Helena Maria Dias Xavier1, Gabriel Lopes Vieira da Silva1 and Denise Von Dolinger de Brito Röder2*
1 Nursing Students at the Federal University of Uberlândia Medical School, Brazil
2
Professor at the Institute of Biomedical Sciences at the Federal University of
Uberlândia, Brazil
*Corresponding Author: Denise Von Dolinger de Brito Röder, Professor at the Institute of Biomedical Sciences at the Federal University of Uberlândia, Brazil.
Received: October 09, 2020; Published: January 28, 2021
Citation: Denise Von Dolinger de Brito Röder., et al. “Hands of Health Care Professionals as a Vehicle for the Transmission of Hospital Pathogens”. Acta Scientific Paediatrics 4.2 (2021): 41-46.
Health Care Related Infections associated with the hands of health professionals has shown high rates of morbidity and mortality as a public health problem. The objective was to synthesize information about the hands of health professionals as a vehicle for the contamination of microorganisms that affect HAIs in hospitalized patients, highlighting risk factors, which etiological agents, analysis of low knowledge and adherence, in addition to analyzing improvement strategies. Articles with the descriptors were searched: Hand Hygiene; Hand Sanitizers; Health Care Associated Infections; Healthcare Workers; Infectious Disease Transmission, Professional-to- -Patient., In the databases and virtual libraries: Scielo, Google scholar, Pubmed, Science direct, Web of Science and Brazilian database Periódico Capes, in the last 5 years. In total, 11,939 articles were found, after exclusion criteria 26 were used to compose the review. Among the relevant risk factors are sepsis, pneumonia, gastrointestinal and urinary tract infections, as well as surgical site infections associated with the hands of professionals. Low knowledge and lack of adherence are related to high workload associated with inadequate resource facilities and training strategies and ineffective hand hygiene assessment. The etiologic agents most frequently detected were Staphylococcus aureus, Staphylococcus coagulase-negative, Staphylococcus epidermidis, Enterococcus spp, Acinetobacter baumannii and Klebsiella spp. Practices such as encouraging the training of professionals responsible for the prevention and control of HAIs in hospitals, surveillance with physical and electronic feedback on the correct execution of hand hygiene, has proven to be effective strategies.
Keywords: Hand Hygiene; Hand Sanitizers; Health Care Associated Infections; Healthcare Workers; Infectious Disease Transmission; Professional-to-Patient
IRAS: Health Care Related Infections; ESBL: Extended-spectrum β-lactamases; GNC: Gram-negatives Resistant to Carbapenemase; MDRGN- Multi-Drug-resistant Gram-negative Microorganisms; MRSA: Methicillin-resistant Staphylococcus aureus; MSSA: Methicillin-sensitive Staphylococcus aureus; VRE: Vancomycin-resistant Enterococcus; DeCS: Health Sciences Descriptors; MeSH: Medical Subject Headings; CoNS: Coagulase Negative Staphylococcus; HCW: Healthcare Workers; HH: Hand Hygiene; ICU: Intensive Care Units
Health Care Related Infections (HAIs) are a public health problem, as the most affected by it are critical patients who have a hospital stay longer than seven days and using invasive devices. In developing countries the occurrence of nosocomial infection is between 5.7% and 19.1% and in developed countries the value is between 3.5% and 12% [1]. Several microorganisms can be found in the hands including: Acinetobacter baumannii (1.4% - 16.5%), Staphylococcus aureus (5.9% - 8.1%), Staphylococcus epidermidis (20.9% - 18.7%) and Enterococcus spp. (1% - 1.3%) [2]. Therefore, the hands of health professionals are one of the main routes of transmission of microorganisms and, for this, hand hygiene is a fundamental measure in the prevention and control for the reduction of HAI [3].
Hospital pathogens through various mechanisms, including the production of biofilm, can remain in the hands and be spread horizontally. This cross-transmission can occur in five ways: from patient to health professionals, patient to environment, health professionals to patient, environment to patient and from environment to health professionals. The most recurrent is contamination of bacteria for hospitalized patients through inanimate objects or direct contact. Thus, the simplest form is through the hands of health professionals as a vehicle that transmits bacteria associated with the environment of the patient and the professional team, and may even cause outbreaks of multi-resistant microorganisms [4]. Pathogenicity and response mechanisms to HAIs will vary with the type of microorganisms, whether they are part of the normal microbiota or whether they are virulent. In addition, it also depends on the maturity or immune responsive state of the patient’s body. In this perspective, critical patients in Intensive Care Units (ICUs) or immunosuppressed can develop HAIs even from non-pathogenic microorganisms [5].
Knowing that the hands of health professionals has been a vehicle for the propagation of microorganisms, it is concerned about the knowledge of the hospital team in the clinical importance of hand hygiene [6]. The importance of knowing the moments of hand hygiene is highlighted, including: before touching or contacting a patient, performing a clean or aseptic procedure, after a risk of exposure to body fluids and removing gloves, contact with a patient and his immediate surroundings and after touching an inanimate object in the immediate vicinity of the patient, even if there is no direct contact with the patient.
In addition, it is also important to choose which antiseptic will be used, the hygiene procedure, how to dry your hands. In this sense, it is indicated for hands that are visibly dirty or not rubbing with water and soap, antiseptics, such as alcohol-based disinfectants, foams or gels or surgical antisepsis [7]. In addition, the environment composed of inanimate objects shared by the hospital team, such as a mouse, keyboard, medical records, among others, are sources of contamination of microorganisms in the hands. Cleaning measures associated with hand hygiene concurrently when investing in surfaces with anti-adhesive properties, with antimicrobial substances incorporated or modified with biological active metals, have been effective ways to avoid HAI [8,9].
The scientific literature, the World Health Organization’s have been made available Hand Hygiene Guidelines, which includes practices such as: creation of a hand hygiene training course; reinforce hand hygiene practices in team meetings; visual reminders and ensuring delivery [10]. In this sense, several multimodal studies point to tools through a scientific structure for implementing hand hygiene quality, which analyze hand contamination based on the logistics of organized and systematic methods in search of gaps in order to propose effective evidence-based protocols , even in low resource conditions [11].
This review aims to analyze the probable hospital pathogens that contaminate the hands of health professionals, addressing the causes and consequences of this contamination and the forms of prevention and control.
Articles with descriptors extracted from DeCS (Health Sciences Descriptors) and MeSH (Medical Subject Headings) were searched: Hand Hygiene; Hand Sanitizers; Health Care Associated Infections; Healthcare Workers; Infectious Disease Transmission, Professional-to-Patient; in the databases and virtual libraries: Scielo, Google scholar, Medline/Pubmed, Science direct, Web of Science and Brazilian database Periódico Capes, in the period from 2016 to 2020. In total, 11,939 articles were found and after exclusion criteria 26 articles were used to compose the review.
In the research, the following inclusion criteria were used: (I) multicentric research, (II) research involving epidemiological surveillance; (III) case reports and (IV) clinical trials (V) publications in Portuguese, English and Spanish. Nevertheless, there were criteria for exclusion of articles for the following reasons: (I) lack of access to the full content of the published article, (II) results described in an incomprehensible or incorrect manner, (III) articles of clinical irrelevance in humans.
Vikke., et al. (2019) [12], in a prospective multicenter observational study from December 2016 to May 2017, shows that the patient during his hospitalization is exposed to a variety of microorganisms and the spread of infection in a hospital environment is due to of three factors: a source of infecting microorganism, a susceptible host and the environment. The hands of health professionals are a potent disseminator of pathogens during patient care, as transmission can occur during direct contact during care or through indirect contact when contaminated surfaces are present. According to Zhang., et al. (2018) [13], in an observational study in 2016 shows the significant causes of HAIs in a hospital environment are: prolonged stays, increased use of antimicrobials, resistance to medications and high treatment costs, which also leads to increased morbidity and mortality in these patients. Therefore, for infection control, it requires adherence to hand hygiene and cleaning of surfaces before contact with the patient. However, a factor that directly interferes with proper hand hygiene is the high workload, as this action is considered to be significantly effective and efficient in reducing the occurrence of HAIs, since the contaminated hands of health professionals are the most relevant source transmission of pathogens.
The hands of professionals, as well as other objects and surfaces that they come into contact with, have been studied with the objective of showing the hands as a vehicle for the contamination of several virulent microorganisms, including multidrug-resistant bacteria that are found in the hands of health professionals (Table 1). In this context, Presterl., et al. (2019) [14], demonstrate that several multi-resistant microorganisms are transmitted directly by the hands of professionals and indirectly through contact with secretions, feces, wounds and contaminated objects containing the pathogens. Having clinical relevance, as it has high mortality rates involving sepsis, pneumonia, infections of the gastrointestinal and urinary tract, as well as surgical site infections, associated with microorganisms that include extended-spectrum β-lactamases, Gram-negative bacteria resistant to Carbapenemase, multi-resistant Gram-negative bacteria, methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE).
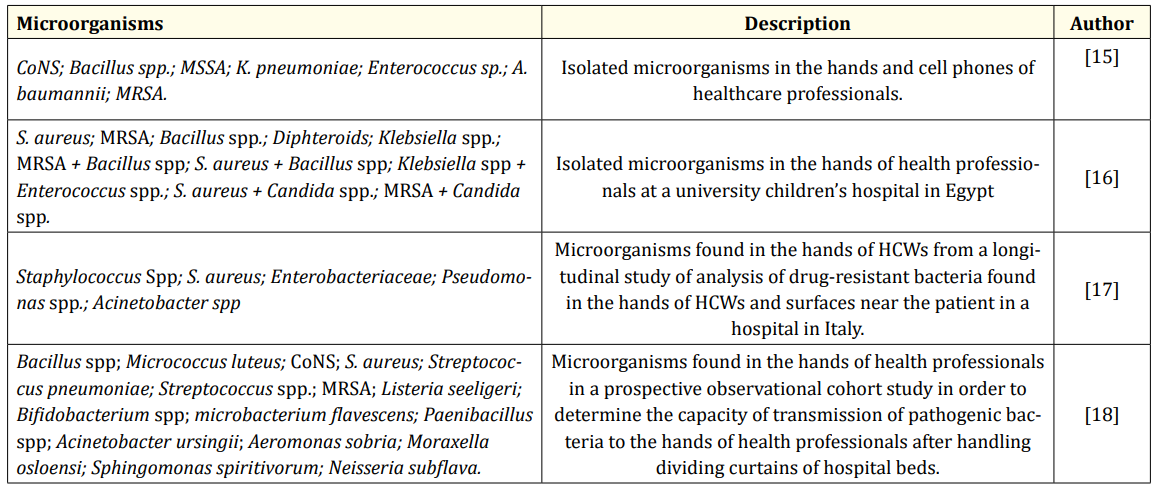
Table 1: Microorganisms found in the hands of health professionals. Methicillin sensitive S. aureus (MSSA); Methicillin-resistant Staphylococcus aureus (MRSA); Coagulase negative Staphylococcus (CoNS); healthcare workers (HCWs).
Qasmi., et al. (2018) [19], in a multicenter study with the participation of 450 medical students in Pakistan, applied a wide quiz and among the characteristics analyzed were basic demographic information, such as age, sex and year of study, knowledge about hand hygiene instructions and procedures, perceptions of the importance attributed to the performance of hygiene by other health professionals, to practices and interventions designed to improve adherence to hygiene. These data were crossed with information from the 434 questions answered in a 95% confidence interval after statistical analysis. It was found that knowledge of hand hygiene and its adherence are low among medical students in the study, however, with emphasis on that women presented hygiene practices superior to men and students from public universities demonstrated superior knowledge in relation to private and semi-private, suggesting as the most important intervention the need for protocols to raise awareness of the importance of hand hygiene and the creation of policies and guidelines to encourage hand hygiene in hospitals.
Knowing that knowledge and low adherence to hand hygiene has been common among students and health professionals, and in the perspective of intervention of this problem, Santosaningsih collaborators (2017) [20] in a randomized controlled clinical trial in 2014 with the participation of 902 tertiary-level hospital beds in Indonesia and 284 health professionals. The study was composed of three phases: (I) pre-intervention; (II) intervention; (III) post-intervention; constituting three different educational programs in the interventions, through active presentations; formation of models; combination of active presentations and model training; in four departments drawn at random. These data were crossed with the 2,766 visualized hand hygiene opportunities and the perception of knowledge assessed among 196 participants in the pre-intervention and 88 in the post-intervention. It was observed that after the intervention there was a significant increase in knowledge and practice in the departments of pediatrics, internal medicine and obstetrics-gynecology, highlighting the importance and effectiveness of implementing educational programs to improve the knowledge and adherence of HH, even when resources are limited.
In addition to encouraging proposals for interventions to improve knowledge of MH, there are several reasons that reduce the adherence to this practice. In this sense, Sadule-Rios and Aguilera [21] in an exploratory and descriptive study with the participation of 452 ICU beds and 42 critical care nurses from a magneto hospital. A questionnaire was answered by the professionals and the questions investigated were reasons for the low HH adherence and suggestions for improvement to increase this adherence in the ICU. These data were crossed with the responses of 25 participants of possible reasons for the professionals’ lack of adherence and 32 responses of suggestions to improve their adherence to the ICU. It was found that despite being aware of the clinical importance of hygiene in the prevention of HAIs, the lack of adherence to the ICU persists due to the high workload associated with the difficulty of accessing hand hygiene resources, and there were suggestions that include designating a team to encourage, assess adherence and the resources made available to HM, create routine meetings to discuss this information, modify the locations of gel alcohol distribution near the bed, in addition to making pocket gel alcohol available for personal use, invest in hand hygiene guidelines and campaigns for healthcare professionals, patients and family members.
Woodard., et al. [22], in an observational study in 2016 with the participation of 750 ICU beds from a tertiary care hospital in the United States. In a first phase, a survey of the knowledge and adherence of HM by health professionals was carried out through an electronic questionnaire, the second step consisted of observing the fulfillment of the 5 WHO moments, and in the last step, it assessed the classification of professionals by prioritizing most important moments of HM among the 5 moments. These data were cross-checked with the responses of 218 health professionals from the electronic questionnaire applied, and 322 opportunities to view HH adherence based on the 5 moments in the 104 bed visits. It was observed that the professionals recognize the importance of MH and have knowledge of how and which moments to perform the MH, however the fulfillment of the 5 moments was low and few professionals remember the moments for not being familiar with this practice, in addition to classifying it as a moment most important of MH before aseptic procedures and as less important after contact with the areas close to the patient.
Moghnieh., et al. [23] in a prospective comparative study between 2015 and 2016 with the participation of 200 university hospital beds in Lebanon and 89 nurses. Participants had an introductory lecture on the 5 moments of hand hygiene, later divided into three groups: (I) control group, (II) incentive-oriented group, (III) feedback-oriented group. These data were crossed with the 9,345 opportunities seen in MH in the 21 weeks analyzed. It was observed that group I did not show significant changes in relation to (II) and (II), in which the group oriented by incentives had a rapid change, however when the incentives were interrupted, this HH adherence according to the 5 moments have been reduced. The feedback-oriented group, on the other hand, had a gradual growth over the 21 weeks and remained stable, showing to be an effective intervention. In this sense, Tartari., et al. [24], in a multicenter study carried out between 2016 and 2018 with the participation of 305 health professionals from 20 countries. A capacitive course based on the World Health Organization (WHO) Multimodal Hand Hygiene Improvement Strategy and the 5 hand hygiene moments, was applied to infection prevention and control professionals in order to expand knowledge and among activities were didactic lectures, simulation-based training and experiential participatory activities. These data were cross-checked with the 297 responses in a pre- and post-test form for the course, assessing the participants’ development and course satisfaction. It was observed that there was an improvement in the knowledge and adherence of the volunteers, indicating that the training program has a large-scale viability of preparing infection prevention and control professionals at local and national levels, especially in countries where hygiene knowledge and adherence of the hands are low or nonexistent.
Reilly., et al. [25] in a randomized controlled trial study with the participation of 120 health professionals from the United Kingdom. The participants were divided into two groups: those who performed (I) the 3-step technique and those who (II) the 6-step hand hygiene technique, and among the characteristics analyzed were comparing the microbiological effectiveness of the hand hygiene technique and the reduction of bacterial contamination of the hands of health professionals. It was observed that even using the same quantity distributed among the participants, the 6-step technique proved to be superior in relation to the 3-step technique in reducing the residual bacterial load, unrelated to the coverage and reach of hand areas, but because of the association with a longer execution time due to the number of maneuvers, demonstrating a better microbiological efficacy against microorganisms. Both hand hygiene techniques and maneuver time are essential factors in reducing the risk of cross-transmission between healthcare professionals and patients, however the method used to dry hands has an influence on this process, putting re-contamination at risk after hand hygiene if not done properly. Mutters and S.L (2019) [26] in a comparative study with the participation of 80 health professionals from a university hospital in Germany. He divided the volunteers into two groups, those who performed hand drying with paper towels after hand washing with soap and water, and those who performed hand drying using a jet air dryer and among the characteristics analyzed were comparing the effectiveness of drying between the two methods in order to remove transient bacterial contamination and evaluate the effect of the resident flora on the hands of the volunteers. It was found that the amount of the bacterial load was reduced with the correct drying technique, especially with the use of the jet air dryer, sheltering fewer viable bacteria to be transmitted to the touch.
In the case of the hands of health professionals, the etiologic agents of medical and hospital importance were Staphylococcus aureus, Staphylococcus coagulase-negative, Staphylococcus epidermidis, Enterococcus spp, Acinetobacter baumannii and Klebsiella spp., Including multi-resistant microorganisms to antimicrobials. The biggest problems related to low adherence to hand hygiene and the most important factor of low knowledge and adherence is high workload associated with a lack of inadequate facilities and ineffective hand hygiene training and assessment strategies. There are practices that prove to be effective for the control of HAIs associated with hand hygiene such as encouraging the training of professionals responsible for the prevention and control of HAIs in hospitals, surveillance with physical and electronic feedback on the correct execution of hand hygiene.
To the National Council for Scientific and Technological Development (CNPq).
None.
Copyright: © 2021 Denise Von Dolinger de Brito Röder., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.