Lotha B1*, Bergonzani M2 and Zeinalddin M3
1Craniofacial Cleft Surgeon, Yemen Global Smiles, Sanaa, Yemen
2MD, Maxillo-Facial Surgery Division, Parma University Hospital, Italy
3Craniofacial Orthodontist Mohammad Orthodontic Center - Senior Lecturer Oman Dental College, Oman
*Corresponding Author: Lotha B, Craniofacial Surgery Fellowship, Yemen Global Smiles, Sanaa, Yemen.
Received: July 24, 2020; Published: August 18, 2020
Citation: Lotha B., et al. “Learning to Crack the Cleft Aesthetic Code in Unilateral Cleft Lip Surgery by Younger Cleft Trainees: Using Nuances and the Innovative Taipei Pear Analogy for Inferior Turbinate-flap Floor of Nose Reconstruction”. Acta Scientific Paediatrics 3.9 (2020):10-16.
Unilateral cleft lip surgery is part and parcel of every trainee cleft surgeon’s armamentarium. As their cleft expertise is founded on solid principles and anthropometric measurements, the chances of error and iatrogenic deformity are significantly lower than that of the untrained surgeon who attempts cleft surgery. In this communication we would like to mention the possible dimensions of cleft surgery, and how one can improve outcomes by looking at different ways to ease the psychological burden of cleft children. The sequential repair makes for better aesthetic functional results and patients will be satisfied with the post-operative results when the surgery is properly executed, taking into consideration all the rules of engagement in tackling cleft challenges.
Keywords: Cleft Lip; Inferior Turbinate Flap; Median Tubercle; Cleft Training
Unilateral cleft lip surgery is the commonest procedure performed at all smile centres across developing world smile centres. Every cleft surgeon starts with repair of the unilateral cleft lip before moving on to other more advanced surgeries. Accuracy of repair is always a concern and proper training is the need of the hour [1].
It is not so much about comparisons or picture perfect results, but using correct principles as a launching pad for future improvements even as younger cleft surgery trainees start their careers as primary cleft surgeons.
At the outset, it cannot be stressed enough that anthropometric measurements are absolutely essential for every cleft trainee. As advised by our dear mentor John Mulliken of Childrens MA, we make sure trainees everywhere are familiar with the measurements and also practice the speciality at home before embarking on overseas missions [2]. Earlier this season, John had shared with us that the typical cleft lip repair of an untrained surgeon manifests itself as a poorly understood and badly executed repair.
Getting it right the first time would serve as the perfect launching pad for any cleft service as primary unilateral cleft surgery is the first test of a surgeon’s skill at clefts. Failure to launch will inevitably lead to iatrogenic deformities where one deformity is replaced by another, as the unenviable process of serial expertise continues due to poor understanding of the basic principles [3].
Since the majority of the world’s population with clefts live in developing countries, the need of the hour is to market the AARaffordable, applicable and reproducible, take-home message for all who follow this sub speciality with a passion for underprivileged cleft populations.
One of the key strategies in understanding the anatomy of change in unilateral cleft lip surgery, lies in a good knowledge of the orbicularis oris muscle-dermis complex [4]. Our focus is on the perfect simulation of a normal muscle dermis complex with the usual add-ons that, arguably create more happiness for our patients over the years.
We would like to propose five possible dimensions in unilateral cleft lip surgery. In poor countries with sparse resources, the 1st to 5th Dimension of cleft care is more or less a 1st to 5th Illusion of cleft care, as all of us are sadly aware. The first and second dimension are part and parcel of what we would term “Functional and Aesthetic Correction” during primary the cleft lip surgery in welldeveloped units, where the plastic surgeon is well versed with the different aspects of the procedure and is not trying to divide the two into separate entities.
The First dimension- reconstructive element which corrects the functional aspects and leads to proper function of repaired the cleft lip; this is what is so commonly encountered in developing world smile missions where this aspect alone is addressed without the equally important second step.
The Second dimension includes the small z and cheiloplasty procedures with Tajima primary rhinoplasty [5], which are aesthetic in nature, thereby adding an attractive aesthetic appearance after the correction; the usual aesthetic lip repairs in well-developed units.
The others are ancillary procedures involving scar modulation, gleaned from the interphase between Aesthetic Medicine and Plastic Surgery.
The Third dimension is offered by Aesthetic Medicine where the accidental discovery of “Aesthetic Botox” became a game changer for millions of aesthetic procedures [6]. It makes the aesthetic appearance even more attractive and supple by controlled muscle relaxation and improved scar outcomes.
The Fourth dimension includes Aesthetic Medicine enhancement procedures using Aesthetic Medicine in stepwise progression, using autologous fat filler to improve scar appearance [7], skin tone and volume correction.
The Fifth dimension involves the use of advanced lasers including nano second, fractional or picosecond lasers [8]. Combined with the fourth dimension, the overall results will be enhanced even further. There is an overlap between four and five, because a combined approach may be even more beneficial.
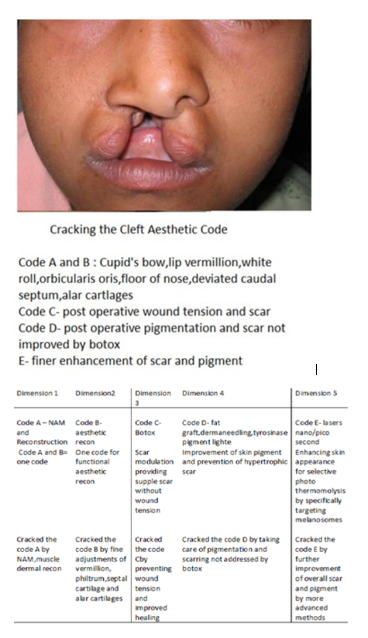
Figure 1: Cracking the cleft aesthetic code (Courtesy L Bona 2020).
For the purpose of simplicity, one can try to make this a user friendly code by using the analogy of a continuous “skin of the pear”, a concept designed in Taipei during a casual discussion of the inferior turbinate flap [10]. Since we use the lateral L flap in nasal floor reconstruction, the concept uses AI (augmented imagination) and imagines that the mucosal and vestibular surfaces are like the skin of a pear; this is true for the continuous inferior turbinate surface facing the nasal cavity (Figure 2,3).
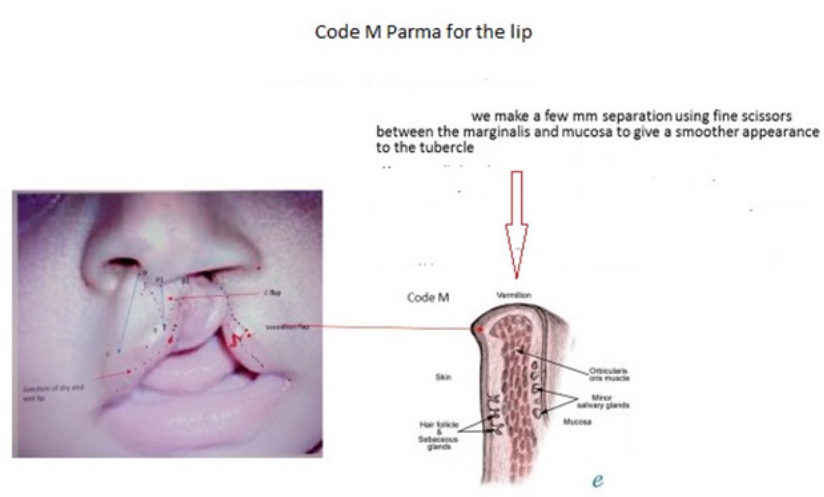
Figure 2: Code M Parma for the lip (courtesy Bergonzani M, Parma).
Figure 3: Analogy of the Taipei slinky S pear incision and its progressions (courtesy L Bona).
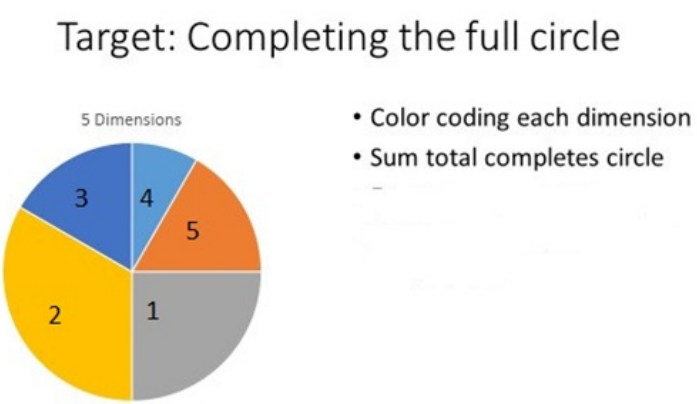
Figure 4
Muscle closure: CINCH SUTURE FIRST. The first stitch to be tied is the cinch suture which has to be tied, with slight over correction. We use internal and nor external cinching sutures:
For easy sequencing, we perform the 5th internal cinching suture first, followed by 1 to 4. We prefer to use our innovative “skin hook” rule by downward traction to suture at equal distances without discrepancy. This ensures symmetrical closure of muscle and skin flaps.
Next, we perform the Tajima rim incision with slight over correction of 1mm on the cleft side ala. Releasing the domes adequately, we then transfix with the cleft dome by an inverted U suture using 4 0 nylon, where the cleft cartilage is kept 1 mm higher. Not every cleft surgeon is familiar with this technique and may use other methods or repair the nose later (older sample pics). Post operatively, a nasal conformer is inserted, with one side 1 mm higher. This is kept for 6 months to reshape the hypoplastic alar cartilage. We also tape the lip edges every 2 to 3 days with 3M tape, without involving the cheeks for 6 months.
Observing the rules of engagement in cleft lip repair, the challenges are managed quite well using the anthropometric measurements and proper sequencing. The step-wise progression is very useful in getting a symmetric lip repair without deformity. The corresponding author’s results have been consistently uniform using these methods on many cleft children during mission outreach with the US Smile Train humanitarian programmes in Yemen and elsewhere.
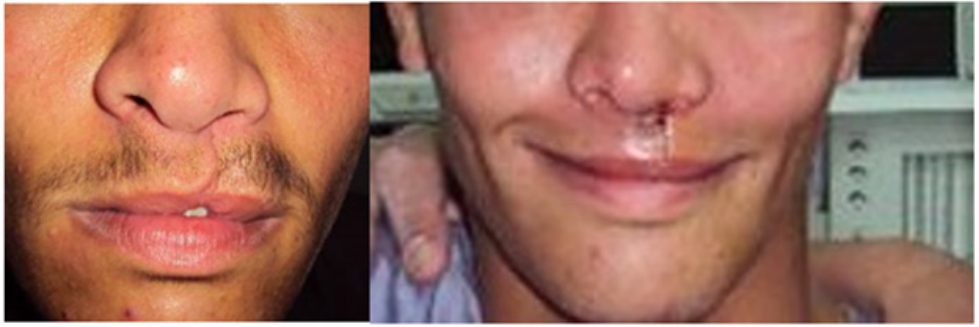
Pic samples: Smile Train NYC and Yemen Global Smiles outreach pics 2010 - 2015 (from smile mission database) (Courtesy L Bona).

Picture 1: Left cleft lip (Tajima not done).

Picture 2: Left Cleft Lip (Tajima not done).

Picture 3: Left cleft lip (Tajima not done).
Picture 4: Microform left cleft lip.

Picture 5: Left cleft lip.
Cracking the cleft aesthetic code is easy to learn by cleft trainees because the anatomical landmarks remain constant for every case. The results will not always be picture perfect because no two deformities are the same. Our aim is not to create a flawless designer lip, but show younger cleft surgeons the importance of anthropometric measurements and the principles of accurate lip repair by our long time mentor John Mulliken. Getting it reasonably good the first time round makes subsequent repairs a lot easier to manage. We hope this brief communication will be of help to trainee cleft surgeons even as they embark upon smile missions to lessen the burden of cleft children across the world.
Copyright: © 2020 Lotha B., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.