Leonid Ovcharenko*, Denis Sheludko, Andrii Vertehel, Igor Samokhin, Tetiana Andrienko and Oleksandr Kryazhev
State Institution “Zaporizhia Medical Academy of Post-Graduate Education Ministry of Health of Ukraine”, Zaporizhia, Ukraine
*Corresponding Author: Leonid Ovcharenko, State Institution “Zaporizhia Medical Academy of Post-Graduate Education Ministry of Health of Ukraine”, Zaporizhia, Ukraine.
Received: May 13, 2020; Published: June 16, 2020
Citation: Leonid Ovcharenko., et al. “The Neuroautonomic Regulation Dynamic in Children with Recurrent Upper Respiratory Tract Infection and Decreased Myocardial Functional Reserve after New Rehabilitation Program ”. Acta Scientific Paediatrics 3.7 (2020):39-45.
The results of rehabilitation program 1 month use in 30 schoolchildren aged 6 - 9 years with recurrent upper respiratory tract infection (URTI) and a decreased myocardial functional reserve were analyzed. We studied the dynamics of changes of the initial vegetative tone (IVT) status and the indicator of activity regulatory systems (AIRS), as well as the concentration levels of neurotransmitters in the blood serum (substance P, vasoactive intestinal peptide (VIP) and final stable metabolites of NO (FSM NO)). The data were obtained that in children after the rehabilitation program, significant differences were found in the improvement of the IVT and AIRS indicators, as well as in the dynamics of changes in the concentration of neurotransmitters in blood serum. Convincing data were obtained that, when positive dynamics were obtained in changes in the serum concentration of neurotransmitters, positive shifts were noted in the indicators of IVT and AIRS in primary school children. The result of the rehabilitation program was a positive trend in the indicators obtained after the Ruffier test.
Keywords: Children; Myocardial Functional Reserve; Recurrent URTI; Ruffier Test; Neurotransmitters
With the beginning of the schooling period in children, contact with respiratory pathogens significantly expands, and psychoemotional stress increases as a result of an intensive school program, which increases the load on neuro-immune homeostasis, and negatively affects the frequency and course of respiratory tract diseases [5,13]. Among children of primary school age, only 12.6% can be considered healthy and after graduation, this figure decreases to 4.3%, on average 2.5 diseases per child [2]. Only 30% of school-age children can fulfill physical standards without risk to health. The level of low physical activity of schoolchildren can lead to the formation of cardiovascular (CVS) pathology [2,7]. According to studies, children of primary school age have unsatisfactory functional fitness for physical activity with insufficient training and a low level of functional reserve of the cardiovascular system [2,8]. An alarming fact is the increase in the number of children with be havioral and mental disorders. More than 58% of children show mental fatigue, anxiety in 49.3% and stress reactions in 69.8% [9].
An increase in the frequency of respiratory tract diseases, complications of school education programs, violation of regimen moments, prolonged use of electronic devices (ED) throughout the day can change the functional state of the autonomic nervous system (ANS), cause physical inactivity and form increased general school anxiety, which ultimately manifested by a violation of the functional reserve of the myocardial. The complex of medical and social problems dictates the need for therapeutic and rehabilitation measures during the vacation period. In this regard, the quality improvement of school-age children is an important and urgent public health task, which is given special attention by the medical community. Preserving and strengthening the health of the younger generation is a strategic task of the state and summer vacations seem to be a seasonal opportunity to gather strength before the next school year [3,11].
To estimate of new rehabilitation program efficacy in children with recurrent URTI and decrease of the myocardial functional reserve.
An analysis of the results of the wellness program for children with recurrent URTI and a decreased of the myocardial functional reserve is carried out. 30 children were examined. Inclusion criteria were: the age of the children - 6 - 9 years, the sex of the child (boys and girls), the presence of a recurrent pathology of the respiratory tract (children with acute respiratory diseases 6 times a year or more [4,10]), reduced myocardial functional reserve (Ruffier test indices 7 and more points [12]). All children were initially assessed for neuroautonomic regulation. During the 1st month, treatment and rehabilitation measures were carried out, which included: daily routine: departure for nighttime sleep at 21:00, restriction of ED to 1 hour per day, sanitation of foci of infection (otolaryngologist to indications), walks in the open air, at least 2 hours a day. Medications: nootropics (piracetam) - 50 mg/kg per day in 2 divided doses, sedatives (am. To-glycine) - 100 mg 2 times a day, vitamins (L-carnitine, vit. B1, B6, B12) - 1 caps. 2 times a day, membrane stabilizer (polyunsaturated fatty acids) - 1 caps. - 1 time per day.
Examination methods: To study the functional state of the autonomic nervous system (ANS), we used the method of analyzing heart rate variability (HRV) using the Cardiolab electrocardiographic complex (Cardiolab SE TU U 33.1-02066769-0022002 manufactured by the National Aerospace University named after M.E. Zhukovsky “Kharkov Aviation Institute”). The state of HRV was analyzed: cardiointervalogram (CIG) data: mRR, MxDMn, SDNN, RMSSD, pNN50%, AMo, SI and spectral analysis: TP, VLF, LF, HF, LF/HF, IC, regulatory activity indicators systems (AIRS). Normal PARS - 1 - 3 points, impaired AIRS - 4 - 10 points, failure to adapt regulatory systems - 8 - 10 points. The indicators of serum concentrations of neuropeptides were studied: vasoactive intestinal peptide (VIP), substance P and biologically active substance - nitric oxide (NO) in the final stable metabolites of NO (FSM NO). The plasma content of the final stable metabolites of nitric oxide (nitrates, nitrites) was carried out by reducing nitrates to nitrites with the determination of the latter by reaction with Gris reagent. The optical length was measured on a spectrophotometer with a wavelength of 540 nm. Calculation of the amount of nitrite was carried out on a calibration graph built on nitrogen [15]. Quantitative determination of substance P and VIP in blood serum was carried out by enzyme-linked immunosorbent assay on a SUNRISE photometer analyzer (“TECAN” Austria) using ELISA test systems “Substance P” and “Vasoactive Intestinal Peptide” manufactured by Peninsula Laboratories, LLC (San Carlos), USA.
The study used statistical methods for processing the obtained information: Fisher angular test, mean (M), average error (m), Student t-test, error curves (ROC curve - receiver operating characteristic curve) were constructed with cut-off point calculation point) and the area under curve (AUK - area under curve).
The study was conducted in accordance with the ethical principles of the People’s Medical Research adopted by the Helsinki Declaration and the Good Clinical Practice (GCP).
In the course of the work, the state of the ANS and AIRS in children of observation groups was studied. When analyzing HRV, indicators with the highest informational entropy were taken into account. The data are presented in figure 1A-1C.
As a result of the impact of the rehabilitation program measures on the CIG data, in most indicators (SI, SDNN, RMSSD, pNN50%) in children with recurrent URTI and a reduced myocardial functional reserve, statistically significant differences were determined according to the confidence intervals (See figure 1A-1С). However, in an indicator such as mRR at confidence intervals, there was no statistically significant difference in children with recurrent URTI and reduced myocardial functional reserve before and after rehabilitation. Based on the Mann-Whitney criterion, it was found that in children with recurrent URTI and a reduced functional reserve of the myocardial against the background of the rehabilitation program, there is a tendency to increase the average duration of RR intervals, indicating a decrease in heart rate (HR) in children (U = 285.5; p < 0.05). As confirmed by the ROC analysis (Figure 2).
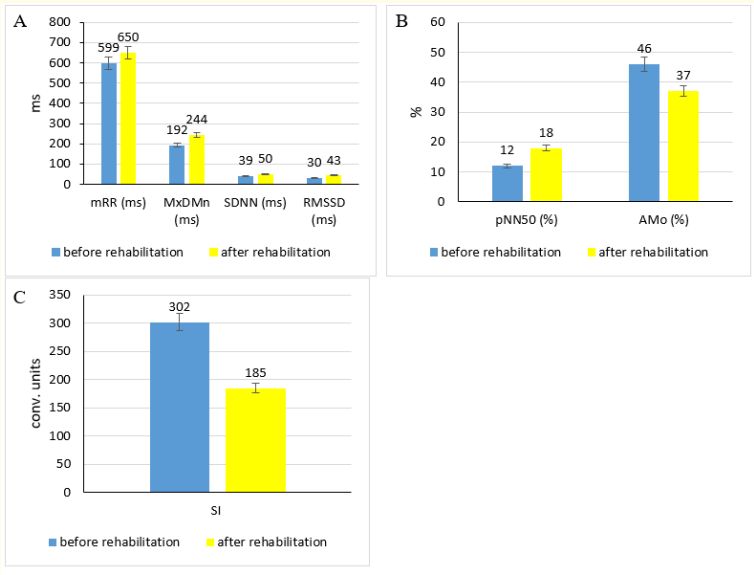
Figure 1: Comparative analysis of CIG indicators: mRR, MxDMn, SDNN, RMSSD (A), pNN50%, AMo (B), SI (C); ms: Milliseconds; conv. units: Conventional Units.
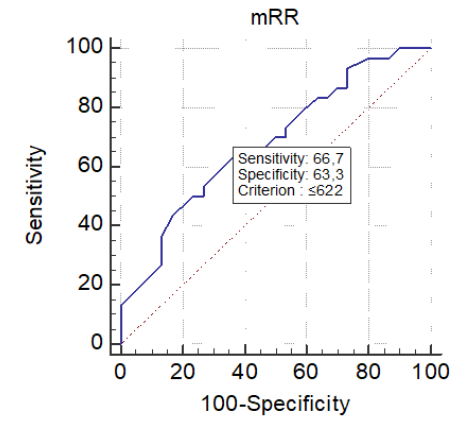
Figure 2: The cut-off value for the mRR indicator after the rehabilitation program.
The analysis of ROC curves after rehabilitation for children with recurrent URTI and reduced functional reserve of the myocardial found that the cut-off point is mRR of 622 ms. Values below this indicator in children with recurrent URTI will be associated with an increased risk of sympathetic activation with a YDN of 0.3 which corresponds to sensitivity of 66.7% and specificity of 63.3%, and AUC of 0.7.
When analyzing the results of the impact of the rehabilitation program in children with recurrent URTI and a decreased functional reserve of the myocardial on the spectral analysis data (TP, VLF, LF, HF, LF/HF, IC) and AIRS, statistically significant differences were found according to the confidence intervals, which indicates improving the functioning of the ANS (See figure 3A and 3B).
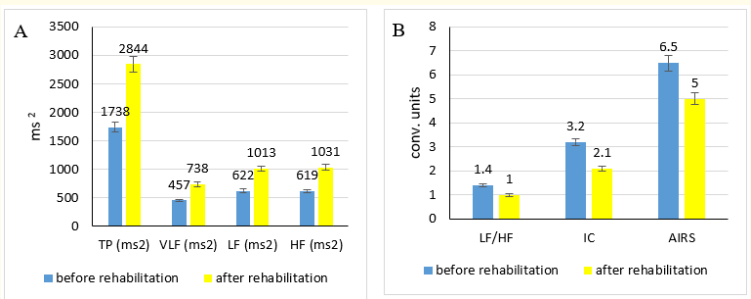
Figure 3: Comparative analysis of the spectral analysis indicators TP, VLF, LF, HF (A), LF/HF, IC, AIRS (B); ms2 : Milliseconds; conv. units: Conventional Units.
After a comprehensive rehabilitation in children with recurrent URTI and a decreased functional reserve of the myocardial, AIRS was analyzed. The data are shown in figure 4.
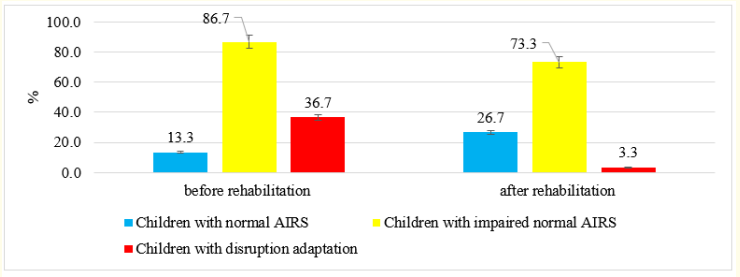
Figure 4: Dynamics of the activity indicator of regulatory systems after a rehabilitation program. Notes: *: p < 0.01 when compared with the results before and after rehabilitation.
A comparative analysis of the results of rehabilitation in schoolchildren with recurrent URTI and a decreased functional reserve of the myocardial showed that the number of children with impaired AIRS decreased by 13.4% (p> 0.05). The failure of adaptation processes decreased by 11 times (p < 0.01), which indicates a decrease in the level of tension in the regulatory systems of the child’s body.
After the rehabilitation course, the interaction of HRV and AIRS was evaluated. The data are presented in table 1.
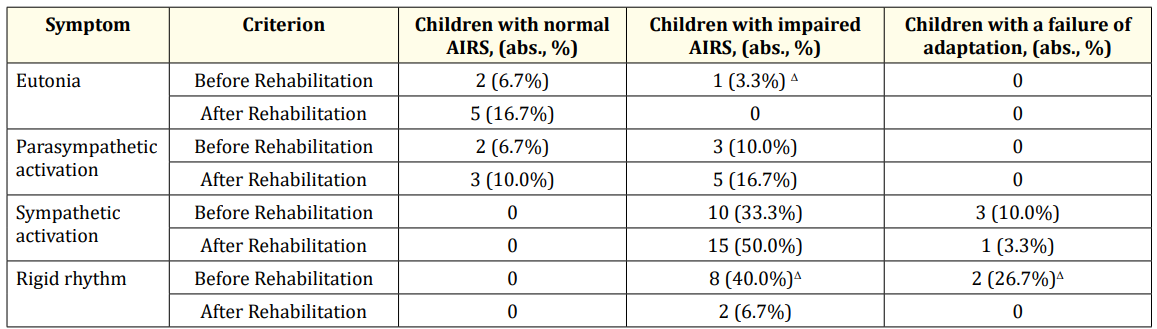
Table 1: Interrelation of HRV and AIRS indicators before and after the rehabilitation program. Notes: Δ: p < 0.05 when compared with the results before and after rehabilitation.
After the rehabilitation period in children with recurrent URTI and a decreased functional reserve of the myocardial with the presence of eutonia, normal AIRS indicators were detected 10.0% more often (p > 0.05). No violations of AIRS were detected (p < 0.05). Among children in whom predominated parasympathetic activation, normal AIRS indicators were more often recorded, and AIRS disorders were detected only 6.7% more often (p > 0.05). Among children in whom sympathetic activation predominated, AIRS disorders were detected more often by 16.7% and the presence of a failure of adaptation after rehabilitation in children with sympathetic activation decreased by 6.7% (p > 0.05). Among children with a rigid rhythm, registration of impaired AIRS decreased after rehabilitation by 5.9 times and amounted to 6.7% (p < 0.05). Disruptions in adaptation processes were not detected (p < 0.05). In total, the violation of AIRS in children with sympathetic activation and a rigid rhythm decreased by 16.6% (p > 0.05). The number of identified cases of adaptation failure in children with sympathetic activation and a rigid rhythm after the measures decreased by 11 times (p < 0.01).
A marked change in the levels of concentration in the blood serum of neurotransmitters (substance P, VIP and FSM NO) in primary school students with recurrent URTI and a decreased functional reserve of the myocardial. The data are presented in table 2.
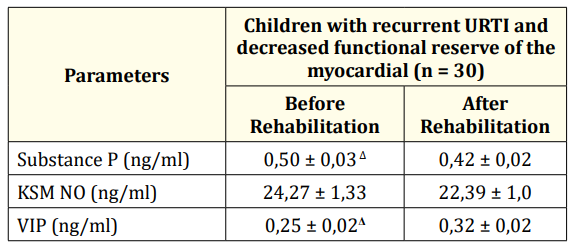
Table 2: Indicators of the level of concentration in the blood serum of neurotransmitters in children during the period of somatic well-being before and after the rehabilitation program (M ± m). Note: Δ: p < 0.05 - when comparing with the results before and after the rehabilitation program.
After the rehabilitation program, a statistically significant decrease in the serum concentration of substance P was revealed in children with recurrent URTI and a decreased functional reserve of the myocardial (p < 0.05).
In the indicators of serum concentration of FSM NO in children with recurrent URTI and a reduced functional reserve of the myocardial after the rehabilitation program, no statistical difference was found (p > 0.05). Based on the data of the Mann-Whitney test, a significant difference between the indicators before and after the rehabilitation program (U = 254.5; p < 0.05) was revealed. Which is also confirmed by the ROC analysis of figure 5.
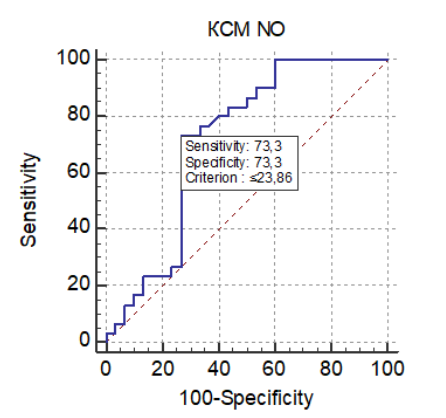
Figure 5: The value of the cut-off point for the FSM NO indicator after the rehabilitation program.
The ROC curve data for children with recurrent URTI and a reduced functional reserve of the myocardial showed that the cut-off point is the value of FSM NO 23.86 ng/ml A value higher than this indicator will be associated with an increased risk of sympathetic activation with a YDN of 0.47 which corresponds to a sensitivity of 73.3% and specificity of 73.3%, AUC of 0.72.
During the course of rehabilitation therapy, indicators of the relationship of the levels of neurotransmitters with HRV and AIRS in children with recurrent URTI and a decreased functional reserve of the myocardial underwent changes. The data are presented in table 3.
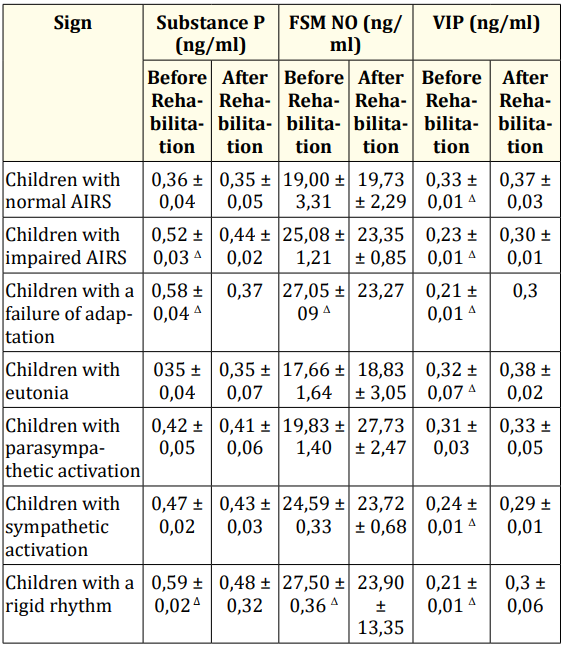
Table 3: Indicators of the concentration of substance P, FSM NO and VIP in children before and after the rehabilitation program. Note: Δ: p < 0.05 - when comparing with the results before and after the rehabilitation program.
The results showed that the relationship between the indicators of serum concentration of substance P in children with recurrent URTI and a decreased myocardial functional reserve before and after the rehabilitation program has changed. A statistically significant decrease in the concentration level of substance P was observed in children with impaired AIRS, disruption of adaptation processes, rigid rhythm (p < 0.05).
Indicators of the concentration of FSM NO in children with recurrent URTI and a decreased functional reserve of the myocardial before and after the rehabilitation program revealed a statistically significant decrease in the level of concentration of FSM NO in children with a disruption in adaptation processes and a rigid rhythm (p < 0.05).
The dynamics of the level of VIP concentration in serum in children with recurrent URTI and a decreased myocardial functional reserve before and after the rehabilitation program established a statistically significant increase in the concentration of VIP in children with normal AIRS and impaired AIRS, disruption of adaptation processes, eutonia, sympathetic activation, rigid rhythm (p < 0.05).
The functional reserve of the myocardial was determined on the basis of the Ruffier test in children with recurrent URTI of the respiratory tract at the beginning and at the end of the school year, as well as after a rehabilitation course.
Figure 6 presents the data obtained from the results of the Ruffier test.
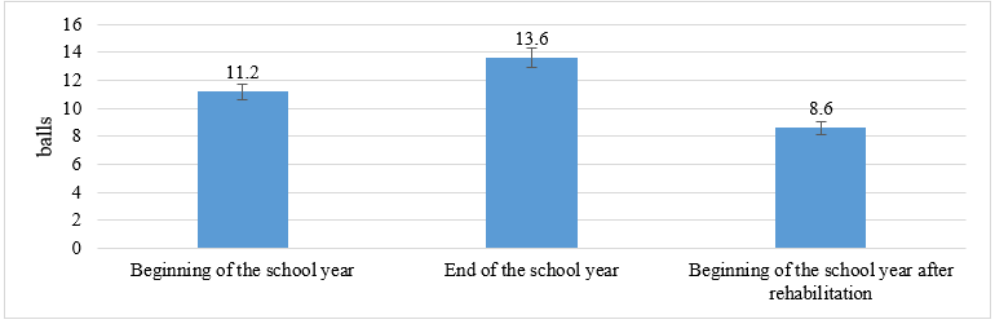
Figure 6: Ruffier sample performance data for the school year.
Analyzing the data obtained, after conducting a rehabilitation program in children with recurrent URTI and a reduced functional reserve of the myocardial, a statistically significant difference was established in confidence intervals in the average Ruffier test at the beginning and end of the school year, as well as at the beginning of the school year without a rehabilitation program and after a rehabilitation programs (p < 0.05). When analyzing the dynamics of changes in indicators in children with recurrent URTI and a decreased functional reserve of the myocardial before and after the rehabilitation program, the Ruffier test index improved by 4 points compared to the baseline.
In the course of the rehabilitation program, children with recurrent URTI and a decreased functional reserve of the myocardial established a positive dynamics of CIG indices, characterized by a decrease in the overvoltage of the sympathetic division of the NS manifesting itself in an increase in such indicators as MxDMn, SDNN, RMSSD, pNN50% and a decrease in SI and AMo% compared to data before rehabilitation measures.
After a comprehensive rehabilitation program and its influence on the state of the spectral analysis indicators in children with recurrent URTI and a decreased functional reserve of the myocardial, it is noteworthy that after rehabilitation positive dynamics are recorded, characterized by an increase in such indicators as TP, VLF, LF, HF and a decrease LF/HF, SI and AIRS, which characterizes the decrease in the likelihood of a rigid rhythm and overvoltage of the sympathetic division of the NS.
The number of cases of impaired AIRS, as well as disruption of adaptation processes in children with rigid rhythm, significantly decreased, which led to a redistribution of recorded parameters towards normal AIRS and impaired AIRS in children against the background of eutonia, parasympathetic activation and sympathetic activation. In children with sympathetic activation, there is a significant decrease in the registration of disruption of adaptation processes and their complete absence in children against the background of rigid rhythm (p < 0.05). In the literature available for analysis, we did not find such studies.
After the rehabilitation program, the number of children with impaired AIRS decreased by 13.4% (p > 0.05). Disruption of adaptation processes decreased by 11 times (p < 0.05).
When analyzing the indices of neurotransmitters in blood serum in children with recurrent URTI and a decreased functional reserve of the myocardial, a statistically significant increase in the serum concentration of the substance P in children is revealed in the presence of impaired AIRS, disruption of adaptation processes and the presence of rigid rhythm. The data obtained by us are similar to the data of Karimov M.K.K. (2016), where the author received a significant increase in the concentration of substance P in children with respiratory pathology as the severity of diseases in children [11]. As well as a positive result of the rehabilitation measures, an increase in the serum concentration of the VIP neurotransmitter is considered when children are diagnosed with similar conditions, with impaired AIRS, disruption of adaptation processes, sympathetic activation, and with a rigid rhythm (p < 0.05). The concentration of serum levels of FSM NO showed a statistically significant decrease in children against the background of disruption of adaptation processes and a rigid rhythm after the rehabilitation program (p < 0.05).
The functional reserve of the myocardial after the rehabilitation program was characterized by positive dynamics - the average Ruffier test at the beginning of the school year after rehabilitation (8.6 points) improved by 5 points compared with the figure at the end of the school year before rehabilitation (13.6 points).
Copyright: © 2020 Leonid Ovcharenko., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.