Khaoula Khemakhem1, Leila Cherif1*, Wiem Kammoun1, Mahmoud Ziraoui1, Khadija Baccouche1, Lobna Zouari2, Hela Ayadi1, Imen Hadjkacem1 and Yosr Moalla1
1Department of Child and Adolescent Psychiatry, Hedi Chaker Hospital, Sfax, Tunisia
2Department of Psychiatry C, Hedi Chaker Hospital, Sfax, Tunisia
*Corresponding Author: Leila Cherif, Department of Child and Adolescent Psychiatry, Hedi Chaker Hospital, Sfax, Tunisia.
Received: June 20, 2020 ; Published: September 29, 2020
Citation: Leila Cherif., et al. “Depression, Anxiety and Related Factors in Tunisian Caregivers of Children with Autism Spectrum Disorders: A Cross Sectional Survey”. Acta Scientific Paediatrics 3.10 (2020):51-57.
Objective: The purpose of this study was to investigate anxiety and depression in caregivers of children with autism spectrum disorders and its related factors.
Methods: The study was performed in the department of child and adolescent psychiatry of Sfax. It included eighty caregivers. The anxiety rating scale of Hamilton and the Hamilton Depression Rating Scale were used to assess mental health variables in these caregivers. The Childhood Autism Rating Scale was used to evaluate the severity of autism spectrum disorder.
Results: More than half of the participants were depressed and anxious. The children of caregivers with depression had significantly lower mean scores of severity of autism than those with normal mood. Depression in caregivers was significantly associated with the female gender. Caregivers were significantly more depressed when their children go to speech therapy. Caregivers were more anxious when their children are males and in the rural areas.
Conclusion: Given the high prevalence of anxiety and depression among caregivers of children with autism spectrum disorder, therapeutic intervention should be considered to alleviate their suffering, taking into account the specific risk factors for each culture.
Keywords: Autism; Caregivers; Depression; Anxiety
ASD: Autistic Spectrum Disorder; CASD: Caregivers of Children with Autistic Spectrum Disorder; HAM-A: Hamilton Anxiety Rating Scale; HDRS: Hamilton Depression Rating Scale; CARS: Childhood Autism Rating Scale
Autistic spectrum disorder (ASD) is a complex and serious neurodevelopmental disorder that can affect many areas of a child’s life. It’s characterized by varying levels of impairment of social communication and interaction, and restricted repetitive patterns of behavior, interest and activity from the early period of life [1].
The prevalence of Autism ASD has increased dramatically in recent decades ranging from 0.19/1000 to 11.6/1000, supporting the claim of an autism epidemic [2]. In Tunisia the prevalence is in the order of 35/10000 [3].
Due to the challenges involved in raising a child with ASD, caregivers of children with ASD (CASD) have been shown to have an elevated risk of experiencing physical health problems and mental health problems, such as stress, anxiety, and depression, compared to caregivers of children with other disabilities or the general population [4,5]. Literature shows that psychological disorders of 15% to 54% of CASD may be marked with symptoms of anxiety [6]. In addition to anxiety, literature shows that CASD exhibit symptoms included under the diagnostic of depressive illness [7-9]. On the other hand, it is now clear that parental mental illness can negatively affect the mental health of children [10,11]. It has also been theorized that parental mental health problems negatively affect adherence to behavioral treatment recommendations for the child with ASD [12]. Therefore, it is important to identify psychological effects in terms of anxiety and depression in caregivers of children with ASD (CASD), in order to present them with adequate care and this to ensure the most of his personal well-being and that of his child.
Although parental mental health has primarily been attributed to the child’s challenging behaviors, few studies have focused on other factors that also impact parental stress or decision-making to use autism services [12].
Besides, while there is abundant literature on psychosocial variables related to ASD in various parts of the world, such undertakings are apparently limited in the Arabian countries [13]. A study cared on Sultanate of Oman shows that all indices of stress, depression, and anxiety were higher in CASD compared to caregivers in the control group [13]. A study done in Egypt shows that it was a highly statistical significant relation between awareness, stress and psychological wellbeing [14]. A study, in Qatar shows that mental health was consistently poorer in CASD [8]. Nevertheless, to our knowledge, no study dealing with this subject has been published in the Tunisian population. Yet, understanding these relationships is essential to implementing interventions to reduce parental psychological stress (anxiety, depression) and make their adaptive strategies more effective. Further, understanding cultural differences becomes no less important in a world with increasing mobility and migration [15] and cultural factors can be crucial to take into account when it comes to effectively implementing parent-educative courses or interventions of any sort. Additionally, culture differences can impact results following assessments and clinical decision making. It is also important that assessment tools are culture sensitive [16].
In Tunisia, even after the 2011 revolution, Tunisian children and youth who represent more than 25% of the population, face many problems such as poverty and lack of access to healthcare and education particularly in unprivileged regions [17]. Even more alarming, children with ASD as well as their families must deal with precarious living conditions and the failures of the welfare and healthcare systems, while also experiencing the decline of traditional forms of social organization [18]. All this suggests that the psychological well-being of CASD in Tunisia is deeply affected.
The present study aimed to estimate the prevalence and the determinants of anxiety and depression in CASD.
A cross-sectional study was carried out on 80 CASD (62 mothers and 18 fathers) who accompanied their children to the child and adolescent psychiatry department at the Hedi Chaker Hospital, in Sfax, either for consultation or for patient care at the day hospital, during the period from September to December 2014.
All parents were informed about the objectives of the study and the procedures to participate. Parents of children with ASD were included in the study. Informed consent was taken from the parents. Data on participating parents were gathered through self-administered questionnaires. Parent questionnaires included items on child, parents, and family characteristics and other issues. Data on variables included the present study were collected though using of parent questionnaires and looking for the medical file. The research was approved by the ethics committee of the medicine university of Sfax.
The anxiety rating scale of Hamilton (HAM-A) [19] and the Hamilton Depression Rating Scale (HDRS) [20] were used to assess mental health variables in CASD. To evaluate the severity of ASD, the Childhood Autism Rating Scale (CARS) was used [21].
The HAM-A includes 14 items, each defined by a series of symptoms, and measures both psychic and somatic anxiety. Each item is scored on a 5-point scale, ranging from 0 = not present to 4 = severe, with a total score range of 0 - 56, where less than 17 indicates mild severity, 18 - 24 mild to moderate severity and 25 - 30 moderate to severe [19].
The first 17 items of the Hamilton Depression Rating Scale were used as part of the psychiatric interview. The HDRS is clinician rated and consists of depressive symptoms which are recorded using 5 or 3-point scales reflecting presence and severity over the past week. Scoring is based on the 17-item scale and scores of 0 - 7 are considered as being normal, 8 - 17 suggest mild depression, 18 - 25 moderate depression and scores over 26 are indicative of severe depression; the maximum score being 52 on the 17-point scale [20].
Autism was evaluated using the Childhood Autism Rating Scale (CARS) [21]. This scale consists of 15 items and rate children from 1 to 4 for various criteria (midpoints are also allowed) with total score ranging from 15 to 60 with a minimum score of 30 is considered as a cutoff for a diagnosis of autism. The test interpretations based on the composite score range from non-autistic to mildly autistic, moderately autistic, or severely autistic.
All assessments were arabised but not validated in Tunisian population.
Data entry and statistical analysis were performed using the SPSS software in its 10th version. For the descriptive study, the qualitative variables were expressed as a percentage, while the quantitative variables were expressed as averages with their standard deviations.
To compare frequencies, Chi-squared test was used. Comparisons of 2 means were made using Student’s t-test. Comparisons of several means were made using the Anova test. Percent comparisons were made by the Pearson chi-square test (χ2). In all statistical tests, the materiality threshold was set at 0.05.
The study included 80 parents who have at least one child diagnosed with ASD. The sample showed predominance of mothers compared to fathers (62 versus 18).
Table 1 shows socio demographic characteristics of parents: average of ages, domicile, educational level, family type, socio-economic status, number of children and employment of mothers.
Table 2 shows distributions of children by age group, sex, birth order, educational status, being or not a single child and severity level of autism. Our sample of children showed that the age average at the first consultation is almost 3 years (range 1.50 - 8.30 with SD = 1.05).
From time of symptom onset to first health care contact, children had an average wait of almost 10 months (range 1 - 48 months with SD = 8.26). At the announcement of diagnosis, the average age of children is 3.54 years (range 2 - 8.25 years with SD = 1.05). Finally, the average wait time for medical care was 7.50 months (range 1 - 24 months with SD = 4.26). Children in this sample received institutional care in 88.8% of cases, medication management in 37.5% of cases and speech therapy in 47.5% of cases.
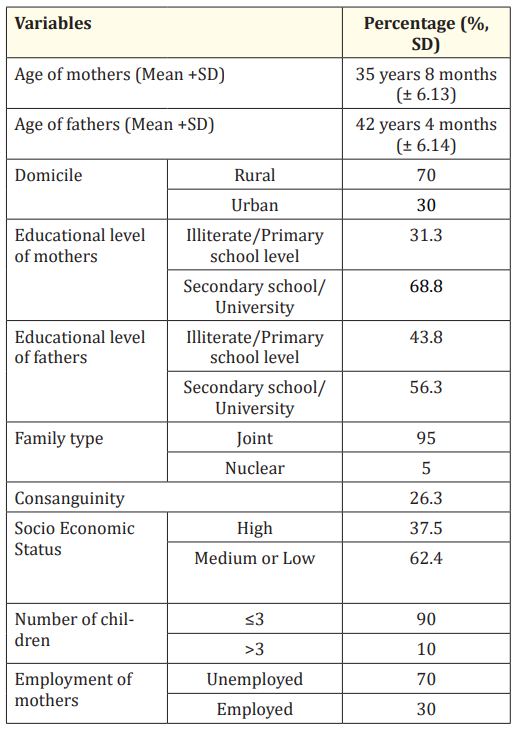
Table 1: Socio demographic characteristics of study population. SD: Standard Deviation.
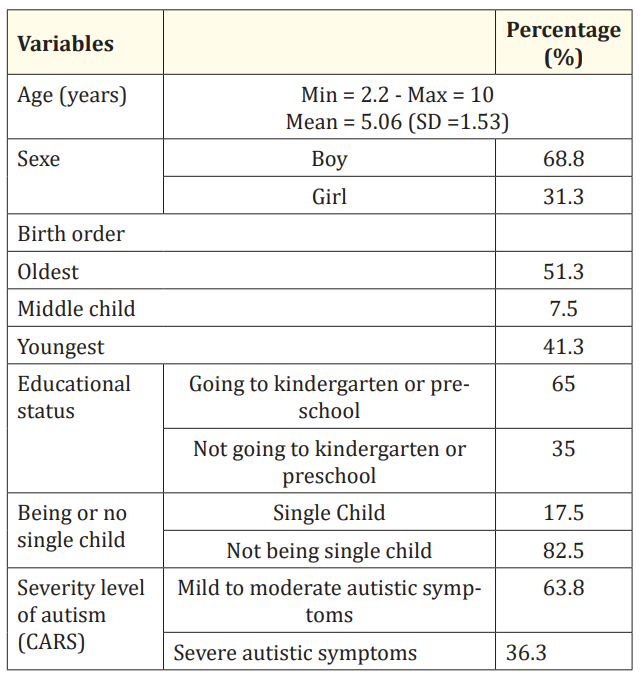
Table 2: Demographic characteristics of children and severity level of autism. CARS: Childhood Autism Rating Scale.
Figure 1 shows the prevalence of anxiety and depression according to level of severity.

Figure 1: The evaluation of depressive and anxiety symptoms and their severity among parents.
The Chi2 test showed that depression was strongly associated with female gender of CASD (94.4% of depression in mothers versus 53.3% in fathers, p = 0.000). CASD were depressive, in 96.6% of cases, when their child go to speech therapy, versus 77.5% when their child do not go the speech therapy (p = 0.037). T test showed that there was a significative association between depression and means of CARS scores. Depressive CASD had their CARS children mean about 38.271 versus 43.00 in normal mood CASD (p = 0.034). There was no significant association between depression, ages of children, mothers and fathers.
Anxiety had significant relationship with male sex of the child. It was noted 30.9% of severe anxiety in CASD when the child is a boy versus 8% when the child is a girl (p = 0.075). CASD from urban area had more anxiety those from rural area (p = 0.034).
There was no significant association between anxiety, severity of ASD, ages of children, mothers and fathers.
No other potential determinants (age, socio economic status, domicile, education level, number of children, birth order) displayed significant associations with depression or anxiety.
The Pearson test demonstrated that parental depression scores were strongly correlated with those of anxiety (p = 0.000, R =
0.811).
Caring for a child with ASD is a challenging situation that may increase the risk of mental health problems among caregivers. Understanding more about these mental health problems may help to provide support programs for CASD and will therefore improve ASD management. Accordingly, the present study aimed to investigate anxiety and depression in CASD and to identify the factors associated with these mental health problems.
More than half of the participants were depressed and anxious. In 2004, Bitsika and Sharpley [22] found, on a sample of CASD in Australia, that approximately 50% of participants were severely anxious and nearly two thirds were clinically depressed. Prevalence figures of anxiety and depression in the standard Tunisian population are inexistent. On a sample of Tunisian hypertensive subjects, with an average age of 61.85 years (±11.95), the prevalence of depression, which was evaluated by the hospital anxiety depression scale, was 44% and that of anxiety 38% [22]. Despite the fact that these people were at risk, given that were aged over 60 and because of high blood pressure, these figures are lower than the ones found in our sample.
Several studies found that autism symptom severity was an important predictor of parental stress [23-25]. According to Machado., et al. severe behavioural symptoms in children were strongly associated with symptoms of anxiety/depression in their parents, with severe symptoms in the child increasing the likelihood of the parents suffering from anxiety/depression by a factor of 35 [26]. A study by Davis and Carter [24] has reported a different finding, concluding that autism symptom severity was not predictive of parental stress.
In this study, contrary to prior studies, the children of CASD with depression have significantly lower mean scores of severity of autism than those with normal mood. This could be explained by several facts. In fact, when autism is mild, school integration is possible and parents are more concerned and then invest more in taking care of their children. Taking in charge autism in our context is limited to few private centres and only one public centre opened in 2018 in the capital of Tunisia. Therefore, parents must organize meetings with different professionals in different localities. They need to travel out of town and they are generally forced to seek places in private centres despite difficult conditions. In front of these constraints, centre’s integration would be significantly impeded and the duration of care would be reduced. Parents are in a position to compensate for this lack by taking in charge their children at home, which is stressful and tiring for the parents. The child state improves after a long exhausting course, which could lead to burnout and depression. In fact, depression in CASD is significantly associated with the female gender. In our cultural context, this finding is attributed to the major role that mothers have historically played in daily care for children with ASD. This is most clearly demonstrated by research showing that mothers of children with autism report more stress and other negative effects than fathers in the same family do [27,28]. Surprisingly, CASD were significantly more depressed when their children go to speech therapy. In fact, speech therapy is indicated when there is an emergence of language in children. In fact, we expect that the development of language in children is a relief for parents however, in Tunisia, access to speech therapy is not easy. In the public sector, appointments are not frequent enough while in the private sector, care is paid but the refund is generally made in partial. This can also be explained by the point of view of Baker., et al. [29] who state that in children with disabilities, parental stress seems to be much more associated with their children’s behavior problems than with their developmental delay. In fact, parents think that the problems and delays in the acquisition of competence are related but independent constructs [24], however, the delay of language is less stressful than language disabilities.
According to the present findings, parents of CASD children are more anxious when their children are males. This might be related to the cultural context where male gender preference is still existent, but also to the high frequency of expressed disorders among boys in the same context [30]. In another cultural context, a study conducted in Brazil showed that when the child with ASD is a girl, the symptoms of anxiety and depression in the parents may be greater, stating that deviant behavior is more acceptable in boys [26].
Nevertheless, in the rural areas, CASD are significantly less anxious. In fact, rural people are more tolerant with the behavioral problems in their children. In the rural areas, the possibilities of care are almost non-existent. Consequently, parents have no possibility to change this situation but they should gradually accept it. However, in the urban areas, care is available but access is difficult either because there are long waiting lists or the number of hours of care is insufficient in the public sector or it is expensive for parents who must pay for it, which causes some concerns and anxiety among these parents [11].
This study did not include a control group, which limits the validity of the results. It is limited by small sample size. In addition, the sample of the present study is recruited from the department of child and adolescent psychiatry that provides services to children with ASD, resulting in sampling bias, as the parents of these children are already seeking support.
Our study suggest that the diagnostic of autism in children has repercussions on parents with important prevalence of anxiety and depression. Female CASD were found to be more depressed while caregivers of male children with ASD, coming from urban areas were found to be more anxious. Thus, lower severity of autism and undergoing a speech therapy were significantly associated to depression in CASD.
A therapeutic intervention targeting specific high risk-groups of CASD is highly recommended in order to alleviate their suffering while taking care of their autistic children to ensure optimum results for both caregivers and children. More attention should be paid to symptoms of depression and anxiety to female CASD when accompanying their children in consultation, even in mild and moderate forms of ASD, and although follow-up and health care for the child with ASD has already been started.
Thanks are due to all parents of children patients with autism who participated in this study.
Copyright: © 2020 Leila Cherif., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.