Md. Mostafijur Rahman1,a, Saimon Miah1,a, Sonia Tamanna1, Md. Bayejid Hosen1, Tasnin Akter1, TH Johra2, Yearul Kabir1 and M Zakir Hossain Howlader1*
1 Laboratory of Nutrition and Health Research, Department of Biochemistry and
Molecular Biology, University of Dhaka, Dhaka, Bangladesh
2 Consultant, Department of Obstetrics and Gynecology, Islami Bank Hospital, Dhaka,
Bangladesh
aAuthors contributed equally in this study
*Corresponding Author: M Zakir Hossain Howlader, Professor, Department of Biochemistry and Molecular Biology, University of Dhaka, Dhaka, Bangladesh.
Received: October 29, 2020; Published: November 27, 2020
Citation: Md. Mostafijur Rahman and Saimon Miah., et al. “Association of Maternal Vitamin D with Neonatal Vitamin D Status and Birth Weight in Urban Population of Bangladesh: A Cross Sectional Study”. Acta Scientific Paediatrics 3.12 (2020):19-26.
Background: Vitamin D deficiency during pregnancy leads to poor neonatal development which has serious consequences during the later part of life. The aim of the study was to evaluate maternal and umbilical cord blood 25[OH] D concentrations and their association with birth weight.
Methods: Pre-delivery maternal venous blood within a week before delivery and paired matched neonatal cord blood samples were collected from 75 pregnant women. Serum 25[OH] D was measured by high-performance liquid chromatography. Serum calcium, phosphorus, and alkaline phosphatase activity were measured by colorimetric methods.
Results: Mean maternal serum 25[OH] D was 46.45 ± 5.02 ng/ml, and cord blood 25[OH] D was 21.89 ± 2.27 ng/ml. The serum 25[OH] D level of the mothers and the neonates were significantly associated (P < 0.01) with a linear correlation coefficient of r = 0.49. The mean birth weight of neonates was 2.83 kg ± 0.38 and 22% of the neonates had low birth weight (LBW) (2.33 ± 0.17). Average birth weight of normal babies was 2.97 ± 0.30. The mean maternal 25[OH] D level of mothers with normal birth weight babies (n = 58; 77.33%) was significantly higher (50.41 ± 5.00 ng/mL) than that (28.24 ± 6.87 ng/mL) of mothers with LBW babies (p < 0.0001). There was a high degree of positive correlation between maternal 25[OH] D status with neonate’s birth weight (r = 0.593, p < 0.01).
Conclusion: The results obtained in this study show that there is significant correlation between maternal vitamin D with neonatal birth weight in a cross-sectional urban population of Bangladesh.
Keywords: Serum 25[OH] D; Pregnancy; Cord Blood; Low Birth Weight
Vitamin D is a fat soluble secosteroid formed mostly in human skin by exposure to sunlight, with a small fraction coming directly from the diet [1,2]. Either endogenous or from dietary sources, both are transported in the liver, where their first hydroxylation at the carbon in position 25 takes place, producing 25-hydroxyvitamin D (25[OH]D) [3]. 25[OH]D is the major circulating form of vitamin D, and its concentration in serum reflects the vitamin D stores in humans. Vitamin D deficiency is a worldwide health problem that affects not only musculoskeletal health but also it may be associated with a wide range of acute and chronic diseases. A recent study reported the association of vitamin D deficiency with the risk of type 2 diabetes mellitus in Bangladeshi population [4]. Adequate vitamin D status is the key parameter for proper bone health in early life and reduced risk for developing osteoporosis later. It also prevents secondary hyperparathyroidism. Vitamin D is one of the most important contributors to calcium (Ca) homeostasis [5].
Vitamin D deficiency during pregnancy is not only a danger for maternal skeletal preservation [6] but also may be associated with an increased risk of preeclampsia [7], insulin resistance and gestational diabetes mellitus [8]. Throughout pregnancy, a woman needs to maintain her vitamin D necessities to support her own and her fetus [9]. Vitamin D status during pregnancy is vital to maternal health, fetal development, and optimal neonatal outcomes [10]. Numerous observational studies indicate an epidemic of vitamin D deficiency in pregnant women in different countries [11, 12]. Studies have shown that vitamin D-deficient mothers develop secondary hyperparathyroidism, which leads to transitory hypoparathyroidism and hypocalcemia among the neonates [13]. During pregnancy, adequate vitamin D guarantees proper maternal responses to the calcium demands of the fetus and neonate as neonatal vitamin D stores are entirely dependent on the mothers [9]. Many clinical studies support that severe maternal vitamin D deficiency causes hypocalcemia and congenital rickets in infants. Also, there is [14] evidence to support an association between the prenatal vitamin D environment and the risk of later schizophrenia development [15]. Grant and his colleagues have reported that maternal vitamin D deficiency is a risk factor for infantile autism disease [16]. Mothers with low vitamin D intake during pregnancy, children are found to be more common suffering eczema, hay fever or allergic rhinitis [17].
Adequate maternal calcium and vitamin D intake are associated with appropriate birth weight [5]. In Asian populations living in England, half of the children having low hemoglobin level are suffering from vitamin D deficiency [18]. Lower serum 25-hydroxyvitamin D [25(OH)D] concentrations during pregnancy are associated with poor health outcomes for pregnant women and newborns [19]. Pregnant women and newborns are recognized as populations at increased risk of poor vitamin D status [20]. Given the potential for poor vitamin D status during pregnancy to affect maternal and child outcomes that remain important determinants of global health, our objective was to determine the status of Bangladeshi pregnant women and their newborns to join the global summary of vitamin D status in pregnant women and newborns.
The aim of this study was to evaluate maternal and umbilical cord blood vitamin D concentrations and its association with birth weight.
Dhaka, the capital city of Bangladesh (23°42′0″N 90°22′30″E) experiences a hot, wet and humid tropical climate. The city has a distinct monsoonal season, with an annual average temperature of 25°C (77°F) and monthly means varying between 18°C (64°F) in January and 29°C (84°F) in August. Although the winter season in Bangladesh is not significantly cold but to avoid the seasonal effect on serum 25OH [D] concentration, samples were collected from April to October 2016. Pre-delivery maternal venous blood within a week before delivery and paired matched neonatal cord blood samples were collected from 75 pregnant women with no history of chronic diseases before pregnancy. Samples were collected from Islami Bank Hospital, Dhaka and Azimpur Maternity Clinic, Dhaka. Pregnant women with multiple gestation, gestational diabetes and complicated pregnancy were excluded from the study. All participants were explained about the nature of the study, and informed consent was obtained. They completed a structured questionnaire covering information on age, height, weight, education, dressing style, occupation, and frequency of child. No specific nutritional data was taken. But from verbal communication it’s seen that nearly all patients take 9 cup of cooked rice, 3 cups of vegetable, and approximately 60 gram of protein every day. No subject reported any history of allergy or smoking. This study was approved by the ethical review committee of faculty of Biological Sciences, University of Dhaka.
Maternal venous blood and cord blood samples were collected; centrifuged and appropriate aliquots of serum were taken in Eppendorf tubes and stored at -20°C. Serum vitamin D was measured using High-Performance Liquid Chromatography (HPLC). The sample was prepared according to the method described by Turpeinen., et al. (2003) [21]. The mobile phase was HPLC grade methanol. For separation, we used C18 column (100 × 4.6 mm, 3 µm particle size). Injection volume was 20 microliters and the runtime was 10 minutes. For detection, the wavelength of UV detector was set to 254 nm. For standard curve preparation we used five different concentration of vitamin D standard (10, 20, 40, 80, 120 ng/mL). The curve was linear for area vs concentration data and the goodness of fit (R2) was 0.9985. The lower detection limit was 2.0 ng/mL. Five (5) ng internal standard was used for each sample. Before running the sample, three replicates of a standard were used to evaluate the relative standard deviation ( ± 2%). Serum calcium, inorganic phosphorus and alkaline phosphatase (ALP) activity was measured using the commercially available kit supplied by ThermoFisher Scientific.
Data were presented as mean ± SD or percentage (%). The mean of two groups were compared using unpaired t-test. Linear correlation and regression were used to test the correlation between the measured parameters with graph pad prism 6. Data were tabulated and statistically analyzed with Microsoft Excel 2013. P < 0.05 was considered significant.
In light of the ongoing debate on the optimal vitamin D concentration in pregnant women, most experts are of the opinion that the 25[OH]D concentration in maternal blood should exceed 30 ng/mL [22,23]. However, other authors claim that maternal concentration that fully normalizes vitamin D metabolism and calcium homeostasis is at least 40 ng/mL [24], and still others that > 20 ng/mL is necessary to prevent vitamin D deficiency in the newborn [25].
The following criteria of maternal serum 25[OH] D concentration were used in this study: recommended level > 30 ng/mL, insufficiency 20 - 30 ng/mL, deficiency < 20 ng/mL [26]. For umbilical cord blood, >20 ng/mL was the recommended level and lower values signified vitamin D deficiency [27].
Maternal and neonatal characteristics are presented in table 1. Mean age of the study subjects was 24.78 ± 3.67 years (95% CI 22.68 to 24.68) (range: 18-32 years), most of them were housewives (72%). They were divided into three groups according to their educational status like primary (5 years of education), secondary (10 years of education) and higher secondary (12 years of education). Almost half of the study participants (48%) passed higher secondary or more and 40% of the study subjects completed their high school education and the rest (12 %) has completed primary education. Among the study subjects, 68% are Primigravida (first time pregnancy). In Bangladesh, most women wear saree and salwar kamiz. Specially, after marriage, they prefer saree. In our study, 60 % of the study subjects used to wear hizab with saree or salwar kamiz when going outside.

Table 1: Maternal and neonatal demographic characteristics.
We also analyzed maternal demographic characteristics between mother of LBW baby group and mother of NBW baby group. There was no significant difference between these two groups on education, occupation, clothing, presence of supplement, outing time, and BMI (Table 2).
Mean level of serum 25[OH] D in mothers was 46.45 ± 5.02 ng/ml and in their neonates was 21.89 ± 2.27 ng/ml. The serum 25[OH] D level of the mothers and the neonates were significantly associated (P < 0.01) with a linear correlation coefficient of r = 0.49 (Figure 1). We found no significant difference in 25 [OH] D levels due to dressing style.
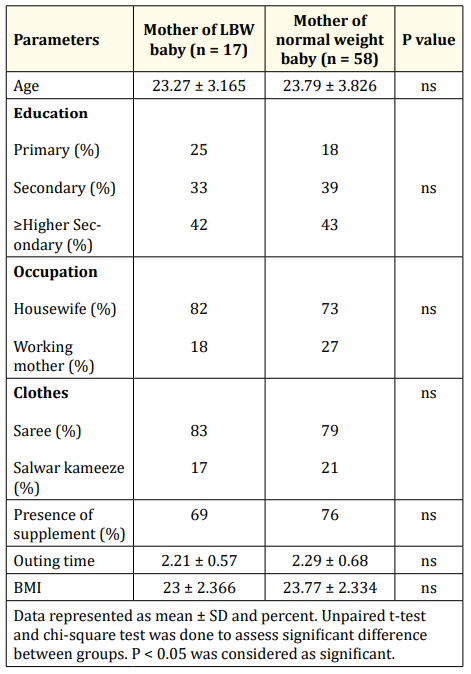
Table 2: Maternal demographic parameters based on mother of LBW baby and mother of NBW baby.

Figure 1: Correlation between maternal and neonatal vitamin D. There was low degree of positive correlation between maternal and neonatal serum vitamin D level (r = 0.49, p < 0.01).
According to serum level of 25[OH] D, study mothers were divided into three groups like sufficient (>30 ng/mL), insufficient (20 - 30 ng/mL) and deficient (< 20 ng/mL) groups. More than half of the study mothers (54%) showed the recommended or sufficient level of serum 25[OH]D level, 20% of the study mothers were insufficient, whereas 26% of the study mothers were deficient in serum 25[OH] D level. Neonates were divided into two groups depending on the umbilical cord blood 25[OH]D contents like recommended or sufficient group (> 20 ng/mL) and deficient group < 20 ng/mL). Almost half of the neonates (54%) of the study group were deficient in 25[OH]D level and 46% of the neonates were found to have recommended or sufficient level of 25[OH]D.
The mean birth weight of neonates was 2.83 kg ± 0.38 (95% CI 2.72 to 2.94) (range: 1.8-3.6 kg) and 22% of the neonates have low birth weight (LBW) (2.33 ± 0.17) (95% CI 2.23 to 2.43). Average birth weight of normal babies was 2.97 ± 0.30 (95% CI 2.876 to 3.064). The mean maternal 25[OH]D level of mothers with normal birth weight babies (n = 58; 77.33%) was significantly higher (50.41 ± 5.00 ng/mL) than that (28.24 ± 6.87 ng/mL) of mothers with low birth weight (LBW) babies (p < 0.001). There was a high degree of positive correlation between maternal 25[OH] D status with neonate’s birth weight (r = 0.593, p < 0.01) (Figure 2). Mothers with LBW babies had lower calcium but higher phosphorous and ALP activity compared to mothers with NBW babies (Table 3).
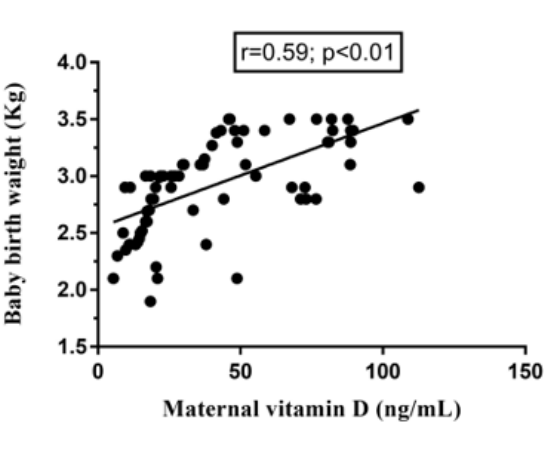
Figure 2: Correlation between maternal vitamin D and neonatal birth weight. There was high degree of positive correlation between maternal vitamin D and neonatal birth weight (r = 0.59, p < 0.01).
![Table 3: Maternal and neonatal status of 25OH[D], calcium, phosphorus, and alkaline phosphates according to birth weight.](https://actascientific.com/ASPE/images/IJMCR/ASPE-03-0328-table3.PNG)
Table 3: Maternal and neonatal status of 25OH[D], calcium, phosphorus, and alkaline phosphates according to birth weight.
Among the study subjects, 22.6% (n = 17) mothers gave birth to LBW babies (birth weight < 2.5Kg). Along with the lower 25[OH] D status in low birth weight neonates (assessed in cord blood samples), other biochemical parameters like calcium, phosphorous, and alkaline phosphatase activity were significantly different when compared to normal birth weight neonates (Table 3). When we compared babies born with low birth weight with those with normal birth weight, we found significantly lower serum 25[OH]D (p < 0.0001), lower serum calcium levels (p = 0.0131), lower phosphorous (p < 0.0001), and higher alkaline phosphatase activity (p < 0.0001). Similar pattern was found when we compared venous blood of corresponding mothers.
Correlation analysis between maternal 25[OH] D and other biochemical parameters shows that maternal 25[OH] D have significant positive correlation with maternal calcium (r = 0.35, p < 0.05) and maternal phosphorus (r = 0.336, p < 0.05). On the other hand, a significant negative correlation was found between maternal Vitamin D and maternal ALP activity (r = -0.53, p < 0.05). The maternal vitamin D has an impact on neonatal serum parameters. Maternal serum 25[OH] D status showed a positive correlation with neonatal 25[OH] D (r = 0.49, p < 0.01) and neonatal calcium (r = 0.195, p < 0.05). Maternal 25[OH] D level showed a negative correlation with neonatal phosphorus (r = 0.24, p < 0.05) and ALP activity (r = 0.35, p < 0.05).
Most of the studies on vitamin D status in the general population identified women and newborns as groups at increased risk of serum 25[OH]D concentrations [28,29]. Vitamin D deficiency is prevalent in various parts of the world including South Asia. Bangladesh is a tropical country of South Asia where sunlight is abundant almost year round; therefore the extent of vitamin D deficiency is rather surprising in Bangladeshi population given its geographic latitude ( 23°42′0″N 90°22′30″E), which support cutaneous vitamin D synthesis year-round. However, a high prevalence of vitamin D deficiency in Bangladeshi women has been reported in some studies [30,31]. In Bangladesh, socioeconomic status have been reported to impact the level of serum vitamin D, calcium and alkaline phosphatase (ALP) activity in pregnant women [32].
More than half of the study mothers (54%) showed the recommended or sufficient level of serum 25[OH] D level, 20% of the study mothers were insufficient, whereas 26% of the study mothers were deficient in serum 25[OH] D levels. The mean value of maternal 25[OH] D level was 45.53 ± 30.81 ng/mL and the neonatal 25[OH] D level was 22.16 ± 12.37 ng/mL. Most of the authors recommend that the pregnant mother should receive 2000 IU of 25[OH] D daily during the third trimester [33]. In the present study, 75% of the pregnant mothers were found to intake 200 IU of vitamin D per day as a component of multivitamin preparation from 15 to 20 weeks to the full term of pregnancy which may contribute to the maternal 25[OH] D level. This is a positive sign of health care in Bangladesh. With the growing economy of the country, consciousness about health care is also growing among people. High income group people usually take their medical care from private hospitals which are expensive but in our study most of the subjects were from moderate to low income group.
The neonates derive the vitamin D through the trans-placental passage of vitamin D metabolites during intrauterine life. The major metabolite to cross the placenta is 25[OH] D with cord level being approximately two-thirds of those found in the mothers [34]. Thus, unless exogenous vitamin D is provided, the vitamin D of the neonates will drop as its half-life is only 3 - 4 weeks. The vitamin D content of the breast milk has been estimated to be between 20 and 60 Iu/L [35] and is not adequate for meeting the requirement of a growing baby [36]. The infants of the mothers with adequate 25[OH] D are likely to improve their vitamin D status faster than those of the mothers with lower serum 25[OH] D level.
Vitamin D metabolism is enhanced during pregnancy and lactation. It crosses the placenta, so the vitamin D level of the newborn is entirely dependent on the maternal 25[OH] D level [37]. Like most of the other studies [38], we found the higher maternal 25[OH] D levels compared to neonatal levels (Figure 1). When the mean value of maternal vitamin D level was 29.61 ng/ml, then the concentration in the cord blood was found to be 21.05 ng/ml; but when the maternal level was found to be 91.66 ng/ml the concentration in the cord blood is found 30.57 ng/ml. Serum 25[OH] D level in cord blood is directly related with relatively lower maternal vitamin D levels but when the maternal 25[OH] D level is relatively higher, the cord blood level not elevated in the similar fashion. These findings may be due to some other factors, including the availability and function of vitamin D binding protein.
Lower 25[OH] D levels in low birth weight groups (both neonate and mothers) are associated with lower calcium, phosphorus levels and higher ALP activity. When we compared the biochemical parameters in cord blood of LBW groups with the normal birth weight groups, there was a significantly higher level of vitamin D, calcium and phosphorus in normal babies than LBW babies (p < 0.05). Mothers of LBW babies (< 2.5 Kg) were found to have low 25[OH] D level. A study conducted by Mannion., et al. showed that the birth weight had been higher in women who consumed food fortified with serum 25[OH] D than those who did not [39]. We found significantly lower calcium and phosphorus level in mothers of LBW babies than the mother of normal weight babies (p < 0.05). As vitamin D facilitates the intestinal absorption of calcium and phosphorus, lower levels of calcium and phosphorus in mothers of LBW babies may be due to lower levels of vitamin D. A study on Pakistani population revealed that mothers of LBW babies have significantly lower levels of calcium and phosphorus than the mothers of normal babies [40].
From our study, it can be said that Maternal low vitamin D level have a negative impact on neonatal birthweight and other parameters like calcium and alkaline phosphatase. Further study on large population may help to strengthen our findings in future.
The authors declare no conflict of interest.
This research was supported by the Ministry of Science and Technology, Government of Peoples Republic of Bangladesh (Grant No: 39.009.006-01.00.049./MED’S-26).We would like to acknowledge the participants of the study.
Copyright: © 2020 Md. Mostafijur Rahman and Saimon Miah., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.