Meenakshi Wadhwani1* and Kulbhushan Gangwani2
1 MS Ophthalmology, Assistant Professor, Chacha Nehru Bal Chikitsalya, New Delhi, India
2 Consultant Pediatrician, RB Medical Centre, Delhi, India
*Corresponding Author: Meenakshi Wadhwani, Assistant Professor and Officer in Charge Ophthalmology, Chacha Nehru Bal Chikitsalya, New Delhi, India.
Received: October 15, 2020; Published: February 11, 2021
Citation: Meenakshi Wadhwani and Kulbhushan Gangwani. “Pediatric Ocular Conditions-Guidelines for Treatment during COVID 19 Pandemic”. Acta Scientific Paediatrics 4.3 (2021): 28-30.
Covid-19 caused by SARS COV-2, is associated with neurological and ophthalmological manifestations. It is one the largest global pandemic affecting over 3 million people in 213 countries worldwide. It has led to a death toll of > 200 thousand people in a short period of 4 months as per WHO on May 1st 2020. India has reported over 33,000 cases with > 1000 deaths [1,2].
Keywords: Covid-19; SARS COV-2; Pediatric Ocular Conditions
WHO guidelines recommend in addition to routine standard precautions in the form of personal protective equipment (PPE) that includes gloves, face shield, N 95 mask and PPE dress that all health care workers (HCW) use against possible droplet and physical contact when caring or examining for any patient suspected or confirmed of covid 19 infection. Additional precautions must be taken while doing aerosol generating procedures (AGPS) (Figure 1a-1d).
These AGP’s are defined as procedures that lead to generation of airborne particles specially when a child cries forcefully. This problem becomes all the more important in case of small children who cry and also according to ICMR/WHO children below 2 years are exempted from wearing a mask. So, it becomes all the more important for ophthalmologist.
The disease caused by novel coronavirus (SARS-Severe acute respiratory syndrome) has a high risk of transmission mainly through fomite and aerosols. There is an increased propendence of shedding of virus as an aerosol during coughing, crying in case of children, sneezing thereby settling on the surface. Subsequently, it is transmitted from contaminated hands to mouth, nose and eyes [3,4].
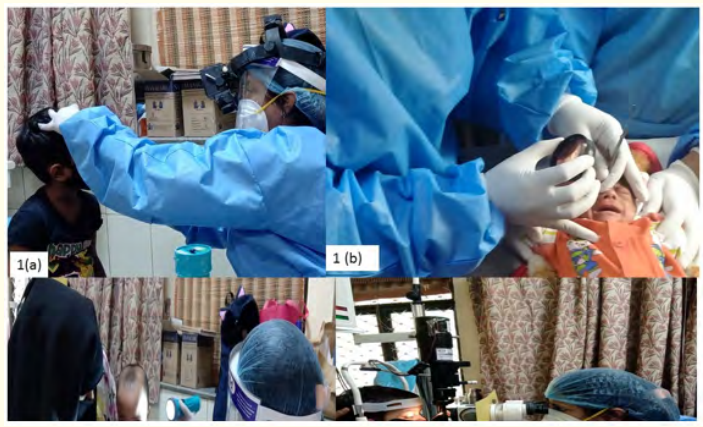
Figure 1: Ophthalmic examination by an ophthalmologist wearing gloves, mask face shield, disposable gown doing. 1a: Indirect ophthalmoscopy in a child. 1b: ROP screening in a preterm baby (aerosol generating is likely as the child is crying. 1c: Torch light examination in a child less than 2 years without mask. 1d: Slit lamp examination in a child with a protective shield in form of Xray film mounted at slit lamp.
SARS COV2 is also detected in the tear secretions by reverse transcriptase PCR reaction in a recent study. Recently a study conducted in china reported the presence of this virus in almost 31.6% of patients with COVID 19 related conjunctivitis tested positive on nasopharyngeal swab [2-4].
Those who have to go close to such babies for doing indirect ophthalmoscopic specially fundus examination in children. The importance of PPE kits becomes important specially in case of conducting ROP screening in NICU where the child is preterm not wearing mask on incubator, eyes can act as a portal of entry through direct aerosol inoculation [5,6].
VUCA-Volatility, uncertainty, complexity and ambiguity of general situations and it fits apt for the world is today is thoroughly affected by COVID 19 pandemic. This can be converted to VUCA2: Incorporating vision, understanding, courage and adaptability which may help us to reach our previously pending vision targets set by WHO and Universal Eye Care 2025 [7].
Personal protective equipment in the form of gloves, surgical cap, N95 mask/surgical/three play masks must be provided to all the health care workers. should be a security barrier at the entry point so that only the patient and one attendant can enter the hospital. Benzalkonium chloride has an inhibitory effect on various viruses including coronavirus. It is a very effective quaternary ammonium compound with cationic amphiphilic property inhibitory against various bacteria and virus. It is an essential constituent in sanitizers and wipes [6,9].
Incidentally, it is commonly used as a preservative in ophthalmic solutions. It’s concentration may vary ranging from 0.01% to 0.04%. It has shown promising results in treatment of adenoviral conjunctivitis even at concentration as low as 0.02%. Hence, use of BAK containing ophthalmic lubricating drops in HCW’s can be used as a safe strategy [8].
Betadine eye drop for conjunctivitis has also shown inhibitory effect on viral effect on viral conjunctivitis. Though, it has side effects like burning and irritation but these can be reduced by diluting 1 ml of 5% Betadine with 4 ml of BAK containing lubricating eye drop [8,9].
This can be done at the hospital gate:
All the patient should be asked about history of fever with dry cough, in case of SARI (Sub acute respiratory tract infection) symptoms they can be referred to the COVID flu corner if available in the hospital. If there is no such facility then patient should be referred to nearby COVID hospital.
In a recent study conducted on impact on patient visit to hospital after opening of lockdown in this pandemic by Das et al it was found that nearly two third of the patients were emergency and one third as routine when classified according to AIOS guidelines as when these patients were triaged, it was found that nearly 6% had visited for allergic conjunctivitis in case of children [11]. So, all these visits could have been postponed if teleophthalmology is promoted amongst the patients attendants. This teleophthalmology is a new revolution in the field of ophthalmology. This can be done through emails, social media, what’s app.
The following measures can be taken while teleophthalmology:

So, with all this a new tiered health care system needs to be revived with minimal risk to the health care personal along with safe treatment of patients. One such way to achieve that goal is by procuring teleophthalmology in the routine ophthalmic practice. With all this association and understanding from ophthalmologist and patient point of view a new normal can be incorporated in the field of ophthalmology [12].
Copyright: © 2021 Meenakshi Wadhwani and Kulbhushan Gangwani. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.