Loredana Matei1,2*, Aurel Nechita1,2, Irina Profir1,2, Mihailov Oana Mariana1 and Anisoara Munteanu1
1Faculty of Medicine and Pharmacy, “Dunărea de Jos” University of Galati, Romania
2“Sfântul Ioan” Emergency Clinical Hospital for Children, Galati, Romania
*Corresponding Author: Loredana Matei, Department of Clinical Medical, Faculty of Medicine and Pharmacy, “Dunărea de Jos” University of Galati, Romania.
Received: March 11, 2021; Published: May 07, 2021
Citation: Loredana Matei., et al. “Study on the Antibiotic Resistance of Streptococcus pneumoniae Strains Present in the Paediatric Population”. Acta Scientific Paediatrics 4.6 (2021): 08-12.
Background: Antibiotic resistance is an issue whose characteristics are always dynamic, being by definition a crisis in the medical world. Currently, the studies in the specialized literature confirm the need for comprehensive efforts to minimize the rate of microbial resistance to antibiotic therapy, by studying the emerging microorganisms and the mechanisms of resistance of antimicrobial agents.
Method: Current research aims to analyzed the distribution of the incidence of Streptococcus pneumoniae detected over a year, focusing on the particular characteristics of this pathogen (sensitivity to antibiotics, but also resistance).
Results: For the patients hospitalized during 2019 in “Sfântul Ioan” Emergency Clinical Hospital for Children in Galati, an average total number of 230.42 was detected, which is associated with a standard deviation of ± 55.348 strains. The analysis of bivariate correlations with Pearson index demonstrates by its sig values of <0.05 the existence of statistical significance between the seasonal predisposition of antibiotic sensitivities of Streptococcus pneumoniae strains, but also the correlations between sensitivity - resistance for this pathogen.
Conclusion: One of the most important current issues in the medical world is the increase in resistance of Streptococcus pneumoniae, the pathogen being one of the main causes of development of otitis, pneumonia, meningitis and even septic states. The antibiotic resistance of pneumococcus is increasing worldwide, documented in the case of beta-lactams and macrolides in the first place.
Keywords: Streptococcus pneumoniae; Antibiotic Resistance; Sensitivity
SD: Standard Deviation; CI: Confidence Interval
Streptococcus pneumoniae is a common commensal agent of the upper respiratory tract, whose colonization can lead to local or systemic infections [1].
The information in the specialized literature confirms that in the USA, Streptococcus pneumoniae is the pathogen most often incriminated in the appearance of community-acquired pneumonia, meningitis, but also acute otitis media [2].
The scientific research show that the most commonly used classes of antibiotics are β-lactams and macrolides. The de novo resistance to these antibiotics rarely occurs in a sensitive population. This is in contrast to the predictable occurrence of population subgroups with reduced susceptibility to fluoroquinolones due to spontaneous point mutations [3,4].
This paper is a retrospective study that was conducted in the clinical laboratory of „Sf. Ioan”, Emergency Clinical Hospital for Children in Galati, on a number of 731 strains of Streptococcus pneumoniae isolated from various pathological products collected from patients aged 0 - 18 years. The total period of the study was of 1 year, with the separation of the statistical analysis of the variables monitored during the 12 months. The trained medical staff collected these pathological products under aseptic conditions with sterile materials and instruments, and their transport was carried out quickly under biological protection and ensuring the identity of the samples. For the examination and establishment of the morphotinctorial features of these strains, Gram stained smears were used, subsequently seeding on their culture media, differentiating them according to the type of pathological product collected (nasopharyngeal secretion, laryngeal-tracheal secretion, blood and otic secretions). For nasopharyngeal, larynx-tracheal and otic secretions, the inoculation was performed on blood agar, then the optochin test was performed identifying the suspicious alpha-hemolytic cultures. The blood culture technique was practiced for blood using the BACT/ALERT device. The sown media were incubated at 37°C for 24 - 48 hours under aerobic conditions. The identification of the Streptococcus was performed based on the biochemical characters observed on the special Muller Hinton environment, and the identification of the species was done with the help of the automatic bacteriology analyzer Vitek 2 COMPACT. The determination of the spectrum of sensitivity to antibiotics and chemotherapeutics was performed using the automated VITEK 2 COMPACT system, the method of minimum inhibitory concentration (MIC).
The data obtained from the research of the observation sheets of hospitalized patients during 2019 were entered into the statistical analysis program IBM Statistics V. 24 * SPSS, INC., Chicago, Îl, USA) and Excel 2019, subsequently being filtered and sorted according to different criteria.
Initially, the gross descriptive statistical parameters were calculated for all the variables for which this type of calculation approach was considered potentially useful. These include: the mean value, the standard deviation (SD), the minimum and maximum value for continuous numerical variables, the frequency for categorical values, the median and mode value, the skweness and kurtosis indices. The categorical values were entered in the contingency tables and the non-parametric chi-square test (χ2) was applied. Thus, the comparisons between frequencies were made, by comparing the absolute frequencies recorded to the theoretical ones corresponding to the case in which there was no association.
In order to calculate the central trend and data dispersion, descriptive statistics was used, with the 95% confidence interval (confidence interval, 95% CI), the standard error of the mean, the minimum and maximum value. For continuous data, simple bivariate correlations were analyzed with the calculation of Pearson’s correlation coefficient (r - linear correlation coefficient) and the determination factor (R2). To highlight statistically significant differences between groups or subgroups generated in the study group, the T-student test was used. For each of the existing statistical tests, a level of statistical significance for values of 0.05 was used, the value of the p-index at two ends being calculated.
The descriptive analysis of the analyzed batch will start with the detection of the gross statistical characteristics for each of the variables whose analysis was possible from this point of view. Thus, the descriptive statistic analysis highlights a maximum number of 326 strains of pathogens, defined by an average number of 230.42. As to the distribution of the existing Streptococcus pneumoniae strains in pediatric wards, an average of 10.75 strains is found, which is associated with a standard deviation of ± 6.52 strains. The values of the statistical indices Skewness and Kurtosis present values that define the existence of a homogeneous distribution, with the appearance of a normal Gaussian curve, the maximum peak incidence being around 10, as it can be seen in the analysis of the underlying table (Table 1).
The analysis of the histograms corresponding to all the scalar variables presented above, shows distributions of normal Gaussian curves. However, the following particular features will be noted:
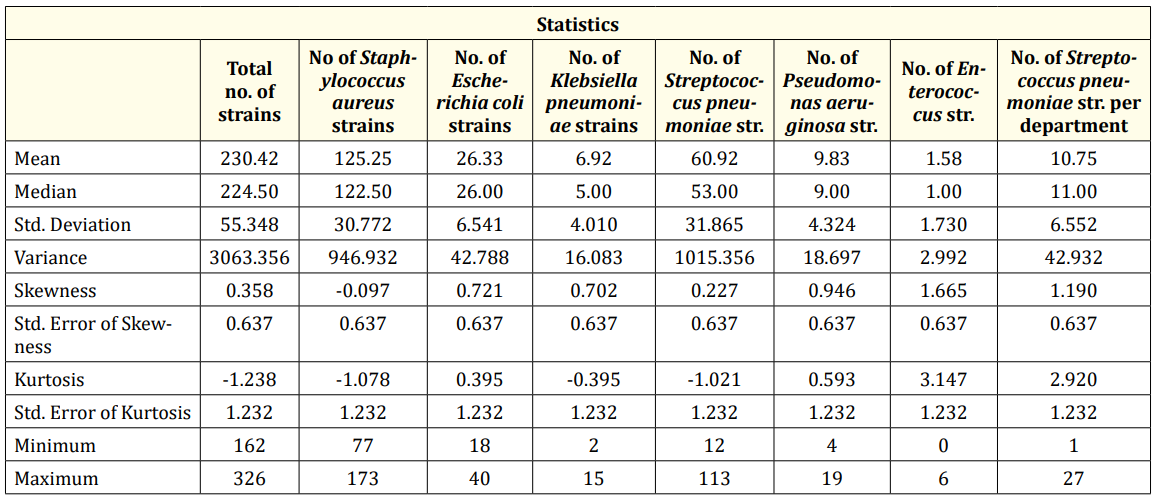
Table 1: Descriptive statistics of scalar variables.
Hereinafter, I will present the distribution of Streptococcus pneumoniae sensitivities. The first three antibiotics were monitored, chosen according to the pathogen’s response to the applied therapy. It will be noted that the first step is Amoxicillin (with a percentage of 33.3%), followed by Cefepim (with a percentage of 25% - corresponding to sensitivity class 2), respectively Ciprofloxacin (25% - for sensitivity class 3), but also three other antibiotics corresponding to a percentage of 16.7% (Norfloxacin, Vancomycin and Linezolid). In terms of resistance to antibiotics, the highest incidence is that of Co-Ttrimoxazole (83.3% as the first antibiotic to avoid), followed by Erythromycin (25% for resistance class 2).
By applying the Pearson bivariate correlation test, the existence of a series of positive and extremely strong correlations can be observed in terms of statistical significance (for reference p index values l ess than 0.01) as follows:

Table 2: Bivariate Pearson correlations.
Antibiotic resistance is in itself a direct consequence of excessive and inappropriate use of antibiotics [5,6].
Increased incidence of antibiotic resistance in patients with pneumococcal infections is detected mainly for macrolides and cephalosporins. This is a real problem of prophylaxis attempts in today’s medical world, along with the existence of bacterial species in multiple classes of antibiotics [7].
The susceptibility of Streptococcus pneumoniae to different classes of antibiotics has a wide range of variation in Europe. For example, the literature confirms, in the case of isolated pneumococcal species, with non-invasive activity, the existence of a variation of penicillin non-susceptibility from 1.7% in Norway to 83% in Romania [8-11].
The present study focused on the statistical analysis of antibiotic resistance in terms of the incidence of different classes (as determined during the 12 months of the study), but also of the specific patterns. The clinical characteristics of the pediatric patients, hospitalized during 2019 were analyzed at the same time.
The obtained data were compared to those existing in the literature. They show the following general resistance to pneumococcal species (from various foci of infection): clindamycin (95.8%), erythromycin (95.2%), tetracycline (93.6%) and last but not least trimethroprim/sulfamethoxazole (66.7%). In the case of the present study, the percentages of antibiotic resistance are the following:
The pediatric infections with Streptococcus pneumoniae are one of the most important issues to monitor in the pediatric world, largely due to the increasing resistance of antibiotic therapies. As a result of the present statistical research, a predominantly increased pneumococcal resistance could be observed in the case of Co-trimoxazole administration (exceeding 90%), with monthly variations. The limitations of the current research are represented primarily by the short period of time during which the analysis was performed (12 months), the study being based on information found in a single clinical laboratory, and not least by the lack of all information regarding the severity of the pathologies, the existence of complications or the evolution of pediatric patients.
As future research perspectives, I mention the attempt to make a centralized analysis on a group of pediatric patients, who were administered (or not) the pneumococcal vaccine, to detect particular characteristics.
No funding was received.
LM and IP performed the literature search for relevant publications on the topic. AN and AM participated in drafting the manuscript and provided critical insight. OMM performed the statistical data analysis. All the authors verified and approved the final version of the manuscript.
The Hospital Ethics Committee approved this study. Each patient, in this case legal guardians, had to fill in an informed consent for each of the sample collection procedures. Subsequent research was carried out under the conditions agreed upon in this informed consent, which was drawn up in accordance with the current legislation of the World Health Organization and the European Union on research on human subjects in the field of medicine, considering the latest version of the Declaration of Human Rights in Helsinki.
The authors declare that they have no competing interests.
Copyright: © 2021 Loredana Matei., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.