Isha Deshmukh1*, Fouziya Sultana2, Nishigandha Sonawane2 and Sushant Mane1
1Assistant Professor of Pediatrics, GGMC Mumbai, India
2Senior Resident in Pediatrics, GGMC, Mumbai, India
*Corresponding Author: Isha Deshmukh, Assistant Professor of Pediatrics, GGMC Mumbai, India.
Received: May 22, 2021; Published: July 05, 2021
Citation: Isha Deshmukh., et al. "Clinical Profile of Neonates Admitted in a Tertiary Care Neonatal Intensive Care Unit”. Acta Scientific Paediatrics 4.8 (2021): 02-05.
After birth the smooth transition to the extra-uterine environment is essential to help newborns survive the most critical period of life with good outcomes. We conducted a retrospective review of all neonates admitted in NICU during 24 months study period in GGMC and JJ NICU. Clinical determinants of neonatal sepsis in mother along with demographic clinical profile with laboratory corelation was the main purpose of the study conducted. A single centre retrospective study for the correlation of C reactive protein with blood culture in evaluation and treatment of neonatal sepsis in a tertiary care neonatal intensive care unit.
Keywords: C Reactive Protein; Neonatal Sepsis; Tertiary Care Neonatal Intensive Care Unit
Neonatal sepsis is a systemic infection occurring in infants at 0 to 28 days of life and is an important cause of morbidity and mortality of newborns [1]. Early-onset neonatal sepsis (EOS) has been variably defined based on the age at onset, with bacteraemia or bacterial meningitis occurring at 72h in infants hospitalized in the neonatal intensive care unit (NICU), versus 7 days in term infants [2-4]. In preterm infants, EOS is most consistently defined as occurring in the first 3 days of life and is caused by bacterial pathogens transmitted vertically from mother to infant before or during delivery [3]. Late-onset sepsis (LOS) is sepsis occurring after 72h in NICU infants and 7 days of life in term infants, has been variably defined as occurring up to the age of 90 or 120 days and may be caused by vertically or horizontally acquired pathogens [2,3,5-7].
The primary threatening signs and symptoms of neonatal sepsis are mostly nonspecific and can easily be mixed up with the non-infective causes. Nonspecific signs/symptoms make it very challenging to formulate a timely clinical diagnosis [8]. C-reactive protein (CRP) is the most extensively acute phase reactant studied so far and despite the ongoing rise (and fall) of new infection markers it still remains the preferred index in many neonatal intensive care units [9].
The study was conducted in Neonatal Intensive Care Unit of a tertiary care centre, Grant Medical College, Mumbai. All neonates born within January 2019 to December 2020 were enrolled in the study. The presenting clinical features of admitted neonates with suspected sepsis and values of CRP and blood culture report were recorded and results formulated. This study indicated that raised CRP could be used a marker for sepsis due to its high sensitivity, specificity, positive predictive value and negative predictive value.
Neonatal intensive care unit of GGMC, Mumbai is the main referral centre in the region that provided access to healthcare services for the suburban population. A 25 bedded level one nursery and NICU cares for all high risk preterm and term infants. A list of all newborns who were admitted to the NICU during the study period was obtained from the hospital electronic database. Data was extracted from the electronic medical records after a comprehensive review of the admission notes, daily progress notes, consultation notes, discharge summaries, problem lists, medication sheets and laboratory investigations. Demographic characteristics, risk factors in mother, indications for NICU admission, morbidities and outcomes were reported as documented by the admission doctor. Data collection was conducted by well trained pediatric resident and interns using pre-tested variables and documented in an excel spreadsheet.
In our unit, definitions of neonatal pathologies and outcomes are based on clinical presentation and supportive laboratory investigations utilizing the standard international criteria as applicable. Total NICU Admissions in JJ NICU over a period of 24 months were 972 from January 2019 to December 2020.
Birth weight was classified using the WHO weight classification system and categorized into low birth weight (LBW: Birth weight less than 2500 grams; very low birth weight (VLBW: birth weight less than 1500 grams) and extremely low birth weight (ELBW: Birth weight less than 1000 grams) (Table 1).
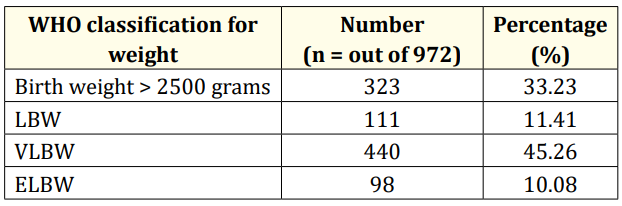
Table 1
Risk factors present in mother during antenatal period were classified based upon clinical maternal determinants for admission of newborns in neonatal intensive care unit (Table 2).
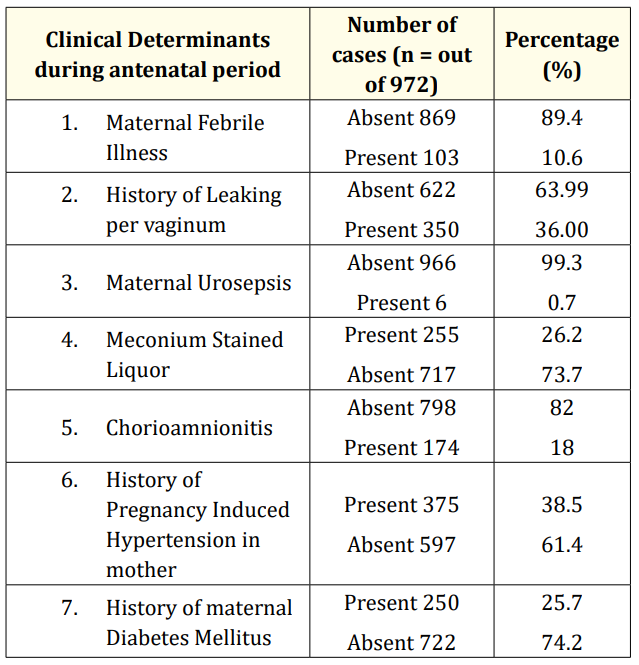
Table 2
Laboratory determinants were categorized based upon the laboratory values of investigations performed in neonates admitted in NICU (Table 3).
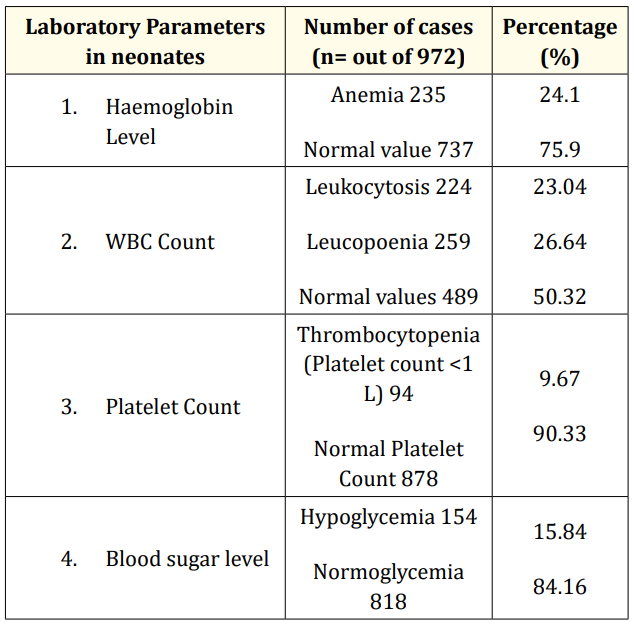
Table 3
Clinical characteristics of neonates admitted in NICU were segregated depending upon the clinical features present at birth during the stipulated study period (Table 4).
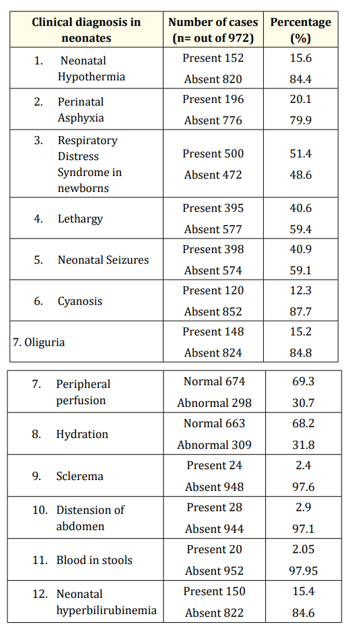
Table 4
Significant data analysis suggested the following results based upon clinical correlation between CRP and blood culture values (Table 5). In present study, the sensitivity and specificity of CRP against blood culture was 85.11% and 43.40% respectively. The positive and negative predictive value was 57.14% and 76.67% respectively. The diagnostic accuracy of CRP against blood culture in detecting neonatal septicemia was 63%. The neonates were detected to have neonatal sepsis on admission and clinical diagnosis and relevant investigations done for neonatal septicemia.
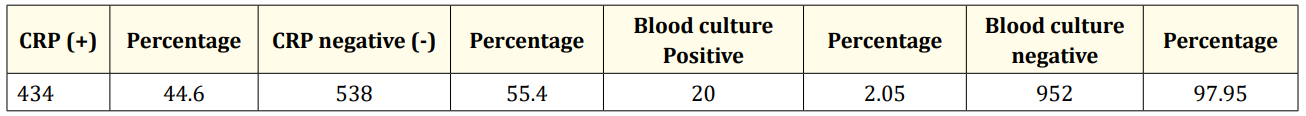
Table 5: Clinical co-relation between CRP and blood culture values. All blood culture positive cases had positive CRP value.
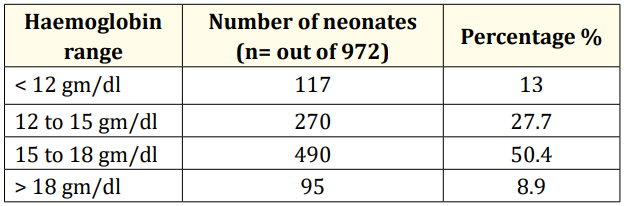
Table 6: Variations in haemoglobin content among neonates.
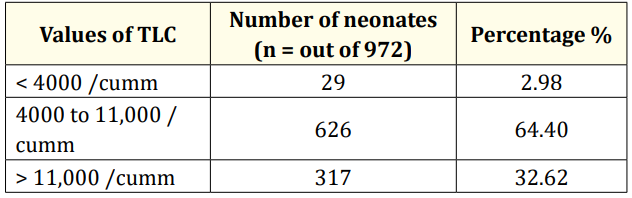
Table 7: Variations in total leukocyte count amongst neonates admitted in NICU.
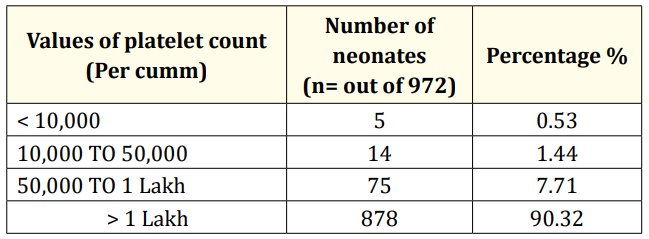
Table 8: Variations in platelet values.
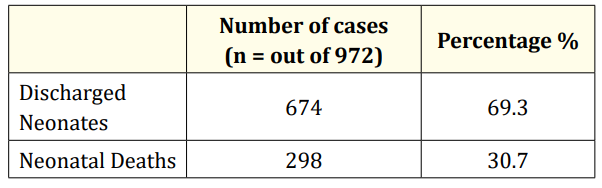
Table 9: Variation in outcomes of neonates amongst neonates admitted in NICU.
Neonatal septicemia is an important cause of neonatal morbidity and mortality. Neonatal sepsis is an important cause of hospital admission in the neonatal intensive care unit of our hospital. This study highlights the sensitivity and negative predictive value but lower specificity and positive predictive value of CRP and blood culture. The present study depicts a significant co-relation between culture positivity and CRP values. Blood culture is the gold standard for diagnosing septicemia. Several laboratory and clinical correlates are available to identify neonatal septicemia amongst NICU admitted neonates, hence this study classifies various determinants of neonatal diagnosis and associated maternal risk factors responsible for neonatal sepsis.
Ethical permission was granted by Ethics Committee at GGMC, Mumbai.
None.
None required since retrospective data.
This retrospective study was collectively conducted by residents and interns in NICU at JJ Hospital, Mumbai. I express my gratitude to the Head of the Pediatrics Department, Dr Nita Sutay and The Dean sir as well as supportive faculty members and staff involved in managing tertiary care level NICU at GGMC and JJ hospital, Mumbai.
Copyright: © 2021 Isha Deshmukh., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.