A Demerdzieva1*, O Lekovska1, N Angelkova1, S Jordanova-Cacanovska1 and N Pop-Jordanova2
1 Acibadem Sistina Hospital, Skopje, North Macedonia
2 Macedonian Academy of Sciences and Arts, Skopje, North Macedonia
*Corresponding Author: A Demerdzieva, Acibadem Sistina Hospital, Skopje, North Macedonia.
Received: April 19, 2021; Published: May 28, 2021
Citation: A Demerdzieva., et al. “Need for Developmental Assessment”. Acta Scientific Paediatrics 4.6 (2021): 68-87.
Introduction: When we start our work as medical professionals the most important was improving and understanding physical growth and nutrition. Today we know that as much important as good knowledge in physical examination is adequate assessment of personality and social development which is crucial for appropriate developmental assessment. In this context early identification of developmental delay is not just responsibility but either obligation of all health care professionals, especially pediatricians.
Aim of the Study: The aim of this study is to analyze developmental monitoring based on parents informations in our hospital in order to find out which percentage of referred children has to be followed further and has to start with early intervention. Our approach to developmental monitoring is: we start the pediatric assessment by taking very careful history of child. Second step is very careful examination in order to find if the child has same kind of organ dysfunction. In second step crucial is neurological examination especially if we know that children with developmental disabilities have very high rate of seizure disorder, structural MRI abnormalities - especially frontal atrophy… Pediatrician has to be aware that observation of the parent-child interaction also, may be an aid in identifying children with delayed development.
Methodology and Sample: The developmental monitoring in 465 children at the age of 12 - 60 months, referred as children with developmental delay according to primary care pediatricians, special educators or family members in the period of 4 years (from January 2016 until the end of 2019) was implemented. The assessment of the evaluated sample is done using CDC developmental milestone checklist (Centers for Disease Control and Prevention) for specific ages -12 and 18 months and 2,3,4 and 5 years. To assess behavioral and emotional problems, physicians need information from family and people who see children in their everyday contexts.
Results: The results were presented for each group separately.
Conclusion: Research indicates that the first five years of a child’s life are critical to brain development, academic achievement and later life outcomes. The right developmental and behavioral assessment can change the trajectory of a child’s life forever.
Keywords: Medical Professionals; Physical Growth; Nutrition; Developmental Monitoring
We are medical workers. Our mission is to increase family knowledge, skills, and participation in health promotion and disease prevention activities. As pediatricians we must promote desired social, developmental and health outcomes of infants, children, and adolescents. One of the most important field of research is child development stimulated by social pressure to improve the lives of children. When we start our work as medical professionals the most important was improving and understanding physical growth and nutrition. Today we know that as much important as good knowledge in physical examination is adequate assessment of personality and social development which is crucial for appropriate developmental assessment. In this context early identification of developmental delay is not just responsibility but either obligation of all health care professionals, especially pediatricians. According to Policy Statement for Identifying Infants and Young Children with Developmental Disorders in the Medical Home: An Algorithm for Developmental Surveillance and Screening from American Academy of Pediatrics developmental surveillance must be incorporated in every well-child preventive care visit [1].
What is developmental delay? According to WHO and ICD-10 classification of mental and behavioral disorders developmental delay is unspecified lack of expected normal physiological development in childhood [2]. Recent studies tell us that as many as 1 in 4 children in the United States, ages 0 to 5, are at moderate or high risk for developmental, behavioral, or social delays [3]. The situation cannot be different in our country. In US young children who live in low income families are even more likely to have a developmental delay [4]. Unfortunately, in our country many families still are with low income. Why is so important to recognize developmental delay? Because it can lead to behavior problems and poor academic achievement [5].
The term developmental impairment or disorder covers a heterogeneous group of conditions that start early in life and present with delay or an abnormal pattern of progression in one or more developmental domain [6]. Pediatricians are always concerned about the reason for developmental impairment. It is true that children develop at different rates, and it is important to distinguish those who are within the “normal” range from those who are following a pathological course. More than twenty years ago we have good evidence that early identification and early intervention improve the outcomes of children with developmental impairments [7,8].
We must define three terms in order to speak about developmental assessment. According to CDC (Center for disease control and Prevention) developmental monitoring observes how child grows and changes over time and whether child meets the typical developmental milestones in playing, learning, speaking, behaving, and moving. Parents, grandparents, early childhood providers, and other caregivers can participate in developmental monitoring. Developmental screening takes a closer look at how child is developing. During screening child will get a brief test, or parent will complete a questionnaire about his/her child. The tools used for developmental and behavioral screening are formal questionnaires or checklists based on research that ask questions about a child’s development, including language, movement, thinking, behavior, and emotions. Developmental screening can be done by a doctor or nurse, but also by other professionals in healthcare, community, or school settings.
The American Academy of Pediatrics recommends developmental and behavioral screening for all children during regular well-child visits at these ages:
At the end we want to define term developmental surveillance. Surveillance is defined as a flexible, longitudinal, and continuous process that includes eliciting and attending to parents› concerns, maintaining a developmental history, making accurate and informed observations, identifying the presence of risk and protective factors, and documenting the progress and findings [9].
Developmental delay can be caused by many reasons. Sometimes is very easy to identify them but in most cases this is very hard work, not always successful. Unfortunately, developmental delay may be reason for later behavior disorders or associated developmental disorders. So, we need appropriate method and approach designed specifically for developmental monitoring of young children by health care providers to identify all possible cases that need further investigation. There are many reports from all over the world which show as that for typically developed children developmental monitoring can provide just reassurance and support parenting competence. But what about the children why have developmental delay? Then developmental monitoring can help us identify the problem early and start with early intervention.
As health professionals we must know that there is an interplay of genetic predispositions (the biology) and early environmental influences (the ecology), which affect later abilities of children to play, learn, work, and be physically, mentally, and emotionally healthy. Which is the group of children with special health care needs? Children with birth defects, inherited syndromes, developmental disabilities, and disorders acquired later in life, that are relatively common and unfortunately this number is constantly increasing.
Developmental monitoring of all children must be continuous process in which health care professionals skillfully observe children, listen to parental concerns, make adequate observations of children, and sharing opinions and concerns with other relevant professionals. Of course, health care professional’s especially pediatricians have to take very precise history and complete physical examination in order to find all possible medical reasons for developmental delay especially those which need early treatment.
Our approach to developmental monitoring incudes: Parents usual came to medical visit with same level of concern for child development - sometimes real according to very specific symptoms and sometimes just because of some family history (other disabled child in family) or concerns of primary care pediatrician. According to American Academy of Pediatrics Developmental concerns should be included as one of several health topics addressed at each pediatric preventive care visit throughout the first 5 years of life [1].
So, we start the pediatric assessment by taking very careful history of child - family history, information’s about pregnancy and delivery, immunizations, vitamin D prophylaxes, past diseases, allergic predispositions, social status of family… Second step is very careful examination in order to find if the child has same kind of organ dysfunction. Special attention must be pointed if child has chronic respiratory or allergic illness, recurrent otitis, head trauma, sleep problems… We pay special attention to growth parameters, head shape and circumference, possible facial or body dysmorphic signs, vascular markings, testicular volume and signs of neurocutaneous disorders. In second step crucial is neurological examination especially if we know that children with developmental disabilities have very high rate of seizure disorder, structural MRI abnormalities - especially frontal atrophy… Neuropsychological correlates include some level of impairment in executive functioning, weak central coherence - problem in integrating information in meaningful wholes, impaired empathy. Further very important is hearing screening especially if child has language delay.
Pediatrician has to be aware that observation of the parentchild interaction also, may be an aid in identifying children with delayed development. Opposite to this strong connection within a loving, supportive family, along with opportunities to interact with other children are protective factors.
The aim of this study is to analyze developmental monitoring based on parents informations in our hospital in order to find out which percentage of referred children has to be followed further and has to start with early intervention. At the end the main aim is to support all children develop in a healthy way and reach their full potential.
The developmental monitoring in 465 children at the age of 12 - 60 months, referred as children with developmental delay according to primary care pediatricians, special educators or family members in the period of 4 years (from January 2016 until the end of 2019) was implemented. All children were divided in 5 groups:
Starting at the time of birth and continuing throughout all childhood, children reach milestones in the way how they play, learn, speak, act, and move. Of course, children development is according to own potential, and it can be difficult to suppose when a child will learn a given skill. However, there is a frame in which one child can rich a special milestone. The assessment of the evaluated sample is done using CDC developmental milestone checklist (Centers for Disease Control and Prevention) for specific ages -12 and 18 months and 2, 3, 4 and 5 years. To assess behavioral and emotional problems, physicians need information from family and people who see children in their everyday contexts. Parents and parentsurrogates are the primary sources of such information for most children. We use information’s from them and check at the same time what are real child’s achievements.
A developmental milestones checklists have questions about a child’s development, including social and emotional development, language and communication, cognitive achievements, movement and physical development. The results of such developmental monitoring helped us planning the best support to development of the child in our care. This kind of monitoring does not provide a diagnosis, but, it indicates whether a child has to be track developmentally and maybe further evaluated.
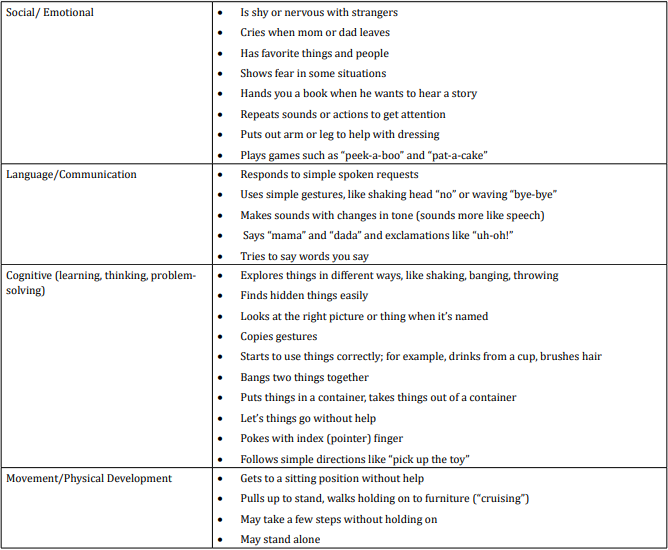
table 1
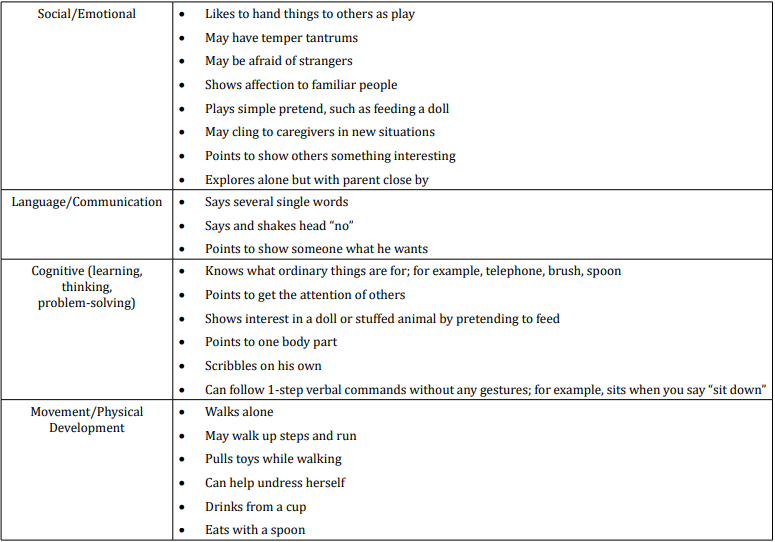
table 2
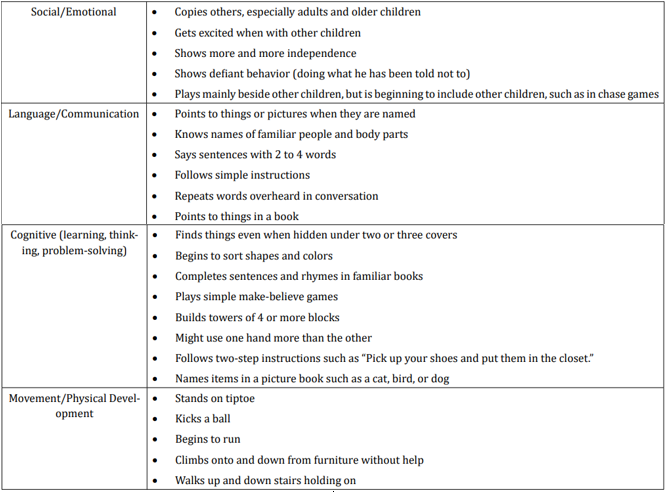
table 3
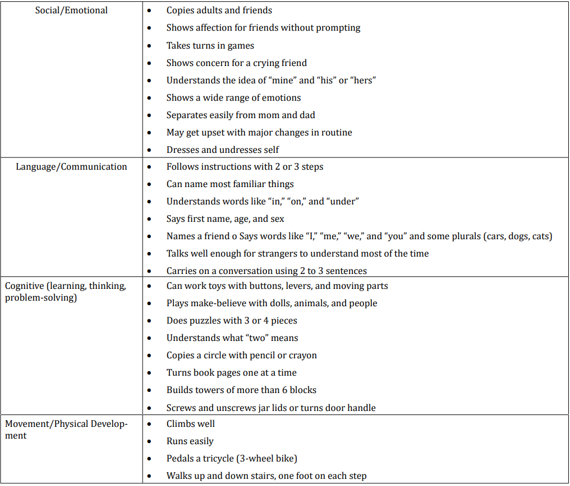
table 4
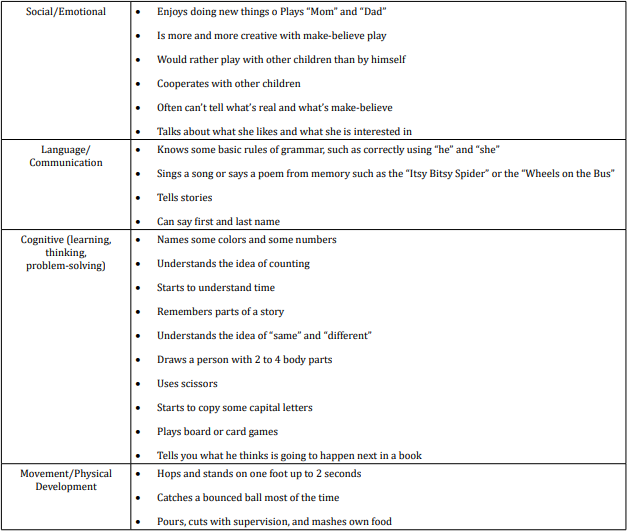
table 5
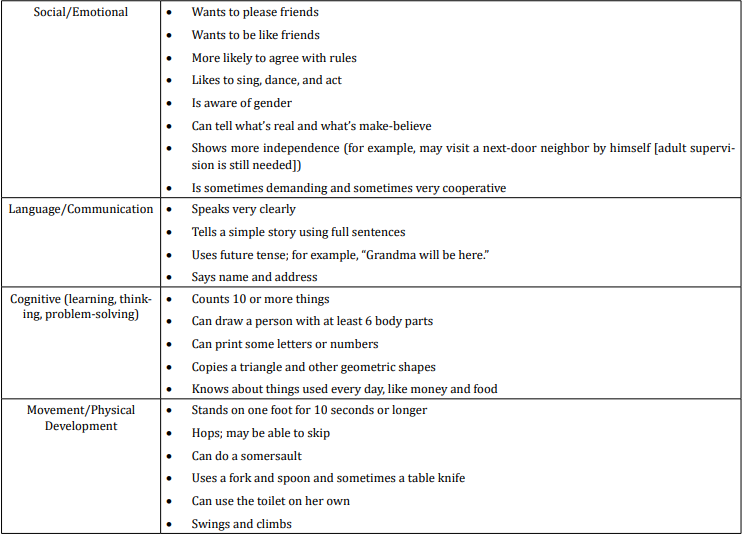
table 6
When we analyzed parent’s answers for milestones in social/ emotional behavior at the end of first year of life we found that all children (or 50 in absolute number): show fear in some situations; put out arm or leg to help with dressing and play games such as peek-a-boo” and “pat-a-cake”. Nearly 80% of children (or 40 in absolute number) at the end of first year cry when mom or dad leaves and have favorite things and people. 60% (or 30 in absolute number) are shy or nervous with strangers; hand us a book when they want to hear a story and repeat sounds or actions to get attention.
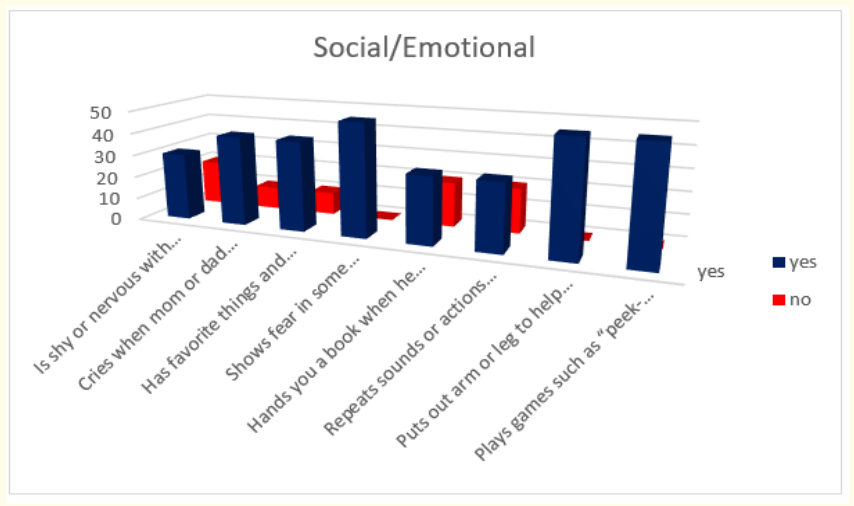
Figure 1: How do parents answer the questions about the milestones that child has reached in social/emotional part of their behavior in first year.
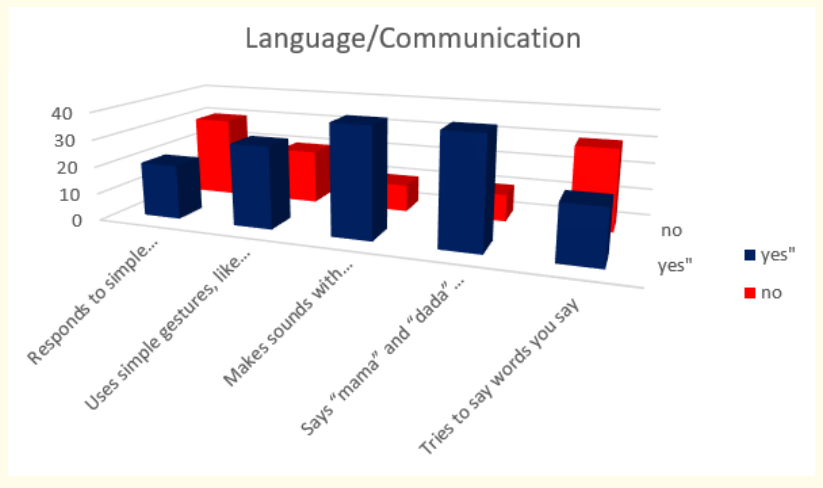
Figure 2: How do parents answer the questions about the milestones that child has reached in language and communication area of behavior in first year.
Answers about language and communication skills show us that 80% (or 40 in absolute number) make sounds with changes in tone (sounds more like speech) and say “mama” and “dada” and exclamations like “uh-oh”!; 60% (or 30 in absolute number) use simple gestures like shaking head for “no” or waving “bye-bye” and 40% of children (or 20 in absolute number) respond to simple spoken requests and try to say words we say.
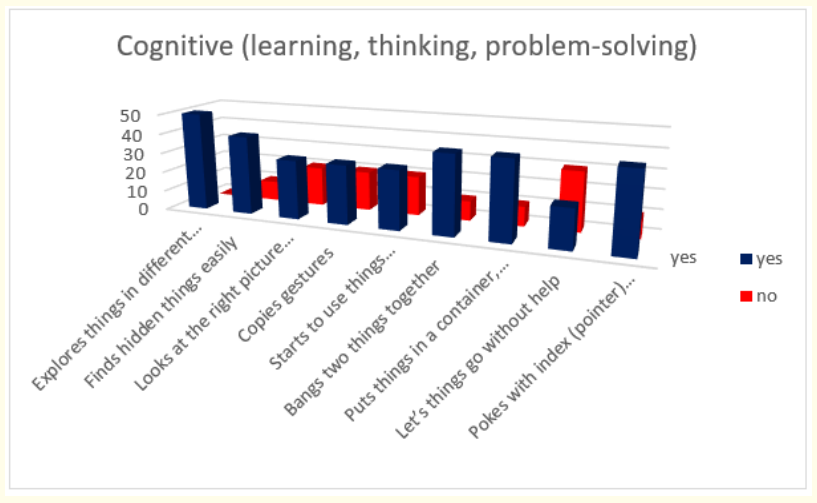
Figure 3: How do parents answer the questions about the milestones that child has reached in cognitive (learning, thinking, problem-solving) area of behavior in first year.
Results about cognitive milestones in first year show us that all children (50 in absolute number) explore things in different ways, like shaking, banging, throwing; 80% (or 40 in absolute number) find hidden things easily; bang two things together; put things in a container and take things out of a container; poke with index (pointer) finger; 60% (or 30 in absolute number) look at the right picture or thing when it’s named; copy gestures; start to use things correctly; for example, drinks from a cup, brushes hair and 40% (or 20 in absolute number) let things go without help.
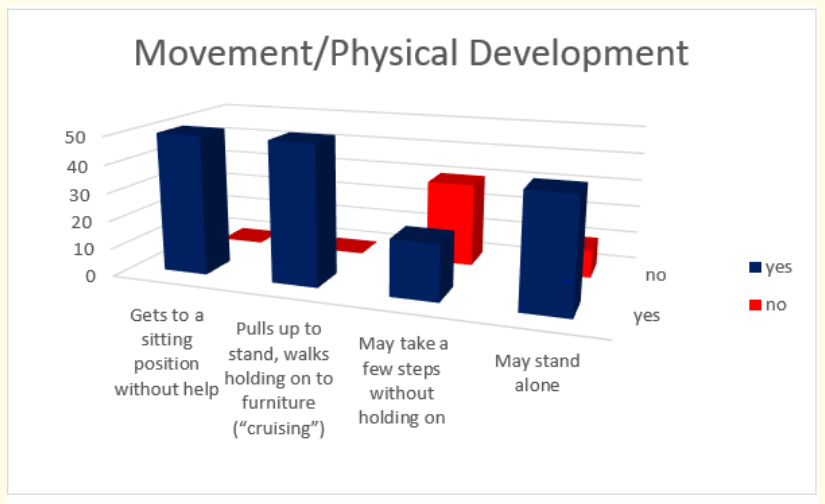
Figure 4: How do parents answer the questions about the milestones that child has reached in movement and physical development during the first year.
Milestones in movement and physical development at the end of first year were presented with these results - all children (50 in absolute number) get to a sitting position without help and pull up to stand and walk holding on to furniture; 80% (or 40 in absolute number) may stand alone and 40% (or 20 in absolute number) make few steps without holding on.
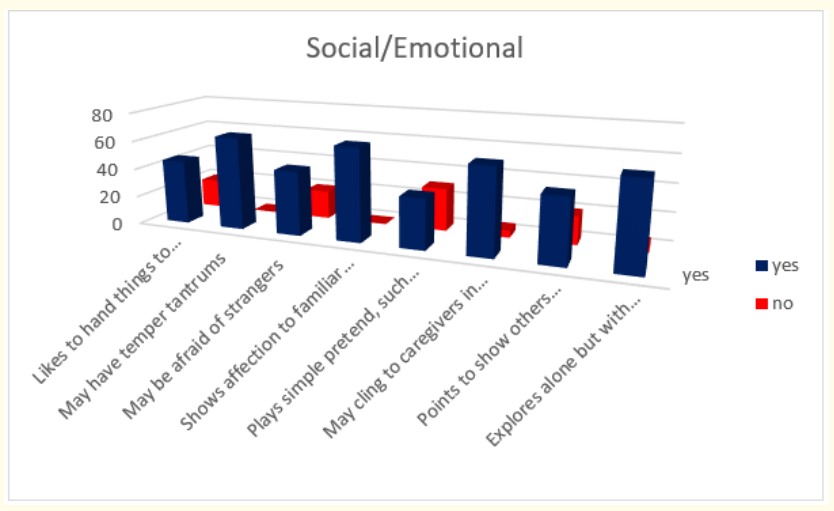
Figure 5: How do parents answer the questions about the milestones that child has reached in social/emotional part of their behavior at the age of 18-th months.
When we analyzed parent’s answers for milestones in social/ emotional behavior at the age of 18-th months of life we found that all of the children (or 65 in absolute number): may have temper tantrums; show affection to familiar people and nearly all (92,3%- or 60 in absolute number) may cling to caregivers in new situations and explore alone but with parent close by. 69,23% of children (or 45 in absolute number) according to their parents like to hand things to others as play, may be afraid of strangers and point to show others something interesting. At the end 53,85% of children (or 35 in absolute number) play simple pretend, such as feeding a doll.
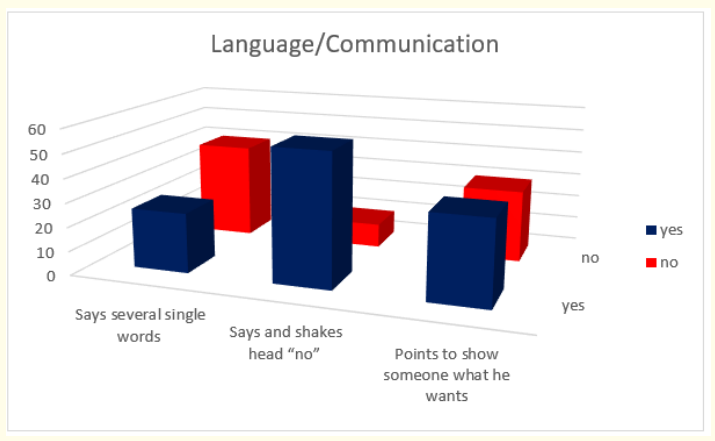
Figure 6: How do parents answer the questions about the milestones that child has reached in language and communication area of behavior at the age of 18-th months.
Answers about language and communication skills show us that 84,61% of children (or 55 in absolute number) say and shakes head for “no”; 53,84% (or 35 in absolute number) point to show someone what they want and only 38,46% (or 25 in absolute number) say several single words.
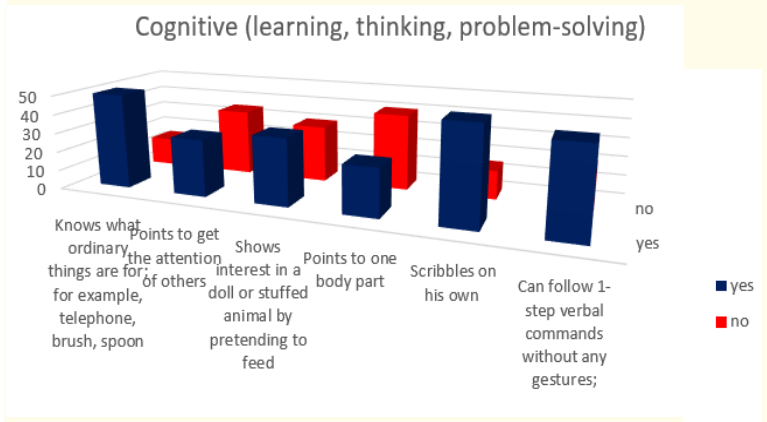
Figure 7: How do parents answer the questions about the milestones that child has reached in cognitive (learning, thinking, problem-solving) area of behavior at the age of 18-th months.
Results about cognitive milestones in first 18 months of life show us that most children - 76,92% (or 50 in absolute number) know what ordinary thing are for; for example, telephone, brush or spoon and scribble on their own; 69,23% (or 45 in absolute number) can follow one step verbal command without gestures; 53,85% (or 35 in absolute number)show interest in a doll or stuffed animal by pretending to feed; 46,15% (or 30 in absolute umber) point to get the attention of others and only 38,46% (or 25 in absolute number) point to one body part.
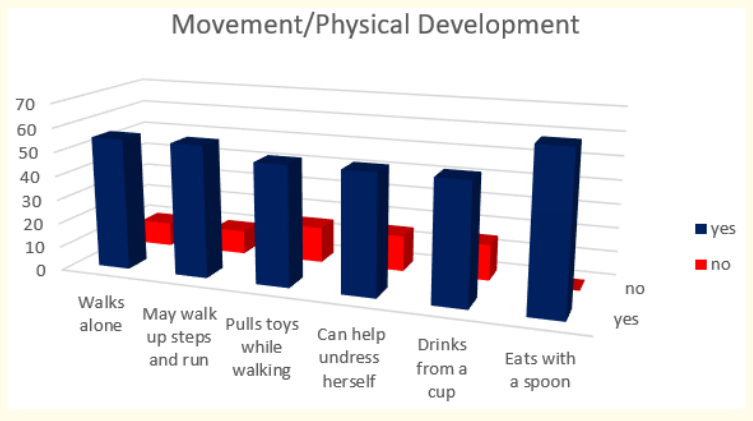
Figure 8: How do parents answer the questions about the milestones that child has reached in movement and physical development at the age of 18-th months.
Milestones in movement and physical development at the end of 18-th month were presented with these results – all children – 100 % (or 65 in absolute number) can eat with a spoon; 84,61% (or 55 in absolute number) walk alone and may walk up steps and run and 76,92 % pull toys while walking and can help undress themselves.
When we analyzed parent’s answers for milestones in social/ emotional behavior during the second year of life we found that all of the children (or 110 in absolute number): show defiant behavior (doing what he has been told not to); 90,90% (or 100 in absolute number) show more and more independence and 81,82% (or 90 in absolute number) copy others, especially adults and older children, get excited when they are with other children and play mainly beside other children.
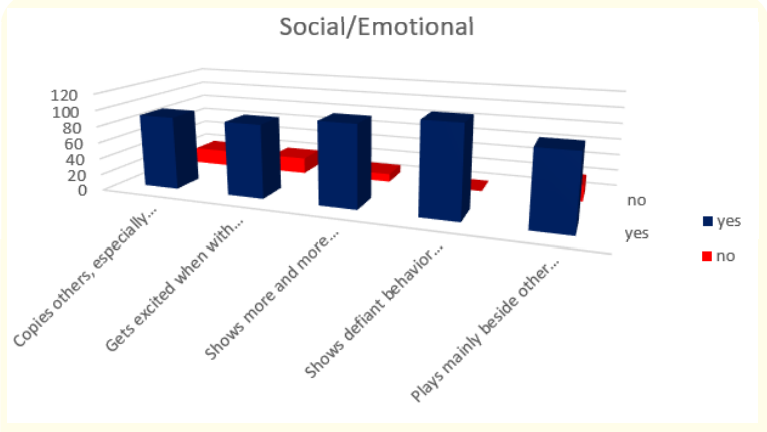
Figure 9: How do parents answer the questions about the milestones that child has reached in social/emotional part of their behavior at the age of 2 years.
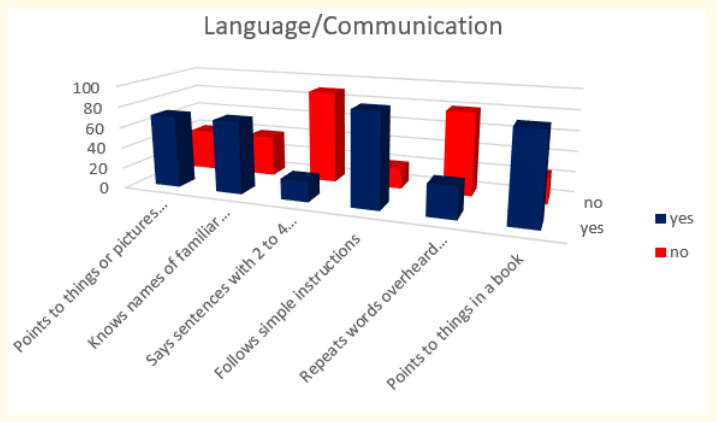
Figure 10: How do parents answer the questions about the milestones that child has reached in language and communication area of behavior at the age 2 years.
Answers about language and communication skills show us that 81,82% of children (or 90 in absolute number) follow simple instructions; 77,27% (or 85 in absolute number) point to things in a book; 63,64% (or 70 in absolute number) point to things or pictures when they are named and know names of familiar people and body parts. Unfortunately, only 27,27% (or 30 in absolute number) repeat words overheard in conversation and 18,18% (or 20 in absolute number) say sentences with 2 to 4 words.
Results about cognitive milestones in second year of life show us that all children (or 110 in absolute number) might use one hand more than the other; 90,90% (or 100 in absolute number) find things even when hidden under two or three covers and build towers of 4 or more blocks; 59,09% (or 65 in absolute number) follow two-step instructions such as “Pick up your shoes and put them in the closet”; 45,45% (or 50 in absolute number) begin to sort shapes and colors and play simple make-believe games; 31,82% (or 35 in absolute number) name items in a picture book such as a cat, bird, or dog and only 9,09% (or 10 in absolute number) complete sentences and rhymes in familiar books.
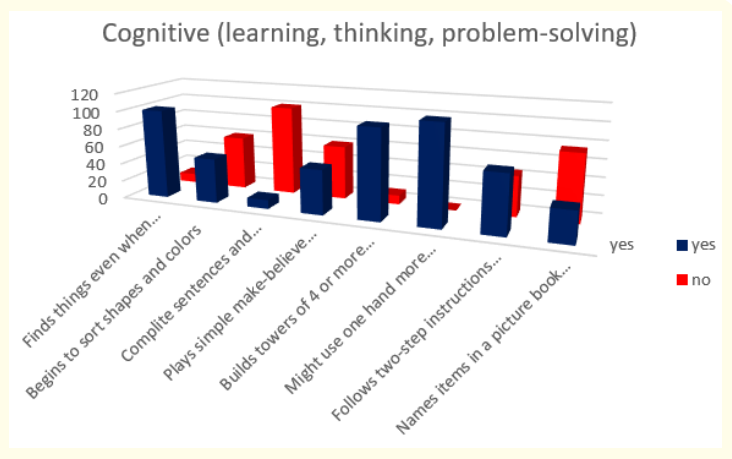
Figure 11: How do parents answer the questions about the milestones that child has reached in cognitive (learning, thinking, problem-solving) area of behavior at the age 2 years.
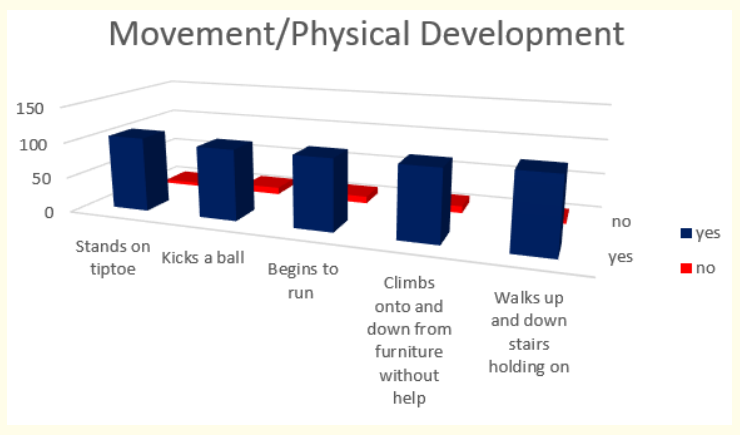
Figure 12: How do parents answer the questions about the milestones that child has reached in movement and physical development at the age of 2 years.
Milestones in movement and physical development at the end of second year were presented with these results - 95,45% (or 105 in absolute number) stand on tiptoe and make or copy straight lines and circles and 90,90% (or 100 in absolute number) kick a ball; begin to run and climb on to and down from furniture without help.
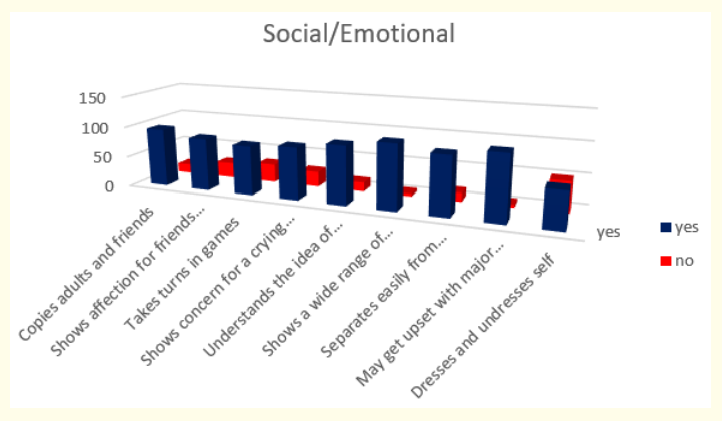
Figure 13: How do parents answer the questions about the milestones that child has reached in social/emotional part of their behavior at the age of 3 years.
When we analyzed parent’s answers for milestones in social / emotional behavior during the third year of life we found that most of the children or 91,30% (or 105 in absolute number) show a wide range of emotions and may get upset with major changes in routine; 82,61% (or 95 in absolute number) copy adults and friends, understand the idea of “mine” and “his” or “hers” and separate easily from mom and dad; 73,91% (or 85 in absolute number) show affection for friends without prompting and show concern for crying friend; 69,56% (or 80 in absolute number) take turns in games and only 52,17% (or 60 in absolute number) dress and undress themselves.
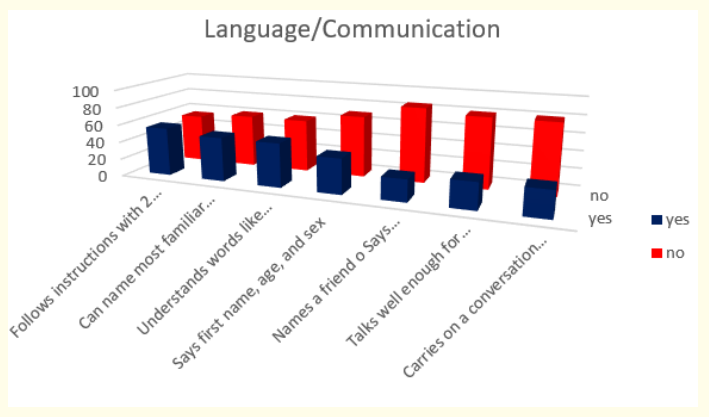
Figure 14: How do parents answer the questions about the milestones that child has reached in language and communication area of behavior at the age 3 years.
Answers about language and communication skills show us that 47,83% (or 55 in absolute number) follow instructions with 2 or 3 steps; 43,48% (or 50 in absolute number) can name most familiar things and understand words like “in,” “on,” and “under”; 34,78% (or 40 in absolute number) say first name, age, and sex; 26,09% (or 30 in absolute number) talk well enough for strangers to understand most of the time and carry on a conversation using 2 to 3 sentences and only 21,73% (or 25 in absolute number) say words like “I,” “me,” “we,” and “you” and some plurals (cars, dogs, cats).
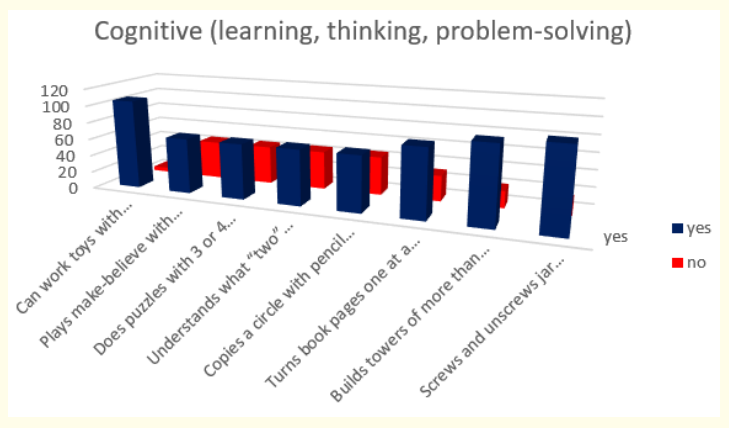
Figure 15: How do parents answer the questions about the milestones that child has reached in cognitive (learning, thinking, problem-solving) area of behavior at the age 3 years.
Results about cognitive milestones in third year of life show us that most of the children or 91,30% (or 105 in absolute number) can work toys with buttons, levers, and moving parts; 82,61% (or 95 in absolute number) screw and unscrew jar lids or turns door handle; 78,26% (or 90 in absolute number) build towers of more than 6 blocks; 69,56% (or 80 in absolute number) turn book pages one at a time and at the end 56,52% (or 65 in absolute number) play make-believe with dolls, animals, and people, do puzzles with 3 or 4 pieces, understand what “two” means and copy a circle with pencil or crayon.
Milestones in movement and physical development at the end of third year were presented with these results - most of the children or 86,95% (or 100 in absolute number) climb well and walk up and down stairs, one foot on each step; 82,61% (or 95 in absolute number) run easily and 73,91% (or 85 in absolute number) pedal a tricycle (3-wheel bike).
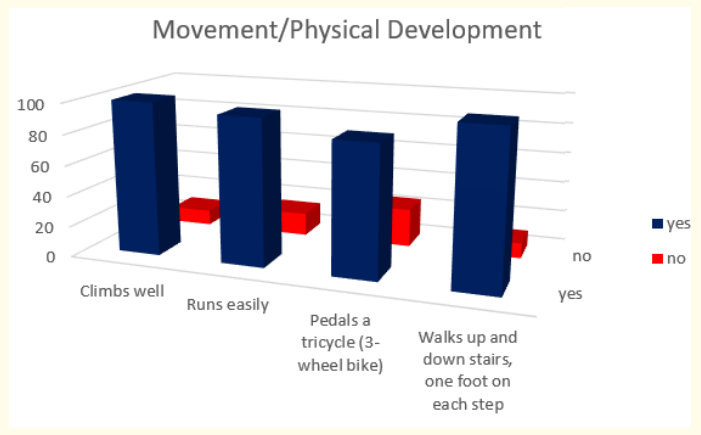
Figure 16: How do parents answer the questions about the milestones that child has reached in movement and physical development at the age of 3 years.
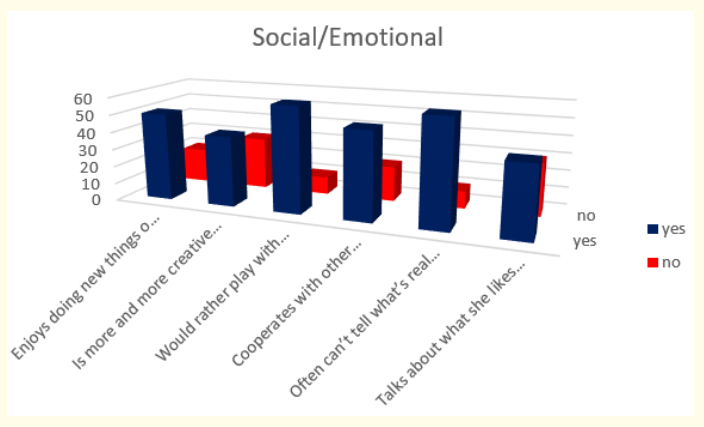
Figure 17: How do parents answer the questions about the milestones that child has reached in social/emotional part of their behavior at the age of 4 years.
When we analyzed parent’s answers for milestones in social /emotional behavior during the fourth year of life we found that most of the children or 85,71% (or 60 in absolute number) would rather play with other children than by themselves and often can’t tell what’s real and what’s make-believe; 71,43% (or 50 in absolute number) enjoy doing new things and cooperate with other children; and at the end 57,14% (or 40 in absolute number) are more and more creative with make-believe play and talk about what they like and what they are interested in.
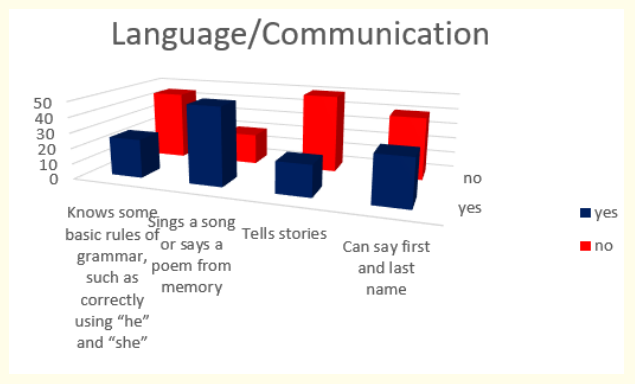
Figure 18: How do parents answer the questions about the milestones that child has reached in language and communication area of behavior at the age 4 years.
Answers about language and communication skills show us that 71,43% (or 50 in absolute number) sing a song or say a poem from memory; 42,86% (or 30 in absolute number) can say first and last name; 35,71% (or 25 in absolute number) know some basic rules of grammar, such as correctly using “he” and “she” and only 28,57% (or 20 in absolute number) tell stories.
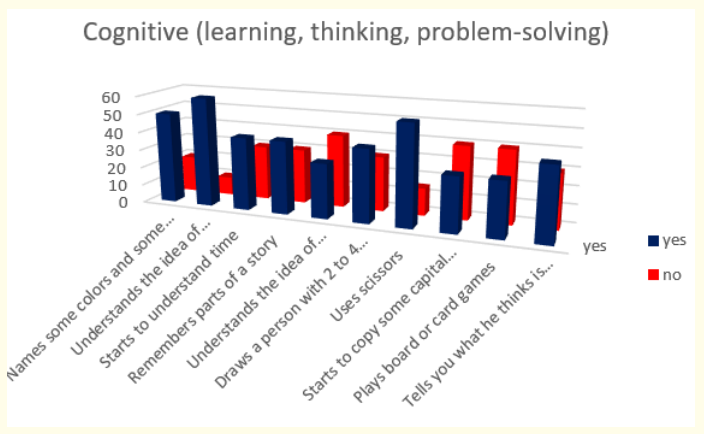
Figure 19: How do parents answer the questions about the milestones that child has reached in cognitive (learning, thinking, problem-solving) area of behavior at the age 4 years.
Results about cognitive milestones in fourth year of life show us that most of the children or 85,71% (or 60 in absolute number) understand the idea of counting; 78,57% (or 55 in absolute number) uses scissors; 71,43% (or 50 in absolute number) name some colors and some numbers; 57,14% (or 40 in absolute number) start to understand time, remember parts of a story, draw a person with 2 to 4 body parts and tell us what they think is going to happen next in a book; and at the end only 42,86% (or 30 in absolute number) understand the idea of “same” and “different”, start to copy some capital letters and play board or card games.
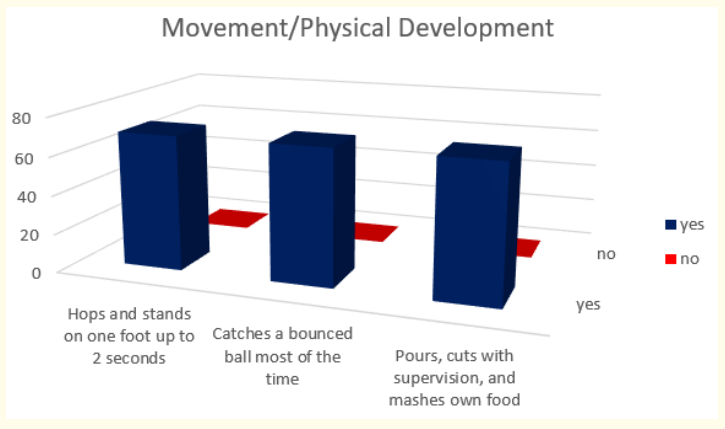
Figure 20: How do parents answer the questions about the milestones that child has reached in movement and physical development at the age of 4 years.
Milestones in movement and physical development at the end of fourth year were presented with these results - all children or 100% (or 70 in absolute number) hop and stand on one foot up to 2 seconds, catch a bounced ball most of the time and pour, cut with supervision, and mash own food.
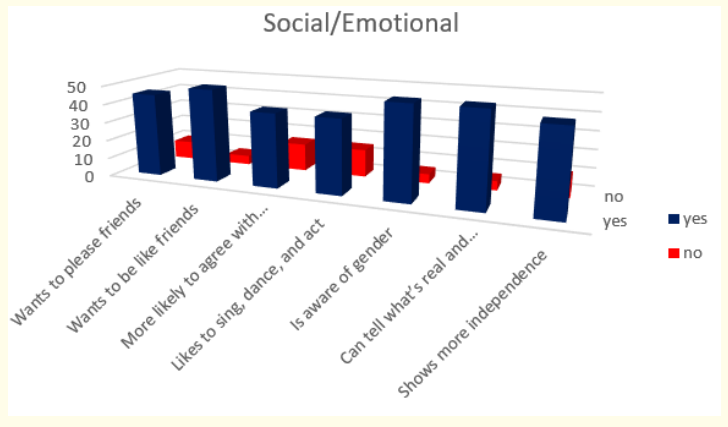
Figure 21: How do parents answer the questions about the milestones that child has reached in social/emotional part of their behavior at the age of 5 years.
When we analyzed parent’s answers for milestones in social / emotional behavior during the fifth year of life we found that most of the children or 90,91% (or 50 in absolute number) want to be like friends, are aware of gender and can tell what’s real and what’s make-believe; 81,82% (or 45 in absolute number) want to please friends and show more independence (for example, may visit a next-door neighbor by themselves (adult supervision is still needed) and 72,73% (or 40 in absolute number) want to be like friends and more likely to agree with rules.
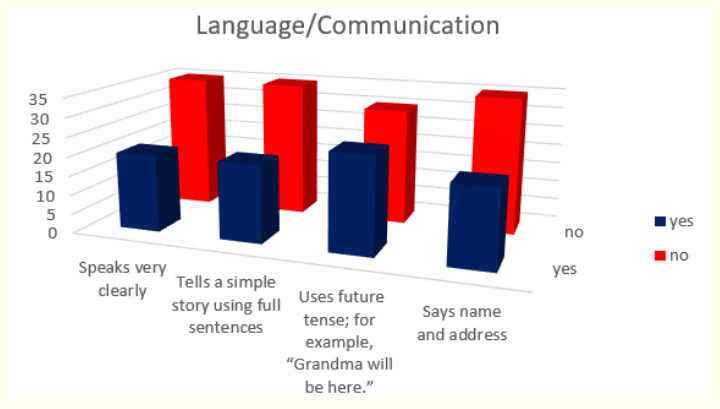
Figure 22: How do parents answer the questions about the milestones that child has reached in language and communication area of behavior at the age 5 years.
Answers about language and communication skills show us that only 45,45% (or 25 in absolute number) use future tense-for example, “Grandma will be here” and only 36,36% (or 20 in absolute number) speak very clearly, tell a simple story using full sentences and say name and address.
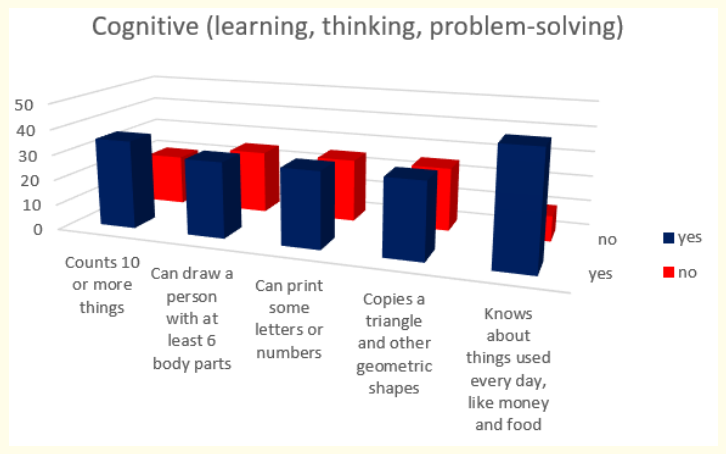
Figure 23: How do parents answer the questions about the milestones that child has reached in cognitive (learning, thinking, problem-solving) area of behavior at the age 5 years.
Results about cognitive milestones in fifth year of life show us that most of the children or 81,82% (or 45 in absolute number) know about things used every day, like money and food; 63,63% (or 35 in absolute number) count 10 or more things and 54,54% (or 30 in absolute number) can draw a person with at least 6 body parts, can print some letters or numbers and copy a triangle and other geometric shapes.
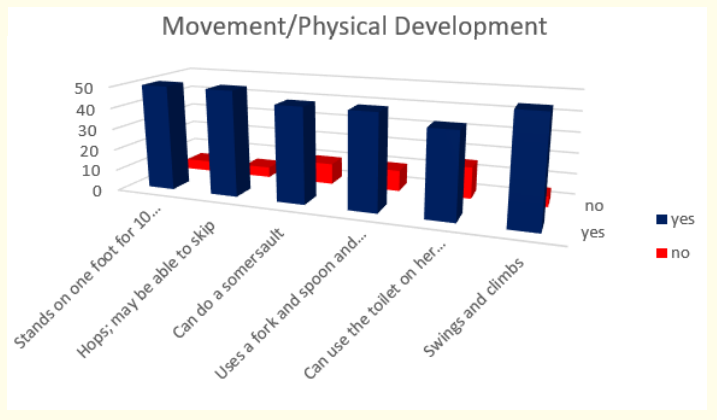
Figure 24: How do parents answer the questions about the milestones that child has reached in movement and physical development at the age of 5 years.
Milestones in movement and physical development at the end of fifth year were presented with these results - 90,91% (or 50 in absolute number) stand on one foot for 10 seconds or longer, may be able to skip and swing and climb; 81,82% (or 45 in absolute number) can do a somersault and use a fork and spoon and sometimes a table knife and 72,73% (or 40 in absolute number) can use the toilet on their own.
We start from the statement that the detection of developmental disorders is an integral component of well-child care. “Developmental delay” is used for the condition in which a child is not developing and achieving skills according to the expected time frame. The term ‘developmental delay’ as it is used in the clinic is a descriptive term, not a diagnosis [10].
We know that asking parents specifically about their child’s behavior can yield valuable information regarding development, because parents do not necessarily differentiate between behavior and development, and developmental delays often manifest through behavior. But we are aware that the absence of parental concern does not preclude the possibility of serious developmental delays [11].
In medical literature there are many studies that have shown substantial variations in the prevalence of developmental delay. A number of methodological issues make it difficult to compare available prevalence rates, such as differences in case definition and criteria, type of measures used, variations in age and whether the studies report on low or high risk populations [12]. Prevalence’s of developmental delay based on the National Health Interview Surveys (NHIS-CH), which is a parent completed questionnaire on development disability, reported that 15% of US children between 3 and 17 years had a developmental disability [4]. The Health Intervention Survey (NHIS-D) on Disabilities reported that 3.4% of all children had general developmental delays and 3.3% had functional developmental delays among American children between 4 and 59 months [13].
Analyzed our results from testing the children at the end of first year show us that most of the children have good achievements in social/emotional behavior. Answers about language and communication skills show us that results were not satisfying for children’s respond to simple spoken requests and the way how they try to say words we say. Results about cognitive milestones and milestones in movement and physical development in first year show us that most of the children reach desired milestones except maybe in making few steps without holding on. From our medical point of view most of the children have good achievements but need to be follow. Anyway as 20% were children that passed NICU we made neurological assessment and all needed investigations.
When we analyzed parent’s answers for milestones in social/ emotional behavior at the age of 18-th months of life we found that most of the children reached expected milestones. Results were unsatisfied for “play simple pretend”, because only half of the children (53,85%) can play simple pretend, such as feeding a doll. We decided to follow this group especially if we know that toddlers with an ASD (autism spectrum disorder) diagnosis showed less pretend play across contexts and less social engagement with parents or the examiner than either low risk toddlers or high risk toddlers without a diagnosis [14]. Answers about language and communication skills show us that 84,61% of children say and shakes head for “no”; 53,84% point to show someone what they want and only 38,46% say several single words. This is very important. We want to quote Finnish authors who wrote “Speech and language development is essential in following up children’s wellbeing. Assessment of active early childhood vocabulary gives information about language development. Parents’ assessment is reliable until about 2 years. Studies show that children aged 1 year 6 months have an average active vocabulary of dozens of words. Though individual variation is wide, most children possess far more than a few words.” So that is the reason why those nearly 40% must be very careful followed.
Results about cognitive milestones in first 18 months of life show us that less than 50% of children (46,15%) point to get the attention of others and only 38,46% point to one body part. We start from the fact that gestures play a crucial role in language development and delays in gesture production may have negative cascading effects on it [15]. This exploratory study examined gesture production in 18-month old infants with different underlying risks for language delay. Findings suggest that a lower rate of pointing at 18-month may be an early common marker of language delay in infants born preterm, especially those with an extremely low gestational age. What about other groups of children? If we know that according to the American Academy of Neurology and Child Neurology Society one of the red flags for autism, which are absolute indications for immediate evaluation is lack of babbling, pointing, or other gesture by 12 months, than this children who did not point to get the attention of others and did not point to one body part at the age of 18-th months, must be further followed very carefully [16]. Milestones in movement and physical development at the end of 18-th month were relatively satisfactory.
When we analyzed parent’s answers for milestones in social/ emotional behavior and movement and physical development during the second year of life we cannot find great disturbances in comparison with normal developed children. But very concerning were results according to language and communication skills and cognitive milestones. Unfortunately, only 27,27% of children could repeat words overheard in conversation and what is even more concerning only 18,18% could say sentences with 2 to 4 words. This is not just problem in our country. The reported prevalence of language delay 20 and more years ago in children two to seven years of age ranges from 2.3 to 19 percent [17-21]. Past decades’ language delay (LD) in young children is a very common problem.
Using the widely accepted criterion of a parent-reported expressive vocabulary of less than 50 words and/or no word combinations, the prevalence of LD is estimated to be approximately 15% at the age of 24 to 29 months [22,23]. We cannot report percentage in whole population or compare our results with other authors works because the observed children were from selected group with some kind of developmental delay. Anyway we must emphasize the importance of further language assessment. Several studies have shown that children with speech and language problems at two and a half to five years of age have increased difficulty reading in the elementary school years [23]. Children in whom speech and language impairments persist past five and a half years of age have an increased incidence of attention and social difficulties [24]. And at the end severe speech and language disorders in young children can negatively affect later educational achievement, even after intensive intervention [25].
Concerning results about cognitive milestones in second year of life are connected again with language development - more than half of analyzed children cannot sort shapes and colors and play simple make-believe games; around 70% cannot name items in a picture book such as a cat, bird, or dog and more than 90% cannot complete sentences and rhymes in familiar books.
Further we analyzed parent’s answers for milestones in social/ emotional behavior during the third year of life and we found that most concerning was the fact that nearly half of the children cannot dress and undress themselves. This fact is in connection with our mentality and the way how we educate our children and their independency from adults. Again answers about language and communication skills show us that more than half of children cannot follow instructions with 2 or 3 steps and cannot name most familiar things and understand words like “in,” “on,” and “under”; more than 65% cannot say first name, age, and sex; more than 70% cannot talk well enough for strangers to understand, cannot carry on a conversation using 2 to 3 sentences and cannot say words like “I,” “me,” “we,” and “you” and some plurals (cars, dogs, cats). All of this is very concerning. Why? Children with isolated expressive language delay have a good prognosis [26-28] but, early language delay can be an indicator for several neuro developmental problems. Language delay can be associated with general cognitive impairment or be an initial symptom of an autism spectrum disorder [29]. Anyway the best is not choosing a “wait and see” strategy, but rather taking early language delay seriously. It was shown that a substantial proportion of children had additional deficits in receptive language abilities, treatable hearing problems, and neurodevelopmental problems [30].
From results about cognitive milestones in third year of life concerning is fact that less than 50% of children cannot play makebelieve with dolls, animals, and people, cannot do puzzles with 3 or 4 pieces, cannot understand what “two” means and cannot copy a circle with pencil or crayon. Again, emphasis must be put on pretended play and connection to autism. Children with autism spectrum disorder (ASD) show deficits in pretend play in early childhood and beyond, but it is unclear how early these deficits can be assessed reliably [31,32]. From aspect of milestones in movement and physical development results are in expected range.
When we analyzed parent’s answers for milestones in social /emotional behavior during the fourth year of life we found that less than 50 percentages of children were less creative with makebelieve play and did not talk about what they like and what they are interested in. Again, the most concerning results were in the group of language and communication skills were little less than 60% could not say first and last name nearly 65% did not know basic rules of grammar, such as correctly using “he” and “she” and more than 70% could not tell stories. What to do in such situation? Children only with speech delay at age 4 years seem more likely to resolve, and this might justify a “watch and wait” approach. In contrast, those with speech disorder at age 4 years appear to be at greater risk for persistent difficulties and could be prioritized for therapy to offset long-term impacts [33]. “Late talkers” is a term used in the scientific field of atypical language development to describe toddlers who exhibit delay in expressive language skills, although they do have intact receptive skills [34]. What about children with developmental language disorder? According Tomas and Vissers, there is continuous interplay between perception, attention, executive functions and language across childhood. This cognitive interplay might underlie problems in communication and social-emotional functioning observed in many children with developmental language delay [35]. In this context are our results about cognitive milestones in our patients in fourth year of life. They show us that more than 40% did not understand time, did not remember parts of a story, did not know how to draw a person with 2 to 4 body parts and to tell us what they think is going to happen next in a book. Unfortunately, more than 50% did not understand the idea of “same” and “different”, could not copy some capital letters and play board or card games. It is known that preterm children from different socioeconomic backgrounds are more likely to have motor, cognitive, and functional development impairment, detectable before school age, than their term peers [36]. What about other children, who were born on time? We were interested about the association between pre-school cognitive ability and later occurrence of mental health-related problems. It is known that sub average cognitive functioning in early life increases later risk of mental health problems. This finding provide new information on a serious and under addressed public health problem among children with sub average cognitive ability who are not considered mentally retarded according to clinical definitions [37]. Other authors assessed the association between preschool cognitive ability and later occurrence of mental health-related problems, including possible variations in profiles of risk factors for emotional and behavioral problems in young adulthood. Such information may be helpful in designing preventive interventions to reduce school- or community-related difficulties among children with lower than average cognitive ability before they enter elementary school [38,39].
Milestones in movement and physical development at the end of fourth year were without deviation from normal.
According to parent’s answers for milestones in social/emotional behavior during the fifth year of life most of the children have good achievements in all asked spheres of action. The worst achievements again were about language and communication skills where more than 50% did not use future tense-for example, “Grandma will be here” and more than 60% did not speak clearly, did not know to tell a simple story using full sentences and did not know to say name and address. Treatment of language impairment is essential and has been assessed by many authors. For example, Catts and colleagues [40] in their study found that children with language impairment in kindergarten were at a high risk for reading disabilities in second and fourth grades. This risk was higher for children with a nonspecific language impairment (nonverbal and language deficits) than for those with a specific language impairment (deficits in language alone). Of course we must be very careful when we analyze just information’s taken from parents because false positive results can be received [41]. Anyway any suspicious for language delay must be very careful assessed and send for further evaluation.
Results about cognitive milestones in fifth year of life show us that most of the children know about things used every day, like money and food; but nearly 40% couldn’t count 10 or more things and over 40% could not draw a person with at least 6 body parts, could not copy some letters, numbers, triangle or other geometric shapes. Of course this kind of cognitive delay is part of global developmental delay and the same like language delay must be further assessed. At the end milestones in movement and physical development at the end of fifth year were presented with good achievements except the fact that more than 25% could not use the toilet on their own. Once more we would like to emphasize that this is according to our mentality and understanding of our mothers who prefer to take care about their children even when they have to be independent.
At the end I would like to quote Christina Bethell and colleagues [42], who wrote “When children are not screened consistently, opportunities for early identification, intervention and treatment may be delayed. Gaps in screening and wide variations across states present considerable opportunities for cross-state learning to improve quality on this critical component of preventive pediatric care. Measurement systems for assessing prevalence and impact of screening require continued evaluation and development”.
First, discussion about healthy development with the child’s family must be done at each well-care visit. This should also occur for a child who comes in for a sick visit or injury and missed the most recent well-care visit according to the practice’s periodicity schedule. Good results on testing at the end of first year are not guarantee for normal development later. So, this must be continuous process.
Second conclusion is that developmental and behavioral screening and support is a team effort. We, always encourage and remind families to communicate with us about their developmental or behavioral concerns, screening results, and inclusion in early intervention programs. With everyone on the same page line, children can get the support they need in every setting.
Third, in some countries children have developmental and behavioral screening passport, similar to an immunization card, which is a tool to help families keep track of their children’s developmental milestones and screening records. After this work our plan is to implement such tool in our hospital to have better results in tracking child development and of course better results in early intervention.
Forth, we think that all parents are just our partners on their child’s developmental journey. To encourage them we usually put accent or name a skill or behavior the child is doing well and note as progress.
Research indicates that the first five years of a child’s life are critical to brain development, academic achievement, and later life outcomes. The right developmental and behavioral assessment can change the trajectory of a child’s life forever.
Copyright: © 2021 A Demerdzieva., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.