Sophia Kiwango1*, Pendo Mlay1, Kiondo S Kiondo1, Caroline Amour2, Innocent B Mboya2,3 and Michael J Mahande2
1 Department of Obstetrics and Gynecology, Kilimanjaro Christian Medical Centre
(KCMC), Moshi, Tanzania
2 Department of Epidemiology and Biostatistics, Institute of Public Health, Kilimanjaro
Christian Medical University College (KCMUCo), Moshi, Tanzania
3 School of Mathematics, Statistics, and Computer Science, University of KwaZulu-Natal,
Pietermaritzburg, South Africa
*Corresponding Author: Sophia Kiwango, Department of Obstetrics and Gynecology, Kilimanjaro Christian Medical Centre (KCMC), Moshi, Tanzania.
Received: September 05, 2020; Published: October 28, 2020
Citation: Sophia Kiwango., et al. “The Effect of Inter-Pregnancy Interval on the Recurrence Rate of Spontaneous Preterm Birth among Women who Delivered at KCMC Hospital, Tanzania: A Registry-based Cohort Study”. Acta Scientific Paediatrics 3.11 (2020):59-65.
Background: Inter pregnancy interval has been associated with adverse neonatal outcomes, including preterm birth and low birth weight. Little is known on the effect of Interpregnancy interval on the recurrence of preterm birth. This study aimed to determine the effect of Interpregnancy interval on the recurrence of spontaneous preterm birth among women who delivered at KCMC hospital, Northern Tanzania.
Methods: We conducted a retrospective cohort study using maternally-linked birth registry data from all recorded women who delivered two consecutive singleton pregnancies and spontaneous preterm birth in their first pregnancy from 2005 - 2015 at KCMC referral hospital. The outcome was the recurrence of spontaneous preterm birth and IPI was the primary exposure of interest. We analyzed data using STATA version 15 and estimated the relative risk and recurrence risk of spontaneous preterm birth with 95% confidence intervals using the log-binomial regression model at a 5% statistical significance level.
Results: The recurrence rate of spontaneous preterm was 23.1%. IPI of ≥ 60, 18 - 23 and 12 - 17 months were associated with lower risk (RR: 0.79; 95%CI 0.53 - 1.16), (RR: 0.78; 95%CI 0.54 - 1.13) and (RR: 0.92; 95%CI 0.65 - 1.31) of SPTB in the subsequent pregnancies compared to 24-59 months. However, these associations were not statistically significant. On the other hand, inadequate (< 4) ANC visits during pregnancy significantly increased the risk of SPTB (RR: 3.98; 95%CI: 3.05 - 5.20) in the subsequent pregnancy.
Conclusion: The recurrence of SPTB is high among women in this study. The short and long IPI were all protective against the risk of recurrence SPTB while inadequate (< 4) ANC visits increased the risk. Interventions to promote optimal Interpregnancy interval and close follow-up of women at risk, especially during ANC visits, may reduce the risk of recurrence of preterm birth and associated adverse outcomes.
Keywords: Inter-Pregnancy Interval; Recurrence Risk; Spontaneous Preterm Birth; Tanzania
Interpregnancy interval (IPI) is the time lapse between the termination of one pregnancy and conception of a subsequent pregnancy [1]. The World Health Organization (WHO) recommend the interval between two successive birth of 33 months (24 months of breastfeeding plus nine months of pregnancy), or six months if the pregnancy ended up with abortion [1]. Optimal IPI (24 - 59 months) has been associated with favorable maternal and perinatal outcomes [1]. Both short (< 24 months) and long (> 60 months) IPI increases the risk of adverse maternal outcomes such as maternal anaemia in pregnancy, preeclampsia, placental abruption, maternal depletion syndrome, hypertensive disorders of pregnancy and adverse perinatal outcomes including preterm birth, low birth weight and perinatal death [2].
Poorly timed pregnancies are detrimental to mothers and newborns. This calls for a need to practice family planning to reduce these adverse outcomes. The WHO, therefore, recommends a minimum of two years (24 months) after a live birth before attempting to conceive again to prevent adverse pregnancy outcomes [1,3]. Moreover, short IPI is known for a long time as a risk factor for preterm birth, which is a significant contributor to the rise of perinatal mortality, particularly in low resourced countries, including Tanzania [4].
The relationship between IPI and preterm birth follows a Jshaped structure [5]. On the other hand, preterm birth increases the risk of recurrence in subsequent pregnancies [6]. This means that women with a previous history of preterm birth are more likely to have preterm birth in their next pregnancy. Furthermore, recurrent preterm birth also increases the risk of perinatal death [7], among other adverse pregnancy outcomes.
Globally, 11% of babies are born preterm (about 15 million babies) [8]. A previous hospital-based study in North-Eastern Tanzania reported a prevalence of preterm birth of 14.3% [4], while the absolute recurrence rate of preterm birth was 17% [9]. Little is known about the impact of IPI on the recurrence rate of spontaneous preterm birth in Tanzania. Therefore, it is essential to determine how short or long IPI may affect the recurrence of this outcome. This information may help to guide clinical decisions and counseling for women at risk of recurrent preterm birth, especially those with previous preterm birth. We, therefore, aimed to determine the effect of IPI on the recurrence rate of spontaneous preterm birth among women who delivered singleton in successive pregnancies at KCMC referral hospital, northern Tanzania.
We conducted a retrospective cohort study using maternallylinked data from KCMC medical birth registry data between 2005 and 2015. The KCMC medical birth registry records information for all mothers delivered in the obstetrics and gynecology department at KCMC referral hospital within 24 hours after delivery or as soon as mothers have recovered in case of complicated deliveries. On average, the total number of 4,000 deliveries occur every year. The KCMC is a referral, consultant, and university teaching hospital located in the Moshi Municipality, a capital city of the Kilimanjaro region, northern Tanzania. It serves over 15 million people, which includes the local community in the catchment area and referred cases from six surrounding regions. High-risk deliveries are referred for observation and delivery in this facility, while women in the local community may come to deliver on their own.
Women who delivered two consecutive singleton pregnancies from 2005 - 2015 with spontaneous preterm birth (< 37 weeks) in their first pregnancy recorded in the birth registry participated in this study. There were 41,038 total deliveries at KCMC between the years 2005 - 2015. We excluded deliveries with missing unique identification numbers since they could not be linked to a specific mother. We also excluded 12,875 women with multiple births and intrauterine fetal death (IUFD), or congenital abnormalities, 19,447 with only one birth, 7,102 with normal deliveries, and 632 missing gestational age. We, therefore, analyzed data for 982 deliveries with complete follow-up data (Figure 1).

Figure 1: Schematic presentation of the cohort follow-up: Data from the 2005-2015 KCMC medical birth registry.
The data extraction sheet was used to obtain information from the medical registry data base. The birth registry records information for all mothers who deliver in the obstetrics and gynecology department. Trained midwives perform daily interviews using a questionnaire within 24h of the delivery, or as soon as a mother has recovered. Data is also obtained from the medical records in the hospital. Data is registered in the medical birth registry office. A well-structured English questionnaire was used to extract all relevant information pertaining to study variables. These were later transferred into a computer data base containing all corresponding variables needed for the study.
The primary outcome was recurrent spontaneous preterm birth defined as birth < 37 weeks of gestation on the subsequent pregnancy. Gestational age (GA) was estimated using the date of last menstrual period (LMP), using this formula: Gestational age (days) = Gestational age (weeks) x 7 days.
The primary exposure variable was Interpregnancy interval (IPI) defined as the time lapse between the termination of one pregnancy and conception of a subsequent pregnancy given as; IPI (days) = (date of birth of the second child - date of birth of the first child) - GA at the birth of the second child. We then categorized IPI as 0 - 5, 6 - 11, 12 - 17, 18 - 23, 24 - 59 and ≥ 60 months.
Other independent variables included maternal background characteristics, i.e., age in years (< 35 vs. ≥ 35 years), education level (primary, secondary and above), occupation (unemployed, employed), religion (Catholic, Protestant, Muslim), area of residence (rural vs. urban), tribe (Chagga, pare, others), number of antenatal care (ANC) visits (< 4 times vs. ≥ 4 visits), alcohol use during pregnancy (Yes vs. No), place referred from (home, hospital and others).
We performed data cleaning and analysis using STATA version 15.1 (StataCorp LLC, Texas, USA). Numeric variables were summarized using means and standard deviations while categorical variables using frequencies and percentages. We used the Chi-square (c2) test for comparison of proportions of IPI by participant characteristics. We considered deliveries as the primary unit of analysis. A log-binomial regression model was used to estimate the relative risk and recurrence rate (RR) of spontaneous preterm birth (SPTB) with 95% confidence intervals (CI) while adjusting for potentially confounding variables. The robust variance estimator accounted for the correlation of observations (deliveries) within mothers. We also tested for multicollinearity of covariates in the models and found no evidence of the correlation between independent variables. We considered a p-value of < 5% to be statistically significant.
The mean age of women in this study was 30 years, and the standard deviation of 5.3 years. Among women aged < 35 years, 46% had short IPI, 11.7% had long IPI, and 42.1% had IPI of 24 - 59 months. Among women with secondary education level and above, 47.2% had short IPI, and 12.3% had long IPI. Furthermore, 45.3% of women who were employed followed the optimal IPI of 24 - 59
months (Table 1).
Only 5.6% of the women who referred from the hospital had a long (≥ 60 months) IPI. Among women with ≥ 4 ANC visits, 43.3% had short IPI, compared to 13.5% with long IPI (Table 2).
Less than half (43.6%) of women who had SPTB in the first pregnancy had optimal IPI and 12% had a long (> 60 months) IPI (Figure 2).
The recurrence rate of SPTB in the second pregnancy among women who had SPTB in the first pregnancy at KCMC referral hospital from January 2005 to December 2015 was 23%.

Figure 2: Percentage distribution of IPI among women who had SPTB in the first recorded pregnancy at KCMC referral hospital from January 2005 to December 2015 (N = 982).

Table 1: IPI by maternal characteristics (N = 982). *Mean age (SD) of women is 30 (5.3) years.

Table 2: IPI by pregnancy-related characteristics (N = 982).
The predictors for Recurrence of SPTB are shown in table 3. Using the IPI categories of 24 - 59 months as the comparison group, regression analysis showed both short and long IPI had a protective effect on the Recurrence of SPTB. In the unadjusted analysis, mothers with extremely lower IPI (0 - 5 months) had a significantly lower risk of experiencing SPTB in subsequent pregnancies (RR: 0.60; 95%CI 0.37 - 0.97, p = 0.04) compared to those with optimal IPI (24 - 59 months). Adjusted for mother characteristics, those with an IPI of ≥ 60, 18 - 23 and 12 - 17 months had (RR: 0.79; 95%CI 0.53 - 1.16), (RR: 0.78; 95%CI 0.54 - 1.13) and (RR: 0.92; 95%CI 0.65 - 1.31) lower risk of SPTB in the subsequent pregnancies. However, these associations were not statistically significant.
On the other hand, having inadequate (< 4) ANC visits during pregnancy is the only factor that significantly increased the risk of SPTB (RR: 3.98; 95%CI: 3.05 - 5.20, p < 0.001) in the subsequent pregnancy, adjusted for other factors. Mothers aged greater than 35 years (RR: 1.04; 95%CI: 0.81 - 1.33) and alcohol use during pregnancy (RR: 1.05; 95%CI: 0.81 - 1.37) also increased the risk of SPTB in the subsequent pregnancy, but these associations were not statistically significant (Table 3).
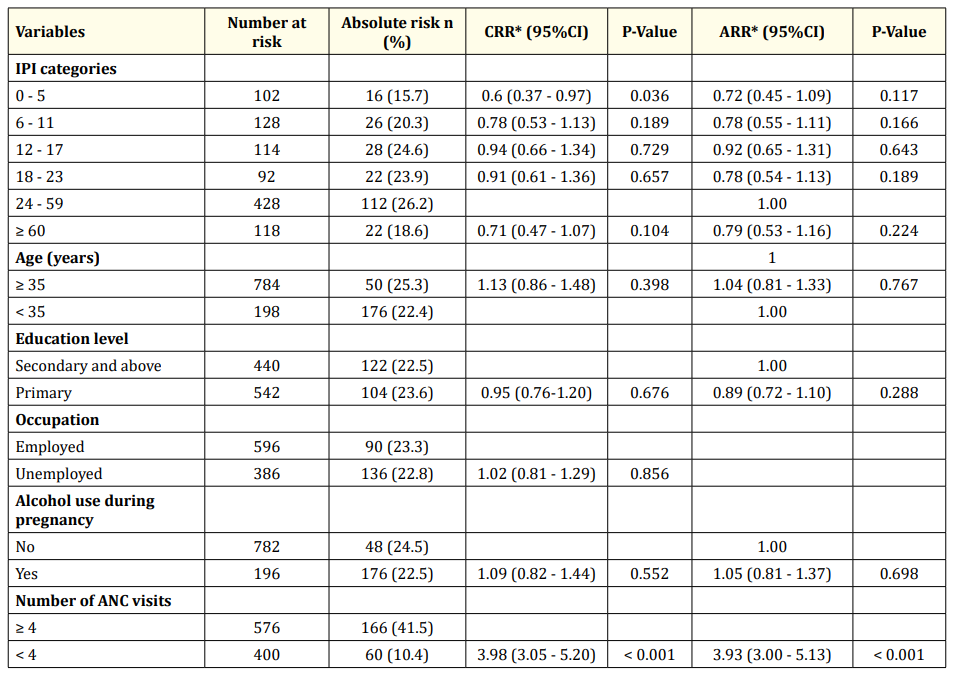
Table 3: The effect of IPI on recurrent spontaneous preterm birth and its predictors in a subsequent pregnancy (N = 982). *CRR: Crude Relative Risk; **ARR: Adjusted Relative Risk (adjusted for maternal age and maternal education level).
We aimed to determine the effect of IPI on the recurrence rate of SPTB. The recurrent PTB was 23.1%. Our finding is similar to a study in Taiwan [10]. A study done in northern Tanzania using the same birth registry reported the Recurrence of PTB of 17% [9]. The difference is due to variations in study outcome, whereby in this study, we limited the analysis to spontaneous preterm birth. In contrast, the former study also included women who were medically induced for delivery. These findings provide critical evidence on the risk of recurrence of preterm birth, hence emphasizing the need for early identification and management, especially during antenatal care visits.
Results from this study also showed that both short and long IPI offered a protective effect against recurrence of SPTB. On the contrary, previous investigators reported a higher risk of adverse pregnancy outcomes such as preterm birth among women with short and long IPI [2,5,9] and the recurrent preterm birth [6,11]. The unusual association between IPI and the Recurrence of SPTB could be due to differences in the characteristics of women contributing to deliveries analysed in this study. As Sanga., et al. [12] also explained, KCMC is a zonal referral hospital, and women delivering here are, for the most part, represent high-risk pregnancies. They further stated that healthcare workers in this level of care are hyper-vigilant and more equipped to address complications that could arise during pregnancy and childbirth, compared to the lower-level facilities, hence reduce the risk of pregnancy complications [12]. Despite these findings, a systematic review emphasized the role of short and long IPI on adverse effects on maternal, perinatal, infant, and child health and identified potential causal mechanisms [13]. Close monitoring of high-risk pregnancies is, therefore, very critical at all levels of care.
Antenatal care is a critical opportunity where skilled health care professionals can early identify women at risk of experiencing pregnancy complications and so receive an appropriate care. In this study, we found that inadequate (< 4) ANC visits significantly increased the risk of recurrent SPTB in this study contrary to findings from Israel where prenatal care was not associated with recurrent preterm birth [14]. Prenatal care may reduce risk of other adverse pregnancy outcomes even if recurrence cannot be prevented [14]. Efforts should be done to promote quality and utilization of ANC services [15] in Tanzania and across other settings.
KCMC being a referral hospital, there is a possibility of selection bias due to referral as some women with previous complications tend to be referred from the lower-level health facilities. Furthermore, the use of the date of the last menstrual period to calculate gestational age might introduce bias because most women do not remember their last menstrual period. This is likely to overestimate the recurrence of SPTB due to the over-representation of high-risk women.
Only half of the study population had an optimal interpregnancy interval. The recurrence of SPTB is high among women in this study. The short and long IPI were all protective against the risk of recurrent SPTB while inadequate (< 4) ANC visits increased the risk. Interventions to promote optimal interpregnancy interval and close follow-up of women at risk, especially during ANC visits, may reduce the risk of recurrence of preterm birth and associated adverse outcomes.
Ethical clearance certificate was obtained with number 2327 from Tumaini University College Research Ethical Committee prior to the initiation of the study. The study observed the confidentiality and privacy of the subjects were protected. Unique identification numbers were used to identify and link mother and child records. For practical reasons, since the interview was administered just after the woman had given birth, consent was given orally. The midwife-nurse gave every woman oral information about the birth registry, the data needed to be collected from them and the use of the data for research purposes. Then informed consent was sought verbally from every woman. Following the consent, the woman could still opt not to reply to individual questions. Inclusion of the orally conducted interview in the database was conditional on informed consent, which was followed as far as the orally conducted interview was concerned. All consent procedures were approved by the Kilimanjaro Christian Medical Centre ethical committee.
Permission to use the data in this study was made through the Kilimanjaro Christian Medical University College Research and Ethics Review Committee and received an approval number 2344. The authors do not have the legal right to share the data publicly. All data requests can be sent directly to KCMC referral hospital, P. O. Box 3010, Moshi, Tanzania, Email: kcmcadmin@kcmc.ac.tz, or through the corresponding author.
The authors declare that they have no competing interests. All authors read and approved the final manuscript.
Conceptualization of research idea: Sophia Kiwango, Michael Mahande, Pendo Mlay, Innocent B.Mboya. Data curation: Caroline Amour, Innocent B. Mboya, Michael J. Mahande, Kiondo Kiondo. Data analysis: Sophia Kiwango, Caroline Amour, Michael J. Mahande. Investigation: Sophia Kiwango, Pendo Mlay, Michael J. Mahande, Caroline Amour, Innocent B. Mboya, Kiondo Kiondo. Methods: Sophia Kiwango, Pendo Mlay, Michael J. Mahande, Caroline Amour, Innocent B.Mboya, Kiondo S. Kiondo. Drafting-original draft: Sophia Kiwango, PendoMlay, MichaelJ.Mahande, Caroline Amour, Innocent B.Mboya, Kiondo Kiondo. Review and editing: Sophia Kiwango, Michael J. Mahande, Innocent B. Mboya, Caroline Amour, Pendo Mlay, Kiondo Kiondo.
Our sincere gratitude goes to the Ministry of Health and Social Welfare for their financial support to enable completion of this work. Our appreciation goes to the Head of Department of Obstetrics and Gynaecology, consultants, fellow residents, and nurses, KCMUCo, for full support in fulfillment of this work.
This project was self-funded.
Copyright: © 2020 Sophia Kiwango., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.