apoptosis that occurs during inflammatory reactions. Troponin test is usually conducted to monitor the response towards a medical intervention. Myocardial tissue gets damaged mainly because of surgical manipulation or irritation during the cardiac surgical investigation; however, myocardial tissue damage is likely to occur during aortic surgery. One of the previous studies have confirmed inadequate intraoperative defibrillation and myocardial protection as the main causes of cell takedown that further increased troponin level [6]. Therefore, it has been reported that increased level of troponin depends on operative cardiac intervention in early post-operative courses [5].
The chances of a constant and consistent increase in biomarkers (troponin I) followed by cardiac surgical interventions are very high, depending on type of surgery, quality of myocardial protection, low levels of vasoactive inotropic score, and duration of ischemic cross clamp time [7-11]. Cardiac troponin T (cT-I) is considered as a significant marker of perioperative myocardial damage because of increased sensitivity. Previous studies have shown rise in bimodal post-operative cT-I with early peak occurring at 6 hours and later peak occurring at approximately 24 - 36 hours [12,13].
Postoperative myocardial ischemia conditions are likely to result in necrosis and myocardial damage. It is difficult to categorize the standard techniques and biochemical markers associated with post-cardiac condition and acute ischemic myocardial injury [14].
In the diagnosis of myocardial infarction in patients with acute coronary syndrome, cT-I are considered as gold standard due to their increased sensitivity and specific markers that highlight myocardial infarction. However, interpretation of releases of cT-I and development of post-surgery complications is a complicated process. Considering short- and medium-term outcomes, some of the previous studies have revealed increased significance of evaluation of post-operative troponin. Therefore, the current study aims to assess the association of post-operative complications with cT-I and CPB.
This study is aimed to examine association between elevated cardiac troponin-I (cT-I) levels as cardiac biomarker and its association with the development of post cardiac surgery complications after cardiopulmonary bypass in paediatric population.
This prospective study was conducted to monitor cardiopulmonary bypass post-operative complications in response to cardiac troponin-I (cT-I) levels in paediatric population to examine, particular patterns prognostic significance. The study was conducted over the period of December 2018 to March 2020 at post-operative Intensive care unit of New Children Hospital (NCH), Cairo University, Egypt.
Total 195 paediatric patients were enrolled prospectively in the study, aged (1 month to 5 year) with diagnosis and active complain of congenital heart defect and underwent cardiac surgery. The sample size was calculated using WHO calculator. Patients were categorized into two group’s post-operative surgery (i) paediatric patients with cardiopulmonary bypass only (ii) paediatric patients on cardiopulmonary bypass with need to perform resect muscle or ventriculotomy (ventricular incision). Out of 195 patients, 2 paediatric patients expire post-operatively and 3 patients lost to follow with no further visits to hospital, rendering a total of 190 enrolled patients.
The study included pediatric population aged 1 month to 5-year, male and female genders, pre- and post-operative cardiopulmonary resuscitation, cardiac lesion history, mechanical ventilation duration, re-intubation incidence with primary cardiac diagnosis. The study excluded all adult cardiopulmonary patients, pregnant women, paediatric patients whose parents were not willing to fill informed consent. After patient’s enrollment, two independent researchers explained the aim of the study to all enrolled participants parents and informed consent were obtained from parents/ guardians. At the baseline demographics, patient medical and surgical history was obtained. The post-operative variables were collected to examine troponin-I patterns including “VIS- Vasoactive inotrope score” at the time of TI sample collection, post-operative cardiac function ECG. Post-operative end organ damage was monitored or hypo perfusion injury in enrolled patients including acute kidney injury (AKI), pancreatitis, “NEC- necrotizing enterocolitis” and requirement of cardiothoracic intensive care unit or mechanical circulatory support.
In all paediatric patients underwent cardiopulmonary bypass, surgical details as per “STAT – Society of Thoracic Surgeons-European Association for Cardio Thoracic Surgery” were monitored to calculate duration of bypass, mortality score, STAT category, intraoperative complications DHCA duration and cross clamping time. Nido cardioplegia solution was used to attain diastolic arrest. Except for DHCA cases, regular systemic moderate hypothermia (24 - 32°C) was used for CPB patients.
Laboratory examination including blood sample was calculated pre-operatively at baseline and post-operatively at a follow-up of 4, 8, 12, 24 and 48 hours respectively. Within one hour of sample collection, all samples were processed and Troponin-I levels were measured through fluorescence immunoassay. All laboratory staff involved in processing processes was blinded of patient clinical status.
SPSS version 21 was used for data entry and analysis. Continuous variables were expressed as mean ± standard deviation. ANOVA was applied to perform multiple groups’ comparison and individual’s comparison of significance was determined. P- Value less than 0.05 was considered as significant.
A total of 190 paediatric patients with congenital heart defect were enrolled in the study with the mean age (3.27 ± 1.24) in patients on cardiopulmonary bypass group and (3.19 ± 1.07) in patients with CPB with ventricular incision with predominantly male (77%) in CPB group and female (37%) in CPB with ventricular incision (Table 1). Most frequently observed cardiac lesion in CPB group was atrial septal defect (ASD) 27% and ventricular septal defect (VSD) 5% in CPB with ventricular incision group. We observed significant correlation in VSD presence in both groups (P = 0.02). Similarly, considering duration of mechanical ventilation in postoperative patients, significant correlation was observed in patient recovery within 12 hours in both groups (P = <0.001). Most of the patients did not require re-intubation after surgery in both groups with statistically significant correlation (P = <0.001). There was no significant difference in duration of CPB was found (78.2 ± 3 2.4) in CPB group and (78.2 ± 32.4) in CPB with ventricular incision group (P = 0.19). Post CPB requirement for DHCA was required in 3 (2%) in CPB group and 15(8%) in CPB with ventilator incision. The results from the study showed no correlation between peak Troponin-I levels and STAT category (P = 0.58).
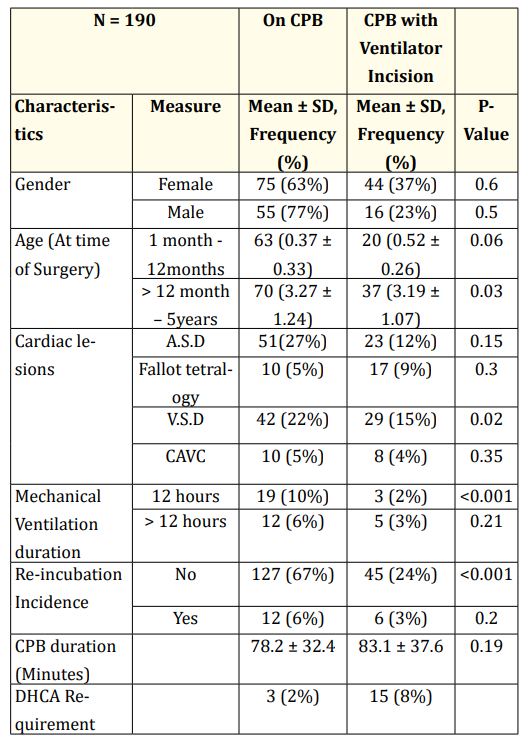
Table 1: Patient characteristics and post-operative data.
Considering the cardiac troponin-I (cT-I) trends in post-operative patients in both groups i.e. CPB and CPB with ventricular incision, the results (Table 2 and figure 1) demonstrated area under the curve (AUC) values of cT-I level were significantly different among two above mentioned groups with the least elevation with the post-operative time interval (0, 4, 8, 12, 24, 48 hours) examined in patients with only cardiopulmonary surgery and highest values in patient with cardiopulmonary surgery with ventricular incision (P < 0.003). Considering the cT-I trends and clinical outcome in post-operative patients with CPB, general trend was observed in cT-I individual at different points (Figure 1) (table 2) and significant overlapping was observed in both groups at different time points.

Table 2: Trends in values of postoperative T-I values based on type of surgery.

Figure 1: Post-operative Troponin-I level trends among CPB and CPB with ventricular incision group.
Table 3 demonstrates post-operative frequently observed compilations frequency in both groups (CPB and APB with ventricular incision) in association with post-operative rise in cardiac troponin-I (cT-I). Therefore, consistent increase in troponin-I levels was observed post-operatively. The results showed 89 (68%) paediatric patients after 8 hours of post-surgery had detectable cT-I levels only in CPB group. Whereas, 41 (31.5%) patients were reported of persistent elevation in Troponin-I levels even after 8 hours of surgery. Out of 41 paediatric patients, 23(12%) developed acute kidney injury; the rate of hypo perfusion injuries post-operatively lead to increased admission duration in CTICU was reported in 18 (9%) patients. Similarly, in CPB with ventricular incision group, 32 (17%) patients were reported of consistent elevation in Troponin-I levels leading to acute kidney injury, necrotizing enterocolitis was observed in 2 (1%) patients, pancreatitis was reported in 2(1%) patient and increase admission to cardiothoracic ICU with hypo perfusion injuries was observed in 23(12%) patients. A significant correlation was observed in both acute kidney injury incidence (P < 0.01) in both CPB and CPB with ventricular incision groups. Also, statistically significant correlation was observed in both groups in relation to hypo perfusion injuries increasing admission duration to CTICU (P < 0.03).

Table 3: Post-operative compilations frequency observed in both groups (CPB and APB with ventricular incision) in association with post-operative rise in Troponin-I level.
The results of the current study demonstrate the association of post-operative complications with cT-I and CPB. The main causes of the complications in the patients are long-term acute kidney injury, hypo perfusion injury, admission to CTICU and other organ disorders. Heart surgeries may also be associated with various arrhythmias and bleeding, along with CPB complications.
A previous study by [15] concluded the similar findings and revealed cT-I as a significant predictor of mortality due to stroke or heart failure in patients. This study also accomplished statistically significant values for doses of vasoactive support, duration of vasoactive support, duration of intubation, serum values of creatinine and hepatic function. However, the current study reveals no statistical significance for cT-I values with serum values of hepatic function, intubation duration, and length of hospital stay. The current study reveals that CPB values are significantly associated with milrinone duration and serum creatinine levels. These findings are opposed by [16] that showed no association of duration of CPB with clinical outcome and its results further showed no correlation between duration of CPB and aortic cross clamping with peak and total cT-I release.
Among the significant biomarkers that can be used to detect post-operative cardiac complications, troponin is the one which is linked with the changes in hypokinesis of cardiac wall, ECG findings, and stenosis or closure of coronary vessels. Previous studies have justified the significant role of cT-I in diagnosis and intervention therapy of myocardial infarction and chronic health failure [17-19]. The release of cardiac enzymes and elevated postoperative cardiac markers depends on the cardiac procedure and occurrence of ischemic cardiomyocyte injury. One of the previous studies has also reported varying cut-off points accompanied with diverse patient outcomes [20]. Just like the current study, another study [21] suggested that cT-I are used to assess patients with unexplainable hemodynamic instability and are identified in the form of cardiac image.
The results of current study suggest that troponin levels should be detected in the patients with increased risk as it would facilitate efficient use of the clinical resources. Measures could be devised for improving patient outcomes if patients at high risk are identified at early postoperative stage.
The current study confirmed that cT-I trends correlate with clinical outcome in paediatric patients with cardiopulmonary bypass specially in post-operative prognostic monitoring. The rate of morbidity and mortality in the patients diagnosed with myocardial injury can be decreased by improving perioperative management.
The study obtained a due ethical approval from New Children Hospital of Cairo University under the ethical approval code no I-081009.
The author declares no conflict of interest.
This study is self-funded.
Duly signed consent forms were obtained from all the recruited participants for obtaining their data from the hospital records before commencing the study procedure.
Copyright: © 2021 Masroor H Sharfi., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.