Hend M Hassan1, Mohamed M Sasi1, Raga Elfakhrei2*, Hind M A Alaneezi1, Amal Elfakhri3 and Yousif Sulaiman4
1Department of Paediatric Medicine, Benghazi Children Hospital, Libya
2Physiology Department, University of Benghazi, Libya
3Commuinty and Family Medicine Department, University of Benghazi, Libya
4Pediatric Department, Medical Faculty, Benghazi University, Libya
*Corresponding Author: Raga Elfakhrei, Physiology Department, University of Benghazi, Libya.
Received: October 12, 2020; Published: November 18, 2020
Citation: Raga Elfakhrei., et al. “COVID-19 Pandemic and Increased Frequency of Multisystem Inflammatory Syndrome in Children/Benghazi 2020”. Acta Scientific Paediatrics 3.12 (2020):13-18.
A flare-up of unidentified pneumonia in Wuhan since December 2019 has been developed which draw an extraordinary consideration around the globe. Primary reports from Europe and the USA found an association between severe acute respiratory syndrome coronavirus 2 in children and multisystem inflammatory syndrome in children, also known as paediatric inflammatory multisystem syndrome.
This study focused on the association between COVID-19 and multisystem inflammatory syndrome in children in the Eastern region of Libya, namely Benghazi a case summary presentation. A series of 12 cases has been described in details. All cases presented with fever, skin and mucous membrane manifestations in addition to GIT symptoms. Three cases have had CNS involvement, three have lymphadenopathy, two cases with cardiac manifestations and two renal with renal involvement. Laboratory data revealed elevated inflammatory markers namely ESR and CRP and lymphopenia. Diagnosis was based on rapid test (IgG, IgM), whereas four cases were diagnosed by PCR. The overall prognosis of all cases is very good with an average hospitalization period of 5 - 7 days. Management strategy included IV antibiotic, oral aspirin and sandoglobulin.
Keywords: Multisystem Inflammatory Syndrome; COVID-19; Paediatric
MSI-C: Multisystem Inflammatory Syndrome in Children; KD: Kawasaki Disease
Severe acute respiratory syndromes coronavirus-2 (SARSCoV-2) are significant microorganisms for human and vertebrates. They can affect numerous system in the body including respiratory, gastrointestinal, hepatic and focal sensory system of human, animals, fowls, bat, mouse and numerous other wild creatures [13].
A flare-up of unidentified pneumonia in Wuhan since December 2019 has been developed which draw an extraordinary consideration around the globe. The causative operator of this secret pneumonia has been recognized as a novel Covid (nCoV) by profound sequencing and etiological examinations by various autonomous research facilities of China. On 12 January 2020, the WHO named this new virus as the 2019 novel coronavirus (2019-nCoV). On 11 February 2020, the WHO named the disease caused by the (2019nCoV) as coronavirus disease (COVID-19) [4].
The impact of COVID-19 which is caused by the novel corona virus has been widespread, with a total detected cases (up to 29.09.2020) of 33758805 worldwide. Since the virus was identified in January 2020 [5].
In Libya, according to the national center for disease control the total number of confirmed cases of COVID-19 up to 28/09/2020 was 34014, active cases 14572, death 540. In the Eastern region of Libya the total confirmed cases 3024, with 2218 active cases, the vast majority of cases were from Benghazi as they accounted for 2123 total cases and 1725 active cases followed by Tobruk [6].
At the beginning, the preliminary data have been focused on severe respiratory manifestations, which are seen mainly in adults, with a dearth data on the burden of COVID-19 in children [7]. Later on, many studies have addressed the issue of covid 19 in paediatric age groups. For instance, Dong., et al. reported that 4% of virologically confirmed cases of COVID-19 in children are asymptomatic and this rate almost underestimate the true rate of asymptomatic infection because many children who are asymptomatic are unlikely to be tested [8].
Among kids who were affected, 5% had dyspnea or hypoxemia (a significantly lower rate than what has been accounted for adults) and 0.6% advanced to intense respiratory distress syndrome or multiorgan failure (a rate that is likewise lower than that found in adults). Preschool-aged children and infants were more likely than older children to have severe clinical manifestations [8]. Another study directed on hospitalized Norwegian kids identified COVID-19 in 10% of hospitalized kids with respiratory infections [9].
In Pakistan, children and adolescents younger than 20 years of age constitute 10.6% (24,625 of 231,818) of the total reported confirmed cases of COVID-19 up to July 8, 2020, with a mortality of 0.3% for those aged 10 years or younger and 0.5% for those aged 11 - 20 years [10].
Primary reports from Europe and the USA found an association between corona virus infection in children and multisystem inflammatory syndrome in children (MIS-C), also known as paediatric inflammatory multisystem syndrome [10,11]
The affected children may require admission to intensive care units with a multisystem inflammatory condition with some features similar to those of Kawasaki disease and toxic shock syndrome. Some Case reports even described a presentation of acute illness accompanied by a hyperinflammatory syndrome, leading to multiorgan failure and shock [12,13].
Kawasaki disease (KD) is a rare acute febrile multisystem inflammatory vasculitis [14]. It is the leading cause of acquired heart disease in children, affects children less than 5 years of age it is triggered by some viral and bacterial infections. However, its exact etiology still unclear [15].
The pathogenesis of hyper-inflammatory syndrome can be explained by a phase of elevated IL-6 causes “cytokine storm”, an increased immune reaction of the infected child [16]. The clinical manifestations of this phase comprise multi-organ failure, shock, myocarditis, respiratory failure, and renal failure, somehow similar to hemophagocytic lymphohistiocytosis. Decreased T helper, cytotoxic lymphocytes, and regulatory lymphocytes, as well as increased inflammatory cytokines and biomarkers, can be found in this stage [17].
Clinically KD is characterized by prolonged fever lasting more than five days, with dysmorphic skin rashes and diffuse mucosal inflammation, bilateral non-purulent conjunctivitis, indurative angioedema seen commonly in hands and feet, and cervical lymphadenopathy. Along with a broad range of nonspecific clinical features such as irritability, uveitis, aseptic meningitis, cough, vomiting, diarrhea, abdominal pain, urethritis, arthralgia, arthritis, hypoalbuminemia [18].
WHO described the criteria to diagnose MIS-C as the following:
Children and adolescents 0 - 19 years of age with fever for three days and more
AND two of the following:
On the other hand, the Centers for Disease Control and Prevention (CDC) has defined the disease considering the following features:
A series of 12 cases diagnosed by serology and clinical picture, all are Libyan, their age ranged between (2-14 year), out of them 9 males and 3 females, all are from Benghazi except 4 cases were from Elmarj, Derna, Tazerbo and Jalo (black race), all of them presented with fever, lethargy, GIT manifestations in particular, vomiting, diarrhea and abdominal pain, 2 - 3 days after fever most of them demonstrated mucocutaneous manifestations typical for KD (Figure 1 and 2) with perianal erythema in three cases (Figure 3) and another case developed palmer erythema. Three cases exhibited cervical lymph nodes enlargement, another 3 case presented with conjunctivitis.

Figure 1: Skin rash.

Figure 2: Strawberry tongue with cracked lips.

Figure 3: Perianal edema.
Two cases presented with respiratory symptoms (cough, dyspnea, chest pain). Another case presented with myocarditis while nephritis was evident in another case.
All of the cases were previously healthy and have no any chronic illness except a case known for bronchial asthma that presented with hands and feet swelling which occurred in further 3 cases. At time of presentation, all of them have no focal site of infection.
Meningeal signs were positive in three cases (Table 1).
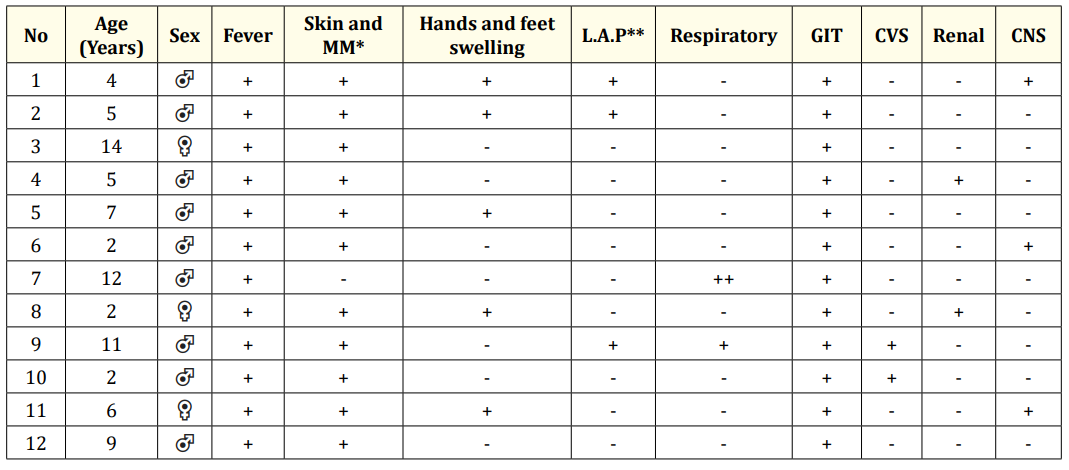
Table 1: Clinical manifestations of the cases. *L.A.P: lymphadenopathy; **M.M: Mucous Membrane.
Chest x-ray of two patients revealed that there is bilateral interstitial infiltration and another one showed significant opacity which has been confirmed as pleural effusion by ultrasound in addition to ascites (Figure 4).
Figure 4: Case 7 with pleural effusion.
ECG was significant in only one case which showed right bundle branch block.
ECHO in all cases was normal except one with left ventricular dilatation and mild aortic regurgitation and another case had dilated cardiomyopathy.
Ten Patients who presented with moderate disease treated with I.V antibiotics, oral aspirin, I.V sandoglobulin, out of them three cases received I.V methylprednisolone. Two mild cases treated only by oral aspirin.
One case were diagnosed late by serology and getting well without treatment.
Duration of hospital admission of all cases ranged between 5 - 7 days , their clinical conditions showed signs of improvement within two days, none of them needed ICU admission, all were discharged in a good health on oral treatment and follow up guidance with cardiologist.
KD is an infection induced vasculitis that influences mediumsized arteries, which primarily affects infants and children younger than 5 years [19]. The gender and age distribution as reported elsewhere boys more commonly diagnosed and the majority of cases occurring in children aged 5 years. In Japan, the peak incidence is at 11 months of age and 85% of cases occur in those aged 5 years [20]. It occurs with variable incidence all over the world its incidence in Arab countries of the North Africa or Maghreb countries is not exactly known. However, it is reported to be low [21].
Since the beginning and spread of the ongoing pandemic of COVID-19 infection, multiple reports have been published describing cases of hyper inflammatory syndrome with multiorgan involvement in paediatric age group. Some of these reports were about children with clinical picture consistent with KD besides laboratory test suggestive of current or past SARS-CoV-2 infection (ECDC 2).
The current case series confirmed that since the time of spread of COVID-19 in the city of Benghazi there has been an obvious raised incidence of KD among children. Although there are no documented figures of KD in Libya specifically the Eastern region, the paediatricians claimed that prior to COVID-19 epidemic we have never received such a frequent cases of KD and MIS-C which reached in some times to three cases a day. It worth mentioning that this growth in KD incidence was reported in different countries and regarded as one of common clinical presentations of COVID-19 in paediatric age group despite that, no causal link has been established between MIS-C and COVID-19 in children [14].
Available literature pointed that viruses have an important role in human vasculitis disease. Several pathogens such as herpesvirus, novel human coronavirus, Epstein-Barrvirus and parvovirus B19 have been suggested as possible agents in the pathogenesis of KD [22].
COVID-19 affected incidence and presentation of classic KD in paediatrics. The affected cases were of different age groups starting from two years and more frequently in older children. Some cases aged 9 - 14 years. Male were the predominant victims just like the known gender difference of the disease. There was few discrepancy from the available knowledge of the classic KD prior to COVID-19 epidemic which is known by the typical changes in the mucous membranes and with less frequency of GIT symptoms.
Poor response to antibiotics is a feature of the disease [23].
In Pakistan a report published online in August 2020 documented two major presentations of KD induced by COVID-19, atypical or typical Kawasaki disease (6 of 8, 75%) and a more severe second one with shock or low cardiac output (2 of 8, 25%). Common presenting features were fever, body aches and abdominal pain. Patient 6presented with altered consciousness and signs of meningism, and an initial diagnosis of meningoencephalitis was made [17].
Classic KD was documented to be of seasonal variation in the incidence according to geographic area, Canada, Korea, Japan, and China the peak incidence in winter, while in Taiwan its peak during spring .In North of Africa countries the peak was in spring with the secondary peak in winter in Algeria and summer in Tunisia which could be related to allergy and viral seasons in general as a relationship between KD and immunological dysregulation is suggested [24]. In this series of MIS_C and classic KD there is an accumulating cases in a dramatic excess started in August which is dry and hot time in Libya as it is summer season. The peak of disease might occur later and the rule of seasonality of classic KD might be broken by COVID-19 epidemic.
COVID-19 epidemic can be seen a leading factor for MIS-C.
Twin epidemics of COVID-19 and MIS-C has been resulted. Paediatric age group were generally considered safe and they act as a disease transmitters in COVID-19 epidemic. However, COVID-19 is manifested as MIS-C which lead to greater burden of the epidemic on health sector and resulted in an increased morbidity and hospital admission of children.
The photos have been published after the permission of the family.
Copyright: © 2020 Raga Elfakhrei., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.