Sarra Osheik Ahmed Shareif1, Eiman Bakri Ali2 and Satti Abdelrahim Satti3*
1Pediatric Registrar, Gaafar Ibn Auf Pediatric Hospital, Khartoum, Sudan
2Associate Professor of Pediatrics and Child Health, International University of Africa, Khartoum, Sudan
3Professor of Pediatrics and Child Health, Almughtarabeen University, Khartoum,
Sudan
*Corresponding Author: Satti Abdelrahim Satti, Professor of Pediatrics and Child Health, Almughtarabeen University, Khartoum, Sudan.
Received: April 19, 2021; Published: June 23, 2021
Citation: Satti Abdelrahim Satti., et al. “Utility of Neutrophil to Lymphocyte Ratio and Platelets Count in Predicting Treatment Success in Preterm Neonates with Patent Ductus Arteriosus, in Gaafar Ibn Ouf Specialized Hospital, Khartoum, Sudan. January 2018 to January 2020”. Acta Scientific Paediatrics 4.8 (2021): 31-35.
Background: Congenital heart disease (CHD) is the most common congenital disorder in newborns. Critical CHD, defined as those requiring surgery or catheter based intervention in the first year of life, occurs in approximately 25% of those with CHD. Patent Ductus Arteriosus (PDA) may result in significant infant morbidity and mortality rates that approach 30%. It is one of the most common congenital heart defects, accounting for 5% - 10% of all congenital heart disease in term infants, and 33% - 55% in preterm. Preterm infants are at an increased risk of PDA compared to term neonates. Early diagnosis is essential, as delaying treatment may decrease the chance of success. Platelet aggregation has a minor role in ductal closure. NLR has been demonstrated to play a predictive role in the prognosis of chronic and acute inflammatory processes such as in aerodynamically significant PDA among preterms.
Objective: To study Utility of Neutrophil to Lymphocyte Ratio and Platelets Count in Predicting Treatment Success in Preterm Neonates with Patent Ductus Arteriosus, in Gaafar Ibn Ouf specialized Hospital from January 2018 - January 2020.
Methods: An observational, descriptive, cross sectional and hospital based study conducted in Gaafar Ibn Ouf Specialized Hospital from January 2018 - January 2020. Forty study participants were included. The relevant data was extracted from these records, prepared, entered and analyzed using SPSS version 25.0. Also, a Questionnaire form was used.
Results: A total number of 40 preterm neonates with Isolated PDA were studied. 70% were in age group of less than 7 days. Male to Female ratio was 1.4:1. 62% were of moderate to late preterm and 70% were low birth weight. Medical complications that had been encountered were Heart failure, followed by neonatal sepsis then pneumonia and RDS as well as metabolic acidosis, neonatal jaundice and DIC, and a minority developed NEC. Regarding management: Almost half received paracetamol, a quarter took diuretics, 7.7% were given surfactant and in fluid restriction plan. Only 5.2% underwent surgical closure and 3.9% were put on mechanical ventilation or CPAP. On admission 67.5% had neutrophils count of ≥ 50 and 32.5% had neutrophils count < 50. While At discharge those who had neutrophils count < 50 were 40% and with count ≥ 50 were 60%. On admission 90% their lymphocyte count was < 50 and in 10% was ≥ 50. The same percentages was recorded at discharge. On admission 72.5%of studied participants had platelets count < 150 and 27.5% had platelets count ≥ 150. At discharge 65% had platelets count < 150, while 35% had platelets count ≥ 150. On admission 36% their initial neutrophil to lymphocyte ratio was < 1, 1-2 in 38% and > 2 in 26%. On discharge 42% had neutrophils to lymphocytes ratio < 1, 40% had ratio > 2 and only 18% had ratio of 1 - 2. 82% of participants discharged in a good condition, while only 18% died. Thrombocytopenia is associated with good outcome. No significant association was found between neutrophil to lymphocyte ratio and the outcome. Improvement of prevention and early radical management of Patent Ductus Arteriosus may provide effective measures directed at reducing the burden of both morbidity and mortality in the country.
Keywords: Preterms; Patent Ductus Arteriosus; Platelets; Neutrophil to Lymphocyte Ratio; Sudan
Congenital heart disease (CHD) is the most common congenital disorder in newborns. Critical CHD, defined as those requiring surgery or catheter based intervention in the first year of life, occurs in approximately 25 percent of those with CHD [1]. Patent ductus arteriosus (PDA) [2] may result in significant infant morbidity and mortality rates that approach 30%. Patent ductus arteriosus (PDA) is one of the most common congenital heart defects, accounting for 5% - 10% of all congenital heart disease in term infants and it is one of the most common problems in preterm infants leading to potentially serious effects on several organ systems [2]. Its incidence may be as high as 60% among those with extremely low gestational age and in very low birth weight infants [3]. Increase in arterial pO2 and a drop in circulating PGE2 and blood pressure within the lumen of the ductus promotes constriction of the ductus [3].
In the neonate, however, persistent patency of the ductus arteriosus (DA) is associated with significant morbidity and mortality [4]. Early diagnosis of PDA is essential, as delaying treatment may decrease the chance of success [3,4]. Although several hypotheses have been introduced to date, the precise mechanisms of ductal closure were proposed to differ in preterm and full-term infants. In full-term infants, ductus closure is related with the decreasing blood flow both in the ductus lumen and vaso vasorum, leading to hypoxia in the vessel wall after birth. Platelet aggregation has a minor role in this setting [4]. Neutrophils - lymphocytes ratio (NLR) may be an indicator of systemic inflammation, as neutrophils and lymphocytes are thought to be significant in tumor immunology and inflammation. NLR has been demonstrated to play a predictive role in the prognosis of chronic and acute inflammatory processes such as in aerodynamically significant PDA among preterm [5]. NLR is inexpensive and easy-to-perform test which is used as an inflammatory indicator especially in patients with cardiovascular disease [6]. Significant correlations were observed between body weight and N/L ratio.
This study aimed to study the utility of neutrophil to lymphocyte ratio and platelets count in diagnosis and predicting treatment success in preterm neonates with patent ductus arteriosus, in Gaafar ibn Ouf specialized Hospital, January 2018 - January 2020.
To study the utility of neutrophil to lymphocyte ratio and platelets count in predicting treatment success in preterm neonates with Patent Ductus Arteriosus, in Gaafar Ibn Ouf Specialized Hospital.
This is a cross-sectional, descriptive and hospital-based study conducted at Gaafar Ibn Ouf Paediatric Specialized Hospital, in Khartoum City, Sudan. The study was conducted from September 2020 to February 2021 covering records of preterm neonates with PDA attending the hospital from January 2018 to January 2020. Gestational age of prematures was between 26 weeks - and 37 weeks) diagnosed as Patent Ductus Arteriosus by ECHO.
The statistical records of all preterm neonates with PDA admitted during the study period was collected. The relevant data was extracted from these records. Also, a Questionnaire form was used. Study variables collected include Demographical and Clinical characteristics plus investigations done and the outcome. Data Analysis was made using SPSS Ver.25 T test and Chi Square test were used and P-vale < 0.05 was considered to be the significant value.
Informed consent from ethical research committee of Sudan medical specialization board and administrative authority of the Hospitals was obtained. Ethical approval was also obtained from national ethical committee at the federal ministry of health.
A total number of 40 preterm neonates with Isolated PDA were studied. 70% were in age group of less than 7 days, 24% in age group more than 14 days and only 6% in age group 7 - 14 days. Male to Female ratio was 1.4:1. 62% of study participants their gestational age was 32 to < 37 weeks and 38% were between 28 and < 32 weeks. 70% were low birth weight, 18% very low birth weight and only 12% extremely very low birth weight (Figure 1). Complications encountered were as follows (Figure 2). Heart failure in 61.4%, neonatal sepsis in 19.9%, pneumonia in 4.2% and RDS in 3.1%, as well as metabolic acidosis, neonatal jaundice and DIC, and 2.1% developed NEC.
Regarding management: 44.2% received paracetamol, 27.4% took diuretics, 7.7% were given surfactant and 7.7% were in fluid restriction plan. 5.2% underwent surgical closure and 3.9% were put on mechanical ventilation or CPAP. On admission 67.5% had neutrophils count of ≥ 50 and 32.5% had neutrophils count < 50. While At discharge those who had neutrophils count < 50 were 40% and with count ≥ 50 were 60%. On admission 90% their lymphocyte count was < 50 and in 10% was ≥ 50. The same percentages was recorded at discharge. On admission 72.5%of studied participants had platelets count < 150 and 27.5% had platelets count ≥ 150. At discharge 65% had platelets count < 150, while 35% had platelets count ≥150 (Table 1).
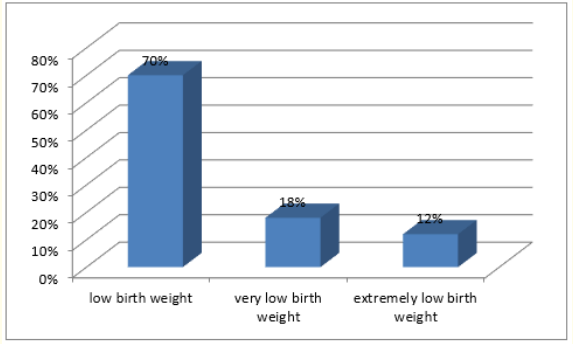
Figure 1: Distribution of birth weight among study participants.

participants.
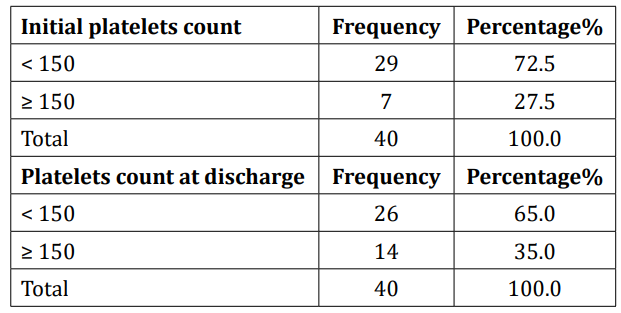
Table 1: Platelets count distribution among study participants on admission and discharge.
Almost two thirds (68%) of participants stayed at hospital for more than 14 days, 20% for less than 7 days and only 12% for 7 - 14 days. 82% of participants discharged in a good condition, while only 18% died. On admission 36% their initial neutrophil to lymphocyte ratio was < 1, 1 - 2 in 38% and > 2 in 26% (Figure 3). On discharge 42% had neutrophils to lymphocytes ratio < 1, 40% had ratio > 2 and only 18% had ratio of 1 - 2 (Figure 4).
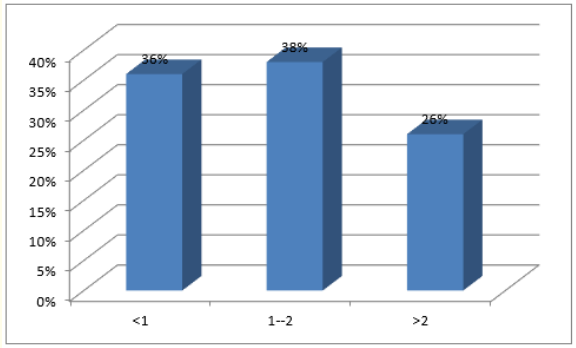
Figure 3: Initial neutrophils to lymphocytes ratio.
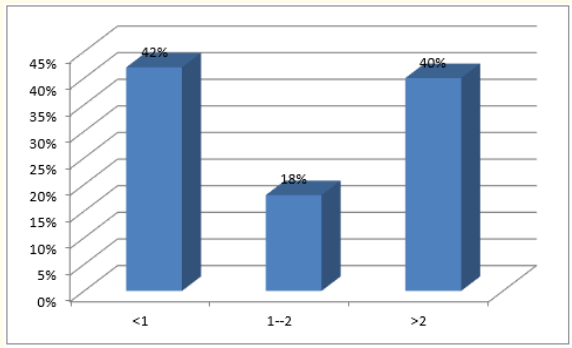
Figure 4: Neutrophils to lymphocytes ratio at discharge.
In this study the total participants were 40 in number. Almost three quarters (70%) of our participants were in age group less than 7 days. Similar to our study Hannes Sallmon., et al. addressed association between Platelet counts before and during pharmacological therapy for Patent Ductus arteriosus and treatment failure in Preterm infants and reported that most of study participants were of age group less than 10 days [7]. The commonest participants (70%) were of low birth weight. Similar to our study MF Ahamed., et al. reported that almost three quarters of their participants were late preterms with low birth weight [8]. Hannes Sallmon., et al. addressed association between Platelet counts before and during pharmacological therapy for P D A and treatment failure in preterm infants and reported that 80% and 86% of their study participants were late preterm and of low birth weight respectively [7].
Almost two thirds (61.4%) of our participants had heart failure and only 19.9% had neonatal sepsis, similar to the study by Gürağaç A., et al. who reported that 53.1% of their participants had heart failure [9]. Less than half (44.2%) of our participants were managed with paracetamol in comparison with Teeranan A., et al. study who addressed the neutrophil lymphocyte ratio and the prognosis of cardiovascular disease. They concluded that 52.7% of their participants were managed with paracetamol [10]. On admission almost two thirds (67.5%) of our studied participants had neutrophils count ≥ 50 and 60% of them had neutrophils count of > 50 at discharge. similar with Teeranan A., et al. study who concluded that dominancy of their participants had high neutrophils count [10]. On admission and on discharge 90% of our participants had lymphocytes count of less than 50. This is similar to the study of Faruk Savluk., et al. who evaluated the association between NLR and good prognosis for CHDs and documented that majority of their participants had low lymphocyte count [11]. 72.5% of our studied participants on admission and 65% of them at discharge had platelets count of less than 150. Sorina R Simon., et al. reported that majority of their participants had reduced platelets count [12].
82% of our participants were discharged in a good condition. The rest discharged against medical advice or referred. Almost third (38%) of our participants had initial neutrophils to lymphocytes ratio of 1 - 2 and 42% had neutrophils to lymphocytes ratio of less than 1 at discharge. M F Ahamed., et al. addressed Predictors of successful closure of Patent Ductus Arteriosus with indomethacin and reported high neutrophils with low lymphocytes among more than three quarters of their participants [8].
Significant statistical association was found between gender and outcome similar with MF Ahamed., et al. Study who addressed Predictors of successful closure of Patent Ductus Arteriosus with indomethacin and reported that females tend to have better outcome [8]. Significant association was found between low platelets count and outcome similar to MF Ahamed., et al. study who addressed predictors of successful closure of Patent Ductus Arteriosus with indomethacin and reported that patients with low platelets count prior to use of medical management tend to have better outcome [8]. Sorina R Simon., et al. study reported that lower platelets count was associated with better outcome [12]. In our study no significant association was reported between neutrophil to lymphocytes ratio and platelets count with outcome. Xu H Sun., et al. claimed in their study that increased post-operative Neutrophils to lymphocytes ratio following cardiac diseases outcomes was associated with longer duration of ICU stay and poor prognosis for CHD in general [13].
In conclusion there was a significant statistical association between gender and outcome where females tend to have better outcome. There was no significant association between neutrophils to lymphocytes ratio and the outcome. The most commonly used treatment was paracetamol, with more than two thirds discharged in a good condition. Majority of preterm neonates with PDA were males with low birth weight.
We recommend early detection of congenital heart diseases so as to provide effective measures directed at reducing the burden of both morbidity and mortality in the country. Also, utility of platelets count as predictor of management outcome.
Copyright: © 2021 Satti Abdelrahim Satti., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.