Khaoula Khemakhem1, Leila Cherif1*, Wiem Kammoun1, Mahmoud Ziraoui1, Khadija Baccouche1, Lobna Zouari2, Hela Ayadi1, Imen Hadjkacem1 and Yousr Moalla1
1Department of Child and Adolescent Psychiatry, Hedi Chaker Hospital, Sfax, Tunisia
2Department of Psychiatry C, Hedi Chaker Hospital, Sfax, Tunisia
*Corresponding Author: Leila Cherif, Department of Child and Adolescent Psychiatry, Hedi Chaker Hospital, Sfax, Tunisia.
Received: September 26, 2020; Published: November 18, 2020
Citation: Leila Cherif., et al. “Quality of Life in Caregivers of Children with Autism Spectrum Disorders: A Tunisian Study”. Acta Scientific Paediatrics 3.12 (2020): 03-08.
Objective: The purpose of this study was to investigate the quality of life and its related factors among caregivers of children with autism spectrum disorders.
Methods: The study was performed in the department of child and adolescent psychiatry of Sfax and included eighty caregivers of children with autism spectrum disorders. The short form-36 health survey questionnaire was used to assess the quality of life among the caregivers. To evaluate the severity of autism spectrum disorders, the Childhood Autism Rating Scale was used. The anxiety rating scale of Hamilton and the Hamilton Depression Rating Scale were used to assess anxiety and depression among them.
Results: Impaired quality of life was found in 60.7% of the caregivers. The quality of life was more impaired among younger children and those undergoing a speech therapy.
Conclusion: The findings of this study indicate the effect of both children young age and speech therapy on quality of life, and emphasize the link between anxiety, depression and impaired quality of life among caregivers of children with autism spectrum disorders.
It reiterate the need for early interventions which assist parents in better managing feelings of depression and anxiety.
Keywords: Quality of Life; Autism; Caregivers
ASD: Autistic Spectrum Disorder; CASD: Caregivers of Children with Autistic Spectrum Disorder; QOL: Quality of Life; HAM-A: Hamilton Anxiety Rating Scale; HDRS: Hamilton Depression Rating Scale; CARS: Childhood Autism Rating Scale
Children with autism spectrum disorder (ASD) are recognized by significant impairment in communication, social interaction and emotional reciprocity, and by the presence of restricted and repetitive behaviors or interests [1]. These significant and persistent challenges associated with ASD, may affect the well-being of immediate family members as well as the child [2]. In fact, families with a child with ASD may find themselves burdened with a lifelong responsibility of caring for their children. They may experience periods of great difficulties in obtaining an accurate and timely diagnosis, as well as the necessary treatments or interventions for their child difficulty throughout his development [3]. These daily challenges may lead to deterioration of quality of life of parents in different domains [4]. Some authors suggest that caregivers of children with autism spectrum disorder (CASD) experience problems with physical health [5,6] and poorer overall well-being [7] and quality of life (QOL) [8]. They report significantly more selfperceived health problems than the control parents, as assessed by the Health Status Questionnaire (SF-36) [9]. This finding reflects not only the caregiving burden associated with parenting a child with an ASD but also has possible secondary effects on the child and vice versa [10].
Several Western studies show that QOL and parental health are influenced, in part, by factors related to the characteristics of the ASD and the child’s particular needs, by another part by socio-demographic or psychodynamic variables of parents [11,12].
Despite the prevalence of studies on QOL in CASD [13], there is a paucity of studies exploring the variables related to the QOL in CASD [14]. To our knowledge, only one study dealing with this subject has been published in the Tunisian population. It involved 50 parents of 50 children with ASD and demonstrated that aggressiveness among children with ASD was the predominant factor that significantly altered the parents’ QOL [15]. Yet, understanding the effect of the variables related to both parents and children is essential to implementing interventions to improve parents’ QOL and to reduce their psychological stress.
The objective of this study was to estimate the prevalence and the determinants of impaired QOL in CASD.
The study was cross-sectional, carried out on 80 CASD (62 mothers and 18 fathers) who accompanied their children to the child and adolescent psychiatry department at the Hedi Chaker Hospital, in Sfax, either for consultation or for patient care at the day hospital. It was performed over four months, from September to December 2014.
All parents were informed about the objectives of the study and the procedures to participate. Informed consent was taken from them. Data on participating parents were gathered through self-administered questionnaires. Parent questionnaires included items on child, parents, family characteristics and other issues.
The ethics committee of the Medicine University of Sfax approved the research.
The short form-36 health survey questionnaire (SF-36) was used to assess the QOL among CASD [16]. To evaluate the severity of ASD, the Childhood Autism Rating Scale (CARS) was used [17]. The anxiety rating scale of Hamilton (HAM-A) [18] and the Hamilton Depression Rating Scale (HDRS) [19] were used to evaluate anxiety and depression among CASD.
The quality of life (QOL) was screened by the Tunisian validated version of the short-form 36 (SF-36). The short form-36 health survey questionnaire (SF-36) [16] is a 36-item Likert-type scale measuring physical functioning, role physical function (problems with work or daily activities as a result of physical health), bodily pain, general health perception which together comprise the physical component summary score. The scale also measures mental health, role emotional function (problems with work or daily activities because of emotional function), energy, and social functioning, which together comprise the mental component summary score. The SF36 questionnaires were scored for each domain; possible scores range from 0 to 100, with higher scores indicating better HRQOL. The normative scores have a mean of 50 and standard deviation of 10, which is representative of the mean and standard deviation of the findings in the general US population.
Autism is evaluated using the Childhood Autism Rating Scale (CARS) [17]. This scale consists of 15 items and rate children from 1 to 4 for various criteria (midpoints are also allowed) with total score ranging from 15 to 60 and with a minimum score of 30 considered as a cutoff for a diagnosis of autism. The test interpretations based on the composite score range from non-autistic to mildly autistic, moderately autistic, or severely autistic.
A questionnaire was submitted to parents to evaluate the prevalence of anxiety using the anxiety rating scale of Hamilton (HAMA) [18]. The HAM-A is a 14 items scale. Each item is scored on a 5-point scale, ranging from 0= not present to 4= severe, with a total score range of 0 - 56. A score less than 17 indicates mild anxiety, 18 - 24 mild to moderate anxiety and 25 - 30 moderate to severe anxiety.
The prevalence of depression was also assessed based on the Hamilton Depression Rating Scale [19]. The first 17 items of the Hamilton Depression Rating Scale were used as part of the psychiatric interview. Scoring is based on the 17-item scale and scores of 0 - 7 are considered as being normal, 8 - 17 suggest mild depression, 18 - 25 moderate depression and scores over 26 are indicative of severe depression; the maximum score being 52 on the 17-point scale.
All assessments were arabized but not validated in Tunisian population. Only the SF 36 was validated.
Data entry and statistical analysis were performed using the SPSS software in its 10th version.
Comparisons of two means were made using Student’s t-test. Comparisons of several means were made using the ANOVA test. Percent comparisons were made by the Pearson chi-square test (χ2). In all statistical tests, p values less than 0.05 were considered statistically significant.
The study included 80 parents who have at least one child diagnosed with ASD. The sample showed predominance of mothers compared to fathers (62 versus 18). At the time of the study, the mean age of mothers was 35 years 8 months (± 6.13) and the mean age of fathers was 42 years 4 months (± 6.14). Among parents, 68.8% of mothers and 56.3% of fathers had a secondary/university educational level. Consanguinity was noted in 26.3%.
The sample of children consisted of 55 boys and 25 girls, with an average age of 5.06 years (±1.53). At the time of the study, 65% of children were attending kindergarten or preschool. Table 1 shows variables related to care and to the severity level of autism.
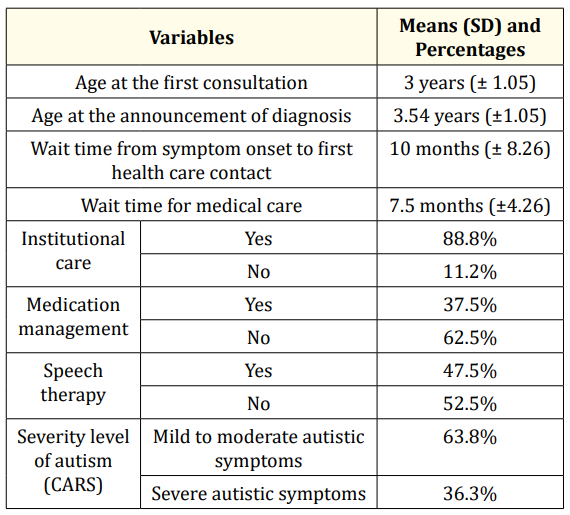
Table 1: Variables related to the care and to the severity level of autism among children. CARS: Childhood Autism Rating Scale.
In our study population, impaired QOL was found in 60.7% of parents. The mean scores are illustrated in table 2.
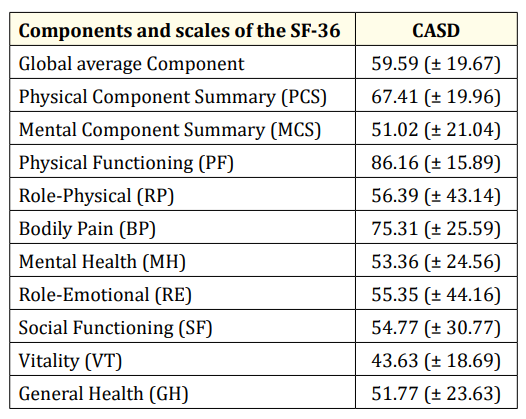
Table 2: Quality of life among the caregivers according to the SF-36. CASD: Caregiver of children with autistic spectrum disorder.
T test shows that there is a significant association between QOL impairment and the age of children. The CASD with altered QOL have their children mean age about 4.72 versus 5.91 in the CASD with normal QOL (p = 0.006). Significant positive linear correlations between QOL and age at the first consultation and age at announcement of ASD diagnosis were raised (See table 3).
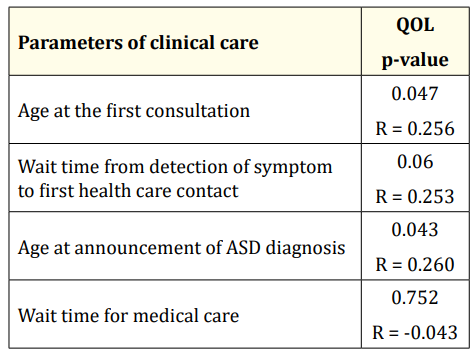
Table 3: Associations between quality of life and factors connected to the care. QOL: Quality of Life; ASD: Autistic Spectrum Disorder.
According to the HDRS, 57.7% of the caregivers were depressed. Severe depression was found in 8.5% of cases and mild to moderate depression in 49.2% of cases. In addition, 57.6% of the CASD were anxious according to the HAM-A, with 23.8% of severe anxiety and 33.8% of mild to moderate anxiety.
Studying the relationship between depression, anxiety and QOL, there was a significant negative linear correlation between the depression score and the overall scores of QOL, and between anxiety score and all scores of QOL except Role-Physical, Bodily Pain and Role-Emotional domains (See table 4).
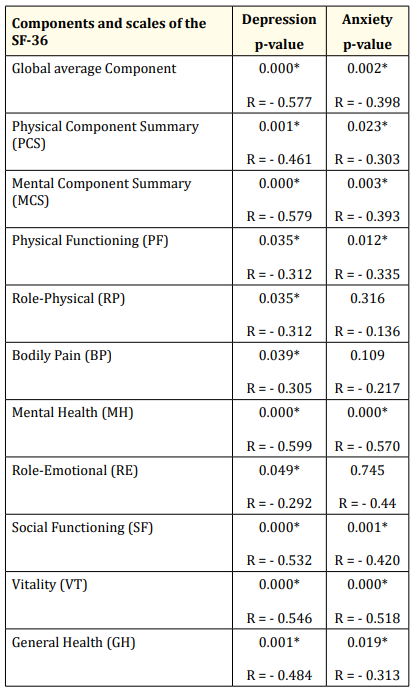
Table 4: Associations between anxiety, depression and quality of life. *Significant.
Caring for a child with ASD is a lifelong responsibility for caregivers that may increase their psychological distress and deteriorate their QOL. In this study, the QOL and the factors affecting the QOL of caregivers of children diagnosed with ASD were investigated.
According to the present study, impaired QOL was found in 60.7% of caregivers. It is clear that reports from across countries and cultures suggest that caring for a child with ASD significantly affects the parents or even the caregivers QOL [8,20,21]. Compared with QOL in parents of children with attention-deficit-hyperactivity disorder (ADHD) in a Tunisian group, QOL of CASD was more impaired [22]. In fact, unlike ADHD, knowledge about ASD is still lacking and treatment is mostly unavailable or unaffordable [14].
In the present study, the mean of Physical Component Summary scores was higher than the mean mental summary scores (67.41 VS 51.02) (Table 2). Similarly, authors have shown that physical health components of QOL among parents of children with ASD were higher than QOL in parents of children with intellectual developmental disabilities [23] and that mental health components were the most impaired [15,23].
As regards the impact of ASD management on the QOL of CASD, literature has reported that the QOL of the parents having children with ASD who attend educational institutions is better than those whose children do not attend school. This may be due to the parent being able to set aside time for himself when the child is outside the home, and to the positive contribution to the child in developing his/her independence skills. It could also be attributed to the positive contribution of support systems such as education and healthcare [24].
On the other hand, the QOL was more impaired when children were younger (p = 0.043). Parents are very hopeful in the beginning, therefore, they do all their best to achieve positive results. In fact, over time, parents become more comfortable with the diagnosis. Their expectations become more realistic and the quality of life improves. In the same way, we explain the positive linear correlations between QOL and age at the diagnosis of ASD diagnosis (p = 0.047). The study of Woodgate., et al. [25] extended prior research, which documented that high levels of stress are present in mothers when their children are quite young. Wait time for medical care was negatively associated with QOL (p = 0.06). Many studies emphasized the importance of an early intervention and enrolment of children with ASD in special learning programs which may increase the independence of the child and reduce the burden on his/ her caregivers [26].
The fact that these characteristics are the most stressful for parents is important for professionals to know when working with families of young children. Actually, as families learn more about autism and about their children’s individual capacity and style of social engagement, parents’ stress associated with the appraisal of children’s limited social relatedness may diminish.
Contrary to other studies, the present study showed no significant relationship between QOL in CASD and the severity of ASD. In general, a statistically significant relationship was found between the disease severity and the QOL scores of the parents [24,27-29].
In the current study, there was a significant association between an impaired quality of life, depression, and anxiety (Table 4). This association is recognized in literature [24]. It is obvious that perceived stress and depression among CASD are significant predictors of physical health, psychological health, social relationships, and environment as related to quality-of-life perceptions [30]. A study conducted in Turkey found that, in the presence of a psychiatric diagnosis in the parent, QOL is significantly negatively affected [24]. In general, low levels of mental health among parents of children with ASD expose them to mental health challenges, given their concerns about the future, their perspectives on disabled children, and the sense of guilt developed over time [23].
Our study suggests that the diagnostic of autism in children has repercussions on parents with impaired quality of life, particularly in regards to the mental health components. The additive effect of both anxiety and depression on the impairment of quality of life raise the importance for both symptoms investigation in the clinical evaluation of CASD children. The recognition and treatment of comorbid depression and anxiety are important in improving the quality of life among CASD children. It can also be stated that ASD management could burden the CASD instead of alleviating their suffering, and that the younger the children, the lower the QOL of CASD. Therefore, it is extremely important to improve and upgrade the services for children with autism and their parents, and it is highly recommended to develop early comprehensive health care strategies to support those who are in direct daily contact with a child with autism.
Thanks are due to all parents of children patients with autism who participated in this study.
Copyright: © 2020 Leila Cherif., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.