Khaoula Khemakhem1, Leila Cherif1*, Wiem Kammoun1, Mahmoud Ziraoui1, Khadija Baccouche1, Lobna Zouari2, Hela Ayadi1, Imen Hadjkacem1 and Yosr Moalla1
1Department of Child and Adolescent Psychiatry, Hedi Chaker Hospital, Sfax, Tunisia
2Department of Psychiatry C, Hedi Chaker Hospital, Sfax, Tunisia
*Corresponding Author: Leila Chérif, Department of Child and Adolescent Psychiatry, Hedi Chaker Hospital, Sfax, Tunisia.
Received: December 29, 2020; Published: February 11, 2021
Citation: Leila Chérif., et al. “Stress Coping and its Mental Health Status in Tunisian Caregivers of Children with Autism Spectrum Disorders”. Acta Scientific Paediatrics 4.3 (2021): 03-09.
Background and Aims: Identifying coping mechanisms that caregivers adopt as they provide care for individuals with autism holds potential to improve caregiver well-being and promote positive social change. The purpose of this study was to investigate coping strategies in caregivers of children with autism spectrum disorders and to investigate their relationship with mental health variables.
Methods: The study was cross sectional, performed in the department of child and adolescent psychiatry of Sfax. The study included eighty caregivers of children with autism spectrum disorders. Coping strategies were evaluated by the Brief COPE and mental health variables were assessed by the anxiety rating scale of Hamilton, the Hamilton Depression Rating Scale and the short form-36 health survey questionnaire.
Results: More than half of the participants were depressed and anxious. Impaired quality of life was found in 60.7% of participants. The emotion-focused coping was noted in 74% of the sample. Religion, acceptance and positive reframing were the principal coping strategies used. Greater use of emotional support, humour, denial and self-blame were generally found to be significantly linked to depression (p values of 0.007, 0.009, 0.034 and 0.010 respectively). Self-distraction and behavioral disengagement were significantly linked to both anxiety (with p = 0.036 and p = 0.001 respectively) and depression (with p = 0.004 and p = 0.001 respectively).
Conclusion: The findings of this study indicated the effect of both anxiety and depression on the application of coping strategies.
Coping strategies in these caregivers should be increased in order to improve their quality of life.
Keywords: Coping; Autism; Caregivers; Depression; Anxiety
Autism spectrum disorder (ASD) is a complex and serious disorder and can affect many areas of a child’s life. It is characterized by an impairment of social interaction and communication, and by restricted and repetitive behavior [1]. The important role of parents in the child’s development and intervention processes has been pointed out as essential by studies conducted in the last few years [2]. The impact of ASD on the family system likely has a reciprocal negative effect on children with ASD, creating a negative feedback cycle that could ultimately mitigate positive effects of intervention [3]. Caregivers of individuals with autism often report increased levels of stress and a lack of social support to help them cope with various stressors as they provide care [4]. Recent research has highlighted the role of coping strategies as influencing well-being in parents of children with ASD [5]. In fact, coping refers to how individuals respond cognitively and behaviorally to manage a stressful situation and the accompanying emotions [6]. Understanding parents’ coping style may help to get a better knowledge of how they respond to the stresses of raising a child with ASD.
While there is abundant literature on psychosocial variables related to ASD in various parts of the world, the research on coping among caregivers of children with autism spectrum disorder (CASD) remains scarce particularly in the Arabian countries [7]. Jordanian [8], Lebanese [7], Qatari [9], Egyptian and Saudi studies [10] on the subject have been published. Nevertheless, to our knowledge, no study dealing with this subject has been published in the Tunisian population. Yet, understanding these adaption mechanisms is essential to implementing interventions to reduce parents’ psychological stress and to increase the level of parental resilience. Additionally, culture differences can impact results following assessments and clinical decision making. It is therefore important to explore coping strategies in Tunisian CASD, taking into account the cultural and socio-economical specificity of this country.
Tunisia is classified by the World Bank as a “lower middle-income economy” among the emerging economies. In this developing country, the infant mortality rate of children younger than 5 years old is 21‰. More children survive their first few years, and life expectancy is higher than the average for both lower-middleincome and Middle East and North Africa region countries [12,13]. The predominance of youth, 24% of the population is aged under 14 years [13], would mean that there is a high chance of having children with special needs. In Tunisia, the prevalence of ASD is in the order of 35/10000 [14] and the treatment of autism is still limited. The medico-psychological structures of care such as child psychiatry departments and care centers are insufficient. Waiting lists to integrate these structures are long. Integration into these structures is partial for few hours per week. The parent needs to look for care alternatives in the private sector that are expensive. Parents do not receive financial support for the care of their child. Poor parents are the most affected [15]. All this suggests to us that the CASD in Tunisia face many daily social and living challenges and thus are heavily stressed. That being the case, it is crucial to understand how and with what impact CASD deal with this stress. The objective of this study was to evaluate coping strategies and its related mental health variables in CASD.
Parents of all children with ASD (80 children), followed up in the child and adolescent psychiatry department at the Hedi Chaker University Hospital in Sfax were enrolled in the study. Only one parent to each child was included. All participants assisted in the management of their child condition and had enough intellectual level to participate in the study. Thus, the sample consisted of 80 CASD 04 (62 mothers and 18 fathers) who accompanied their children to the child and adolescent psychiatry department, either for consultation or for patient care at the day hospital, during the period from September to December 2014.
All parents were informed about the objectives of the study and the procedures to participate. Informed consent was taken from the parents. The study was conducted through face-to-face interview, undertaken by a single interviewer and following a predetermined format. Data were gathered through self-administered questionnaires including items on child, parents, and family characteristics.
The research was approved by the ethics committee of the medicine University of Sfax.
To assess mental health variables in CASD, the Brief COPE [16], the anxiety rating scale of Hamilton (HAM-A) [17], the Hamilton Depression Rating Scale (HDRS) [18] were used.
Coping strategies of CASD were assessed using the Brief COPE [16]. In its situational format, the Brief COPE uses a 4-point Likert scale (1 = I haven’t been doing this at all to 4 = I’ve been doing this a lot) to query respondents on how frequently they employ 28 different behaviors and cognitions, when coping with a specific stressful situation (in the present study, parenting a child with autism). Following Carver [16], parental responses were initially grouped into 14 theoretically derived subscales consisting of two items each (acceptance, active coping, planning, behavioral disengagement, denial, substance use, humor, positive reframing, religious coping, self-distraction, use of emotional support, use of instrumental support, and venting emotions). In the present investigation, Cronbach’s alpha reliabilities across the 14 subscales averaged 0.72 (range: 0.54–0.93). These reliabilities are similar to those reported in Carver (1997) and indicate acceptable to excellent internal consistency for the abbreviated subscales.
The prevalence of anxiety in parents was evaluated using the anxiety rating scale of Hamilton (HAM-A) [17]. This scale includes 14 items, each defined by a series of symptoms, and measures both psychic and somatic anxiety. Each item is scored on a 5-point scale, ranging from 0=not present to 4=severe, with a total score range of 0-56, where less than 17 indicates mild anxiety, 18-24 mild to moderate anxiety and 25-30 moderate to severe anxiety.
The prevalence of depression was also assessed based on the Hamilton Depression Rating Scale [18]. The first 17 items of the Hamilton Depression Rating Scale were used as part of the psychiatric interview. The HDRS is clinician rated and consists of depressive symptoms which are recorded using 5 or 3-point scales reflecting presence and severity over the past week. Scoring is based on the 17-item scale and scores of 0–7 are considered as being normal, 8–17 suggest mild depression, 18–25 moderate depression and scores over 26 are indicative of severe depression; the maximum score being 52.
The quality of life (QOL) was screened by the Tunisian validated version of the short-form 36 (SF-36). The SF-36 health survey questionnaire [19] is a 36-item Likert-type scale measuring physical functioning, role physical function (problems with work or daily activities as a result of physical health), bodily pain, general health perception which together comprise the physical component summary score. The scale also measures mental health, role emotional function (problems with work or daily activities because of emotional function), energy, and social functioning, which together comprise the mental component summary score. The SF-36 questionnaires were scored for each domain; possible scores range from 0 to 100, with higher scores indicating better HRQOL. The normative scores have a mean of 50 and standard deviation of 10, which is representative of the mean and standard deviation of the findings in the general US population.
All assessments were arabized but not validated in Tunisian population. Only the SF-36 was validated.
Data entry and statistical analysis were performed using the SPSS software in its 19th version. For the descriptive study, the qualitative variables were expressed as a percentage, while the quantitative variables were expressed as averages with their standard deviations.
Comparisons of 2 means were made using Student’s t-test. Comparisons of several means were made using the Anova test. Percent comparisons were made by the Pearson chi-square test (χ²). In all statistical tests, the significance levelwas set at 0.05.
The study included 80 parents who have at least one child diagnosed with ASD. The sample showed predominance of mothers compared to fathers (62 versus 18). At the time of the study, the mean age of mothers was 35 years 8 months (± 6.13) and the mean age of fathers was 42 years 4 months (± 6.14). Among parents, 68.8% of mothers and 56.3% of fathers had a secondary/university educational level. Consanguinity was noted in 26.3%. Only 10% of parents had more than three children while 90% had three or less than three children.
Our sample of children showed that the age average at the first consultation is almost 3 years (range 1.50-8.30 with SD = 1.05). From time of symptom onset to first health care contact, children had an average wait of almost 10 months (range 1-48 months with SD = 8.26). At the announcement of diagnosis, the average age of children was 3.54 years (range 2-8.25 years with SD=1.05). Finally, the average wait time for medical care was 7.50 months (range 1-24 months with SD = 4.26). Children in this sample received institutional care in 88.8% of cases, medication management in 37.5% of cases and speech therapy in 47.5% of cases.
According to the Brief-Cope, the most used coping strategies were: religion (87%), positive reframing (85%), acceptance (82%) and instrumental support (82%).
The least used coping strategies were substance use (13%), humor (38%) and behavioral disengagement (46%) (see Figure 2). The student t-test demonstrated that coping was correlated to depression, anxiety and QOL (see table 1). There was no significant association between Coping and any socio-demographic factor.
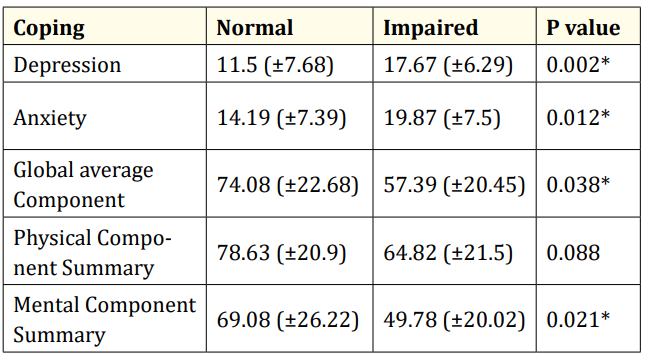
Table 1: Correlations between Anxiety, Depression, QOL and Coping. *Significant; QOL: Quality of Life.
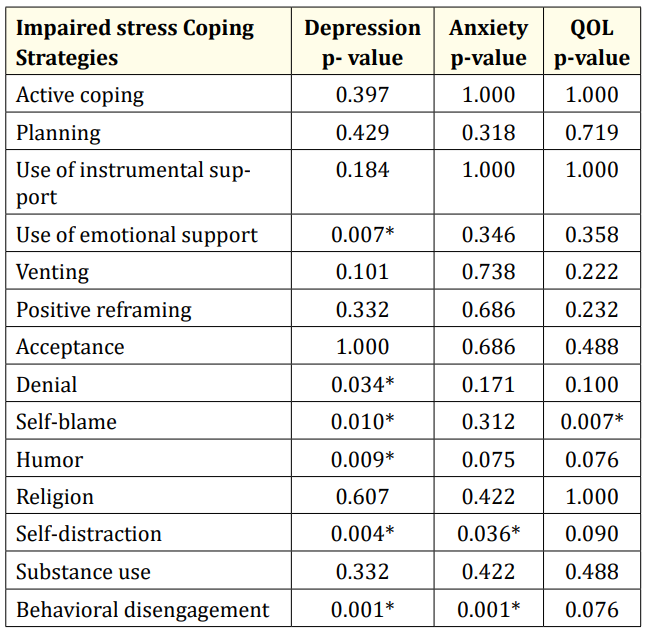
Table 2: Correlations between Anxiety, Depression, QOL and the Stress Coping Strategies. *Significant, QOL quality of life.
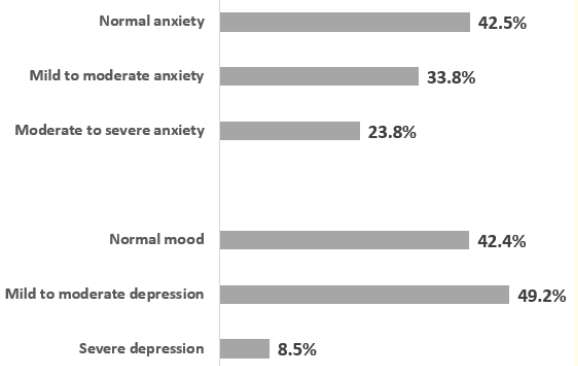
Figure 1: The evaluation of depressive and anxiety symptoms and their severity among parents.
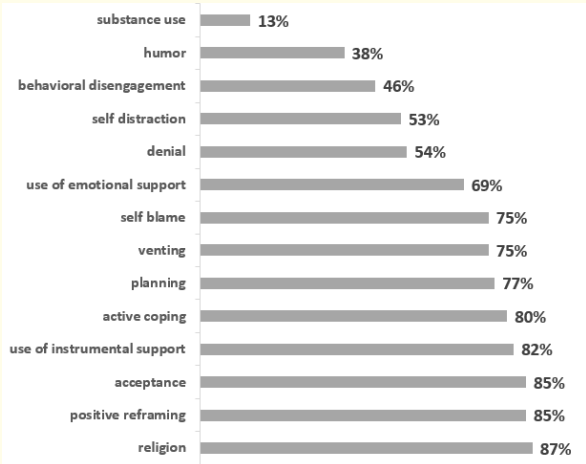
Figure 2: Distribution of CASD according to the use of stress coping strategies.
Figure 1 shows the prevalence of anxiety and depression according to level of severity.
In our study population, impaired QOL was found in 60.7% of parents. The mean of global score was 63.41 (±17.2). The mean of Physical Component Summary (PCS) scores was 67.41 (± 19.96) and the mean mental summary scores (MCS) was 51.02 (± 21.04).
Understanding the ways of the family’s coping with ASD is very important, as this is central to cognitive models of stress. In fact, coping is often applied to families of children with disabilities [20]. Thus, the aim of the present study was to determine the coping strategies and its associated factors in a sample of 80 CASD (62 mothers and 18 fathers) at the Hedi Chaker Hospital, in Sfax.
In our study, the emotion-focused coping were noted in 74% of the sample, which is consistent with what exists in the literature [20]. Religion, acceptance and positive reframing did help a great number of CASD of this study. Prior studies have indicated that acceptance and positive reframing can promote mental health among parents of children with autism and with other disabilities [21,22]. In fact, Islamic culture, like in Tunisia, emphasizes virtues of endurance, resilience and acceptance of poor health, just like good health and good fortune, as both of them are the will of God and are intended to test one’s faith and belief according to Islamic culture. This is similar to other results found in Islamic countries [9,23].
Around half of the sample used behavioral disengagement. In our country, where the economic situation has become increasingly critical and fragile, parents of CASD children may feel constantly worried about the future of their children, therefore, they have to look for ways to help them. Moreover, these parents may be desperate when their children do not evolve as quickly as other normal children [20,24] which may increase their behavioural disengagement. Finally, as problem-solving endurance decreases and care giving issues continue, parents may adopt inappropriate emotion-focused coping such as avoidance of care challenges and stressful feelings [20,25]. In addition, the use of behavioral disengagement can be reinforced by the Eastern ideology of “saving the face”, whereby parents avoid seeking help from others for fear of social stigma and embarrassment associated with children with special needs [20].
The present study also examined the impact of different coping strategies on CASD depressed mood, anxiety, and QOL. Greater use of emotional support, humour, denial and self-blame were generally found to be linked to depression. These findings are largely consistent with the findings of Hastings., et al. [26] and Smith., et al. [27] who stated that depression is a factor associated to ineffective coping, more than anxiety and impaired QOL. In fact, a tendency to experience negative emotions such as depression substantially decreases the ability to cope with the burden of caring for a child with a disability such as ASD [28]. Besides, behaviour disengagement and self-distraction were found to be significantly related to both depression and anxiety. These findings are in line with prior research claiming that caregivers high in neuroticism tended to use more passive-avoidance coping [28]. This result points, like other study findings, the need for interventions which assist parents in better managing feelings of depression and anxiety which are often associated with parenting a child with autism [29]. On another hand, the present study showed that self-blame could negatively affect the CASD’s QOL. As was evidenced by Dardas., et al. [30], parents who accept their responsibilities for the problems they face due to having a child with ASD have a greater sense of control and a better QOL than parents who dwell on the past or blame their selves. Taken together, these findings highlight the need for an assessment of parental stress while at the same time recognizing that many families show an important willingness in coping with the diagnosis of ASD children. Overall, we believe that, in order to improve QOL of CASD, coping strategies in CASD should be increased. Paying attention to this point in taking care of ASD, can help increase QOL of family.
The main limitation of the study is the small sample size. However, it included all parents of all children with ASD followed up in the child and adolescent psychiatry department. It would be relevant to extend the sample to other Tunisian cities and regions to enlarge the sample size. Another limitation is that the used instruments were translated in Arabic but not yet validated in Tunisian population, except the SF-36.
The current study has contributed to the understanding of CASD adaptation by giving a much clear focus on their different coping strategies. It also emphasized the need to develop coping strategies to manage anxiety and depression and to improve the quality of life in CASD.
These findings should help health policy-makers provide better and more support not only to the children with autism, but also to their families. It is necessary to develop early health care strategies that target and support those who are in direct daily contact with a child with autism. Early familiar support with assistance to parents aims at decreasing the overload, improving the family’s health and coping processes.
We thank all parents who participated in this study.
Authors declare no conflict of interest.
Copyright: © 2021 Leila Chérif., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.