Chakradhar Maddela*
Neonatologist, Associate Professor of Paediatrics, Prathima Institute of Medical Sciences, Nagunoor, Karimnagar, India
*Corresponding Author: Chakradhar Maddela, Neonatologist, Associate Professor of Paediatrics, Prathima Institute of Medical Sciences, Nagunoor, Karimnagar, India.
Received: June 11, 2021 ; Published: June 30, 2021
Citation: Chakradhar Maddela. “Enhanced Post-Resuscitation Neonatal Care in Possibly Hypoxic Neonates at Resource Limited Setting: A Systematic Review ”. Acta Scientific Paediatrics 4.7 (2021): 77-86.
Introduction: Approximately 1 million babies are dying each year due to perinatal asphyxia. Ninety nine percent of these neonatal deaths are occurring in LMIC countries. Post resuscitated neonates are prone to develop HIE with multi-organ dysfunction and neuronal injury. Early prediction of HIE in asphyxiated neonates is critical for referral and cooling.
Aim: This study is carried out for recommending guidelines for ideal post resuscitation neonatal care in possibly hypoxic or ischemic neonates to prevent further neurological injury and death in resource limited setting.
Methods: It is a systematic review and data collected through online databases - PubMed, Medline, Cochrane database, Web of science, Scopus, Google Scholar, British nursing index and manual search. Initially Boolean phrase ‘post resuscitation neonatal care’ was used with AND / OR. Primary outcomes were death, neurological injury, feasibility and low cost.
Results: Fifteen study papers collected and critiqued with ‘CASP’ and ‘GRADE’ tools. Based on the theme of the study papers, the data categorized into three - identification (2 papers), monitoring (2 papers) and interventions for HIE (11 papers). Three papers were on cooling therapy.
Conclusion: One- and five-minute Apgar scores < 6 and neonatal resuscitation level 2 were simple predictors for HIE. When cooling not available and referral not feasible, potential interventions at low resource setting are early low dose Erythropoietin, early prophylactic theophylline, maintenance of normal blood glucose levels and no fluid restriction. Cooling is possible in LMIC countries with passive cooling and cooling with phase changing material.
Keywords: Post-Resuscitation Neonatal Care (PRNC); Term Infants; Late Preterm Infants; Neuroprotection; Neurodevelopmental Delay (NDD); Low Resource Setting (LRS); Low to Middle Income Countries (LMIC)
aEEG: Amplitude Integrated Electroencephalogram; AUC: Area Under Curve; BVM: Bag Valve Mask Ventilation; BE: Base Excess; CASP: Critically Appraisal Skill Programme; CI: Confidence Interval; DQ: Development Quotient; EEG: Electroencephalogram; Epo: Erythropoietin; HIE: Hypoxic: ischemic Encephalopathy; LMIC: Low to Middle Income Country; MA: Meta: analysis; MRI: Magnetic Resonance Imaging; NPV: Negative Predictive Value; NR: Neonatal Resuscitation; NDD: Neurodevelopmental Disability; NNT: Number Needed to Treat; OR: Odds Ratio; PRNC: Post Resuscitation Neonatal Care; PPV: Positive Predictive Value; PCM: Phase Changing Material; PRC: Post Resuscitation Care; RCT: Randomized Control Trial; ROC: Receiver Operating Characteristic Curve; RR: Relative Risk; Sn: Sensitivity; Sp: Specificity SR: Systematic Review; SIADH: Syndrome of Inappropriate Anti Diuretic Hormone Secretion; VLBW: Very Low Birth Weight
At global level, annually ten million babies do not initiate breathing at birth. Six million babies require initial resuscitation [1]. One million babies are dying due to perinatal asphyxia. Ninety-nine percent of neonatal deaths are occurring in low to middle income countries (LMIC) [2]. Among survivors from perinatal asphyxia [3], 25 - 60% are suffering from long-term neurodevelopmental disability [4].
Neonatal mortality rate (NMR) is high in India (NMR 23.5 in 2017 [5]). Two-thirds of infant mortality rate is contributed by neonatal deaths. Two-thirds of neonatal deaths are taking place during 1st week of life. Out of these, two-thirds of babies are dying within 24 hours. One-third of neonatal deaths are due to birth asphyxia and/birth injury. Thus, these figures [6] reflect the importance of first 24hours in human life in LMIC countries. At twin towns, Korutla and Metpally, Telangana state, India majority of deliveries take place at health care facilities. These are community health centres and private nursing homes. They are not well equipped with foetal monitoring devices and lack of neonatal intensive care units (NICU) within the premises. They have higher delivery case workload and lower ratio of doctor to patient and nurse to patient [7] to achieve the optimum maternal-neonatal care [8].
There is an urgent necessity to guide and recommend about ideal post-resuscitation neonatal care (PRNC) in these possibly hypoxic babies for preventing further neurological injury and multiorgan dysfunction [9]. Ten percent neonates do not initiate breathing at birth and require initial resuscitation. About 3 - 6% babies need BVM ventilation, less than 1% babies need chest compressions and 0.1% babies may require adrenaline administration.
Perinatal asphyxia is a devastating condition in neonates. Resuscitated neonates should be monitored in the immediate postnatal life for the early recognition of metabolic derangements and multiorgan dysfunction [10]. Appropriate interventions like cooling therapy should be initiated within the window period of six hours [11] or even later [12] to prevent further neurological deterioration. Therapeutic hypothermia is the standard treatment for moderate to severe hypoxic-ischemic encephalopathy (HIE) neonates [13].
This study is conducted to make guidelines for appropriate post-resuscitation care in possibly hypoxic neonates for preventing further neurological injury, organ dysfunction and neonatal deaths in a resource limited community health setting by systematic review.
Physicians and nurses contribute their clinical views and therapeutic interventions based on their background knowledge, experience and clinical situation by making their own clinical decisions. This may result in making suboptimal decisions or delayed decisions with delayed initiation of appropriate therapeutic care and interventions. Guidelines and protocols support evidence-based practice and facilitate decision making.
The term and late preterm (> 35 weeks gestational age) resuscitated infants at birth with bag value mask ventilation (BVM).
Intervention: Enhanced post resuscitation neonatal care.
Control: Standard post resuscitation neonatal care.
Outcomes: Feasibility/cost effectiveness/neonatal survival without major neurological deficit.
Inclusion criteria: Human, term and late preterm infants, post resuscitation care, neuroprotection and cost effectiveness.
Exclusion criteria: Animal studies, adult studies and very low birth weight infants (VLBW).
A comprehensive systematic literature search made in February 2020 through online databases PubMed, Medline, Scopus, Web of science, Google scholar, Cochrane database and British nursing index and manual search for the research topic ‘post resuscitation neonatal care’. A manageable data collected by applying filters and a four phrased PRISMA flow chart prepared [14].
Initially Boolean phrase with ‘post resuscitation neonatal care’ was searched by adding ADD/OR. Further search was also made with appropriate key words - asphyxia neonatorum (MeSH), perinatal asphyxia, high risk, neonatal care, neurological injury, low resource setting, LMIC and long-term outcomes.
Study search limited to English language as software not available to translate other language studies to English language. Study search limited to human studies, newborn population - term and late preterm and systematic reviews (SA). Animal studies were excluded. One hundred and five articles from online databases (PubMed/Medline 28, PubMed/MeSH 14, Scopus 15, Cochrane database of systematic reviews (CDSR) 24 and Web of Science 24 articles) and 19 articles from other sources were identified. The combined search resulted in 124 study articles. Fourteen articles were identified as duplicates and removed from the count. The remaining 110 full text articles were screened in accord to research question with abstracts and keywords and 85 articles were removed from the count for the following reasons:
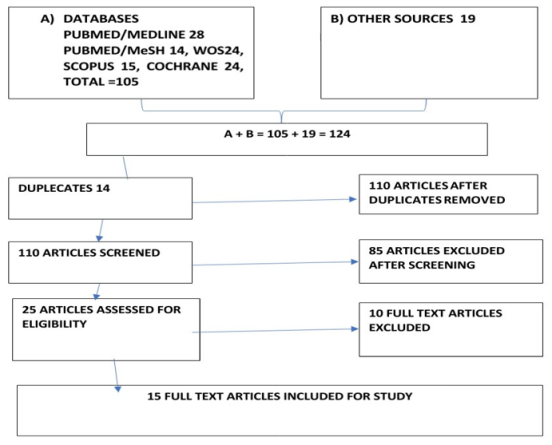
Flow Chart: PRISMA flow chart.
Quality assessment: Twenty-five articles subjected for critiquing with ‘Critical Appraisal Skills Programme, CASP’ [15] tool and 15 articles selected for study purpose. ‘GRADE’ quality of evidence and strength of recommendations is used for quality of evidence and strength of recommendations for evaluating study papers [16].
The collected data of 15 study articles are further studied with title, abstract and findings and categorised into following three groups based on theme - 1. Data on identification of HIE (2 study papers) 2. Data on monitoring of HIE (2 study papers) and 3. Data on therapeutic interventions for HIE (11 study papers)
Statement of findings: This study review included 15 study papers with 1686 study participants. The participants were term and late preterm infants. There were three systematic reviews, seven randomized control trials (RCT), four prospective studies and one observational study. Only one systematic review on fluid restriction in HIE infants did not recruit any RCT trial by inclusion criteria from author. There were four study papers on early identification of HIE with clinical, biochemical and amplitude integrated electroencephalography (aEEG) markers, eight papers on potential early therapeutic interventions for HIE in preventing neonatal mortality and morbidity and three papers on specific therapy for moderate to severe HIE. One paper among eight papers on therapeutic interventions was on prevention of renal dysfunction while remaining seven papers focused on prevention of neurological dysfunction or neonatal mortality. A total of eleven papers were on prevention of mortality and/or NDD. Thirteen papers were on low-cost strategies in HIE infant care. Two papers were on high-cost specific standard care for HIE infants.
Excluded study papers: Ten of twenty-five study papers were excluded from this review (Appendix A). When two study papers were available on same topic, weightage was given in the following order of preference - RCT trial, prospective trial and retrospective trial. Retrospective trials are prone for selection bias, attrition bias and non-blinding.
Quality of evidence: Substantial number of neonatal populations was recruited in this review. The estimates of therapeutic strategies effecting the outcomes, feasibility, low cost, death and disability were reasonable precise.
Table 1: Showing critique of individual study papers based on theme.
Bias: The following study papers were found low risk bias - 1. Tanigasalam V., et al. 2018, 2. Hunt and Osburn 2010, 3. Jenik K AG., et al. 2000, 4. Basu SK., et al. 2016, 5. Bhat MA., et al. 2009, 6. Young L., et al. 2016, 7. Malla RR., et al. 2017, 8. Aker., et al. 2019 and 9. Shankaran S., et al. 2005.
Table 2: Showing bias of individual papers.
Post resuscitation neonatal care should be essential and mandatory component in post asphyxiated infants. A structured and organized organ-oriented post resuscitation care is needed for neonatal survival and neuroprotection. On carrying out this process, the beneficial effects of therapeutic strategies when significantly outweigh the side effects can be included as early effective strategies to treat these infants in the absence of specific therapy for HIE like therapeutic hypothermia.
Identification of HIE: Early identification of (< 6 hours) HIE is crucial in directing and administering specific neuro-protective strategies and supportive therapy [17].
White., et al. (2012) showed clinical markers (1 minute Apgar scores and neonatal resuscitation (NR) level were better predictive than biochemical markers in predicting HIE (univariate analysis). Apgar scores and umbilical blood lactate were simple and reliable in predicting HIE. Multivariate analysis revealed combined NR level (levels of neonatal resuscitation (NR) were 0 = no NR, 1=NR with supplemental oxygen, 2=NR with BVM, 3=NR with endotracheal intubation +/- ventilation, 4=NR with external cardiac massage and 5=NR with adrenal administration) and lactate level were accurate in predicting moderate to severe HIE. All these markers carried high specificity, NPV (99.12%, 99.98%) and accuracy (99.10%).
Talati A J., et al. (2005) prepared a clinical scoring system with 3 variables [(5 minute Apgar score, cord blood base excess, BE (< 60 minutes) and NR level (no intubation, intubation and intubation + adrenaline)]. A score of > 5 predicted moderate to severe HIE with 90% positive predictive value (PPV).
Monitoring of HIE: Toet., et al. (1999) used aEEG at 3 and 6 hours for diagnostic and prognostic purpose. Abnormal aEEG patterns (burst suppression, flat trace and very low voltage trace) at 3 and 6 hours carried adverse outcome (death and NDD) (Sn 0.85 and 0.91, Sp 0.77 and 0.86, PPV 78% and 86% and NPV 84% and 91% respectively). Continuous normal voltage pattern at 3 hours was associated with good outcome.
Jones R., et al. (2017) in a retrospective study found 5-minute Apgar scores < 6 (0.81 (0.64 - 0.98, p = 0.001), Troponin T (0.81 (0.64 - 0.98, p = 0.004) and alanine amino transferase (ALT) (0.78 (0.60 - 0.96, p = 0.004) were strong predictors of HIE in asphyxiated infants with abnormal aEEG background. Hence, these variables could be used as surrogate for aEEG in resource limited setting.
Potential therapeutic strategies for HIE: After initial primary perinatal hypoxic injury, adaptive changes take place resulting in redistribution of cardiac output with vasoconstriction of non vital organs and vasodilatation of vital organs. The HIE infants prone to develop systemic hypotension and multiorgan dysfunction [18].
Fluid management is vital in maintaining hydration, blood pressure and systemic and cerebral perfusion while facing renal dysfunction and cerebral oedema. A common practice exists in restricting fluids to 2/3rd of maintenance.
Tanigasalam., et al. (2018) found that there was no important difference among fluid restricted and normal fluid maintenance for death and major disability in a RCT trial. Moreover the fluid restricted group had showed hazardous increased hypoglycaemia, shock, weight loss and acute kidney injury.
Hemodynamic instability following perinatal asphyxia is a common finding and results in systemic hypotension and redistribution of cardiac output. This results in efficient oxygen delivery to vital organs at the expense of peripheral organs. In more severe cases, there is shift of blood from high resistance foetus to low resistance placenta resulting in circulatory shock [19]. These infants also develop myocardial dysfunction and fall in stroke volume. Thus, managing systemic hypotension and organ perfusion are essential. It is common practice to treat these infants with low dose dopamine infusion in NICUs. Hunt and Osburn (2010) in SR found no important difference among low dose dopamine infusion group and placebo group for primary outcomes (RR 0.33, 95% CI 0.04, 2.48) and hospital stay.
Seventy percent of post asphyxiated infants experience renal dysfunction [20]. Oliguria and raised serum creatinine are common findings. Adenosine mediated vasoconstriction with resultant fall in GFR and oliguria could be the mechanism. Theophylline is a nonspecific adenosine antagonist and got potential role in renal dysfunction in asphyxiated term infants.
Jenik., et al. (2000) showed early administration (<1hour) of single dose theophylline at 8mg/kg/dose was effective in reducing renal dysfunction in HIE infants. Only 17% (4/24) infants in theophylline group and 55% (15/27) in placebo group had severe renal dysfunction (RR 0.30, 95% CI 0.12 - 0.78). Renal tubular function was better in theophylline group as evidenced with reduced urinary beta2 microglobulin levels than placebo (5.01 +/- 2.3 mg/L Vs 11.5 +/- 7.1 mg/L; p = 0.005).
Glucose is major source of energy for brain. Animal studies showed both hypo- and hyperglycaemia were injurious to asphyxiated brain. Foetus is an obligatory parasite. At birth, intrauterine parenteral nutrition is terminated abruptly and euglycaemic state is maintained by liver glycogen, hormonal regulation and enteral or parenteral nutrition. In asphyxiated infant, these processes may be blunted and prone for deranged glucose homeostasis [21]. Basu., et al. (2016) showed early < 12 hours hypo-hyperglycaemia (p = 0.011), recurrent hypoglycaemia (OR 2.1; 95%CI 0.52 - 8.3) and recurrent hyperglycaemias (OR 4.5, 95% CI 1.7 - 12.0) were associated with unfavourable outcome in randomized 214 HIE infants for HT.
After perinatal asphyxia and primary neuronal injury, an excitatory neurotransmitter glutamate is released in large amounts with decreased reuptake at post-synaptic level. Glutamate acts on N-methyl-D-aspartate (NMDA) receptor, induces increased ionic calcium influx and neuronal damage [22]. Magnesium is a NMDA receptor antagonist and at higher concentration may protect the brain from glutamate induced excito-toxicity.
Bhat., et al. (2009) showed the beneficial effects of early magnesium sulphate infusion in HIE infants on short-term neurological outcomes (OR 5.5; 95% CI 1.2 - 23.6, p = 0.02). Magnesium group showed fewer neurological abnormalities, lesser abnormal findings on Computerized tomography imaging and EEG with better established oral feeds at discharge.
After primary neuronal injury, a second phase of neuronal injury occurs on reperfusion after a latent period of six hours in asphyxiated infants. The possible mechanisms involved are oxidative free radicle injury, increased intracellular calcium influx, excitatory neurotransmitter accumulation, cytotoxic cerebral oedema and apoptosis (Volpe., et al. 2007). Seizures are very often seen in HIE infants [23]. Phenobarbitone is a low cost, easily available GABA agonist and had potential role in perinatal asphyxia. Young., et al. (2016) in a systematic review showed early prophylactic phenobarbitone significantly reduced risk of seizures (6 RCTs) (RR 0.62, 95% CI 0.48 - 0.81; RD-0.81, 95% CI 0.27 - 0.09; NNTB 5, 95 CI 4 - 11; 6RCTs, 319 infants) but no impact on combined mortality and major NDD (8 RCTs) except in one trial (Hall 1998) (31 infants, RR 0.33; 95% CI 0.14 - 0.78, RR-0.55, 95% CI -0.84 - 0.25; NNTB 2, 95% CI 1-4).
Erythropoietin (Epo) is essential for development, function and repair of neonatal brain. Epo exhibits anti-inflammatory, neurotrophic and neuroprotective effects. Early low dose (Epo 500 U/kg) erythropoietin monotherapy in a RCT trial by Malla., et al. (2017) showed encouraging results with applicability in low resource setting. The primary outcomes, death and major NDD were low in Epo group (RR 0.57; 95% CI 0.38 - 0.85; NNT 4) and in secondary outcomes, more infants were survived without neurological abnormalities in treatment group than placebo group (RR 0.65; 95% CI 0.45 - 0.94, p = 0.016).
Therapeutic hypothermia is a standard for neuroprotection in moderate to severe HIE infants. Therapeutic hypothermia is not easily available in LMIC countries and indeed it is most required. Hence, alternative low-cost methods of cooling were tried with different success [24].
Passive cooling is a simple, low cost but effective method of cooling when HT is not available. Kendall., et al. (2010) in a prospective study with 39 referred HIE infants to eight cooling centres transported by London Neonatal Transport Service showed 89% neonates attained target temperature by passive cooling alone. Zero percent, 15% and 67% of neonates achieved target temperature at referral centre, on arrival of transport team and reaching at cooling respectively.
Therapeutic hypothermia with phase changing material (PCM) is a new hope for HIE infants in resource limited setting. Aker., et al. (2019) showed the efficiency of PCM in inducing therapeutic hypothermia with favourable outcomes (0.026; 95% CI 0.004 - 0.48, p = 0.023). Lesser moderate to severe abnormalities noticed in cooled babies than non-cooled babies on brain MRI imaging (p = 0.007).
Shankaran S., et al. (2005) in a RCT trial tested whole body servo control therapeutic hypothermia in randomized HIE infants for death and or NDD at 18-22 months of age. Composite death and major disability (45/102 = 44% Vs 64/103 = 62%) neonatal mortality (24% Vs 37%, RR 0.68; 95% CI 0.44 - 1.05; p = 0.08) and major disability were less in hypothermia group than in control group.
Negative findings of study papers: In predicting HIE in asphyxiated infants, one study paper (White 2012) given cut off points for clinical predictors - Apgar score as 5.5 and NR level as 1.5 and adjusted round figures were not mentioned in discussion. Cut off points are very useful in predicting and selecting HIE cases for future action. Decimal figures pose clinical dilemma for care giving physician (figures 6 instead of 5.5 for Apgar scores and figure 2 for NR level instead of 1.5). Kecskes (2010) published SR paper in CDSR on fluid restriction in HIE term infants without study paper. Hunt and Osborn (2010) recruited single study paper (DiSessa
1981) with small study population (n = 14) in CDSR on low dose dopamine infusion in HIE infants. As the study population is too small, the study results cannot be extrapolated to population in large. Aker (2019) in THIN RCT trial on PCM therapeutic hypothermia showed beneficial results mainly in moderate HIE cases and there were very few cases of severe HIE on follow up (only two cases).
Selective evidence in the management of each component of post resuscitation care (PRC) is available in literature but pooled evidence in the management for different components of PRC is scarce. This study adds the need of pooled evidence in management for components of PRNC in HIE infants with special relevance to low resource setting. Three essential components of post resuscitation neonatal care were identified and includes - 1) early identification of HIE 2) monitoring during post resuscitation care and 3) early therapeutic interventions to improve multi-organ dysfunction and prevent neurological injury. These component strategies for PRNC were in practice in advanced NICU centres. This review adds translated evidence of these component strategies of PRNC to low resource setting. Unless we predict HIE during early 6 hours in asphyxiated infants, neither referral to higher centre nor early protective interventions might possible. This study identified 1 and 5 minute Apgar score of < 6 and level 2 neonatal resuscitation were simple, low cost predictors for identifying HIE cases immediately after birth for quick referral or early initiation of therapeutic interventions. The aEEG monitoring is not easily available in LMIC countries, hence 5-minute Apgar score, Troponin T and alanine aminotransferase (ALT) could be used as surrogate for aEEG in LRS. The early therapeutic interventions identified by this review are Epo therapy, prophylactic theophylline, maintaining euglycaemic state by early identification and intervention for hypo and hyperglycaemia, no fluid restriction and prophylactic phenobarbitone for reducing seizures. Passive cooling and cooling with PCM are new hope for cooling therapy at area hospitals, teaching hospitals and tertiary care NICU centres at district level.
What is known about this topic PRNC? There is uncertainty among medical practitioners regarding management of moderate to severe HIE cases at LRS in LMIC.
Appendix A: Excluded study papers with reason.
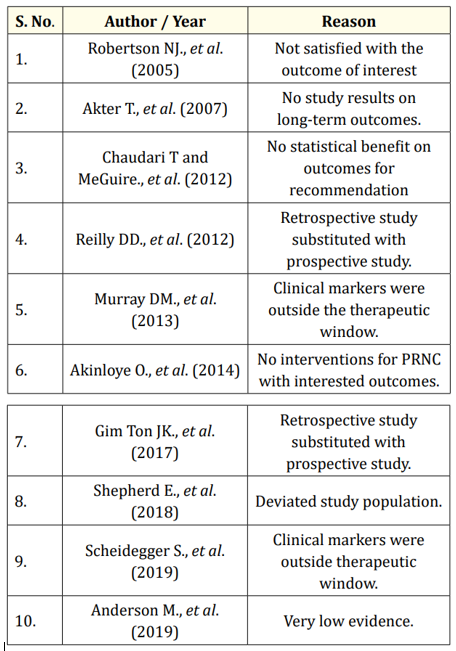
Appendix A
Continuous invasive monitoring of HIE infants, aEEG/EEG monitoring and specific organ perfusion with Near Infrared Spectroscopy is not feasible in LMIC countries. Many HIE infants need ventilation during NICU stay. These facilities are not easily available in resource limited settings. There is a need of further research in these fields and to prepare low cost alternative devices to fulfil these gaps.
Role of magnesium and inotropes in the management of asphyxiated infants need further studies with large population before recommendation.
No conflicts of interest.
There is no sponsoring agency for this study.
Copyright: © 2021 Chakradhar Maddela. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.