Lucas Esuh Esong1,2,4*, Essome Henri2,3, Ida Calixte2,3, Kuate Calixte2,5 and Nehama Linder1,4
1Department of Neonatology, The Helen Schneider Hospital for Women, Rabin Medical Center, Petach Tikva, Israel
2Department of Maternal and Child Health, Laquintinie Hospital Douala, Cameroon
3Faculty of Medicine and pharmaceutical sciences, University of Douala, Cameroon
4Sackler School of Medicine, Tel Aviv University, Tel Aviv, Israel
5Faculty of Medicines and Biomedical Sciences, University of Yaounde I, Yaounde Cameroon
*Corresponding Author: Lucas Esuh Esong, Department of Neonatology, The Helen Schneider Hospital for Women, Rabin Medical Center, Petach Tikva, Israel.
Received: February 18, 2020; Published: May 07, 2020
Citation: Lucas EsuhEsong., et al. “Is Attention Deficit/Hyperactivity Disorder (ADHD) Influenced by Breastfeeding and/or Duration of Maternity Leave?”. Acta Scientific Paediatrics 3.6 (2020):05-10.
Objective: Attention deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder with a risk factor for a broad range of negative outcomes, and therefore places a high financial burden on the healthcare system, families and society. Breastfeeding has been found to be a reducing factor of ADHD. The intended duration of breastfeeding has been found to be a strong predictor. Early return to work after birth has been associated with a shorter duration of breastfeeding and poor maternal-infant bonding. Our objective is to find out if maternal post-delivery leave policies in various countries has significant impact on breastfeeding duration and the incidence of ADHD.
Methods: A systematic search of the medical literature using medline, pubmed, Cochrane review, google scholar and embase in which the largest available study for each country in each category (ADHD, breastfeeding and maternal leave) between 1989 to 2015 was selected.
Spearman Ranks correlation analysis was used to analyze the association between ADHD prevalence, length of paid maternity leave, initiation of breastfeeding, and breastfeeding for 6 six months or more.
Results: A negative correlation between duration of paid leave and ADHD prevalence (Rs -0.54, p < 0.05) and between initiation of breastfeeding and ADHD prevalence (Rs -0.57, p < 0.05). There was also a positive correlation between duration of paid leave and breastfeeding-ever (Rs = 0.4, p < 0.05), i.e. the longer the paid leave duration, the longer the duration of proper breastfeeding.
Conclusion: Paid maternity leave has a very strong negative association with ADHD. Therefore, providing mothers with sufficient paid maternity leave leads to proper breastfeeding within a long period of time and thus reducing the incidence of ADHD.
Keywords: Attention Deficit/Hyperactivity Disorder; Breastfeeding; Maternity Leave
Attention-deficit/hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder of childhood, affecting 3.4 - 7.2% of children and adolescents worldwide [1,2]. Clinical and basic research studies, from genes to higher order neural networks, support a strong genetic contribution for ADHD [3]. Nevertheless, environmental factors are known to have an important role in ADHD etiology, maybe through epigenetic or other mechanisms [3,4]. ADHD has lifelong consequences, associated with a range of adverse short and long term outcomes including higher rates of injury [5], teen pregnancies [6], increased numbers of vehicle accidents [7], poor educational outcomes [8], as well as risk of substance abuse [9], criminal activity [10], decrease in workplace effectiveness [11] and other mental disorders [12] as adults.
Because ADHD might be rooted in altered neural development, early experiences supporting neural development such as breastfeeding are of particular interest [13].
Breastfeeding is promoted internationally as the preferred method of feeding for infants [14]. Among the factors related to the success of breastfeeding are maternal age and level of education [15,16]. The intended duration of breastfeeding has been found to be a strong predictor of the actual duration of breastfeeding and of initiation of breastfeeding [15,16]. Maternal breastfeeding selfefficacy is also a strong predictor of breastfeeding duration, and studies have shown that the integration of strategies to improve self-efficacy would help clinicians increase the quality of care while boosting the confidence of new mothers in their breastfeeding skills [15-17].
At the same time, being employed and early return to work after giving birth have been associated with a shorter duration of breastfeeding and poor maternal-infant attachment. This finding suggests that more flexible working conditions and more generous maternity leave would help women stay home longer with their infants and prolong the duration of breastfeeding [16]. Studies in Scotland and the United Kingdom recommended that health and employment policies be better coordinated to provide working mothers with adequate support to meet the conflicting demands of employment and motherhood [18,19].
Targeting attention processes early can bring about fundamental alterations in the pathogenesis of ADHD, and thus prevent or moderate the course of the disorder [13,19]. There are clear evidences of the sustained, positive effects from early intervention on long-term behavioral outcomes in high risk groups [19,20]. In the case of ADHD, early intervention approach may provide ways in which multiple risk and protective factors transact to impact ADHD development [19-21]. Moreover, since ADHD by itself is conceived as a broad risk factor for a range of negative outcomes (i.e. comorbid behaviors), then these co-morbidities might also be affected or modified [20-22].
ADHD places a high financial burden not only on the healthcare system but also on families and society as a whole [23]. In the United States, analyses based on diagnostic and medical procedure codes estimate the annual cost of this disorder at approximately $1,500 per patient, for a total of about $42.5 billion [24]. Due to these reasons, for the first time the Global Burden of Disease Study 2010 (GBD 2010) has included ADHD in its scope [25]. Better understanding of the epidemiological aspects of the disorder would provide insight into its distribution, etiology, and risk factors and might help health and government authorities allocate mental health services more effectively [23-25].
While there has been substantial focus on perinatal and delivery problems in ADHD [26,27] early postnatal correlates are less well studied [13]. Epidemiological analysis regarding ADHD prevalence identified that study location was associated with heterogeneity especially when estimates from Africa and the Middle East were compared with estimates from North America and Europe. Perhaps the best-studied early postnatal influence, aside from socialization itself, is initiation and duration of breastfeeding [2,13].
A number of articles have reported that a longer duration of breastfeeding may be related to a lower risk of ADHD in children, suggesting that breastfeeding may have a preventive effect on the development of ADHD [13,28-30]. However, it remains unclear if countries with a high prevalence of ADHD have lower rates of initiation of breastfeeding and/or shorter durations of breastfeeding and if maternal leave policy at places of employment affects the risk of children to acquire ADHD. The aim of the present study was to examine these issues.
We conducted a systematic search of the medical literature using the following data sources: MEDLINE, PubMed, UpToDate, Google Scholar, Clinical Key, AccessMedicine and Cochrane Reviews, in addition to specialized textbooks. Key words/terms were child, adolescent, epidemiology, prevalence, ADHD rate, ADD, attention-deficit, attention-deficit hyperactivity disorder, hyperactivity, overactivity, hyperkinetic disorder, parental leave, maternity leave, breastfeeding, breastfeeding duration, duration of maternal leave, paid maternal leave, unpaid maternal leave, and country. Special attention was addressed to comprehensive literature reviews, original population-based investigations of ADHD prevalence, large studies with a sufficient sample size, and studies using DSM diagnostic criteria for ADHD, in addition to large population-based studies of breastfeeding prevalence and duration and unbiased breastfeeding studies reflecting practices in the general population. The studies were categorized by country, and the largest available study for each country in each category (ADHD, breastfeeding) was selected for inclusion in the review. Two authors (Lucas EE, Linder N) independently selected the appropriate articles; disagreements regarding inclusion/exclusion were resolved by consultation with a third author (Kachevanskaya A).
Spearman correlation analysis was used to analyze the association of ADHD prevalence with length of paid maternity leave, unpaid maternity leave, breastfeeding-ever and breastfeeding for 6 six months or more.
Of the total 211 articles reviewed, 20 met the inclusion criteria for ADHD prevalence and 20 for breastfeeding rates/duration (one from each category for 20 countries). However, studies from 5 countries in which the unemployment rate was above 25 were subsequently excluded because the effect of maternal leave could not be estimated. The remaining countries were Australia, Canada, Denmark, France, Germany, Israel, Italy, Netherlands, New Zealand, Norway, Russia Spain, Sweden, United Kingdom, and United States. The data extracted spanned a 14-year period, from 1991 to 2014.
Table 1 summarizes the characteristics of the studies used to analyze ADHD prevalence; by country (Supplementary file references #1-15). Most of the studies based the diagnosis of ADHD on the DSM-IV. The pooled prevalence of ADHD was 7.67% (95% CI 7.5 - 8.2), with significant heterogeneity across studies (p < 0.05). The lowest prevalence rate of ADHD was found in Norway (0.95%) and the highest, in the United States (9.6%).
Table 2 summarizes the characteristics of the studies used to analyze breastfeeding initiation/duration in the same countries (Supplementary file references #16-30). The pooled prevalence of breastfeeding-ever was 88.78% (95% CI 87.34 - 89.54%). Norway had the highest rate of initiation of breastfeeding (breastfeedingever) (99%) and France had the lowest (70.8%). The pooled rate of breastfeeding for 6 months or more was 44.71% (95% CI 43.78 - 45.89%), with Norway having the highest rate (80%) and Denmark the lowest (7%).
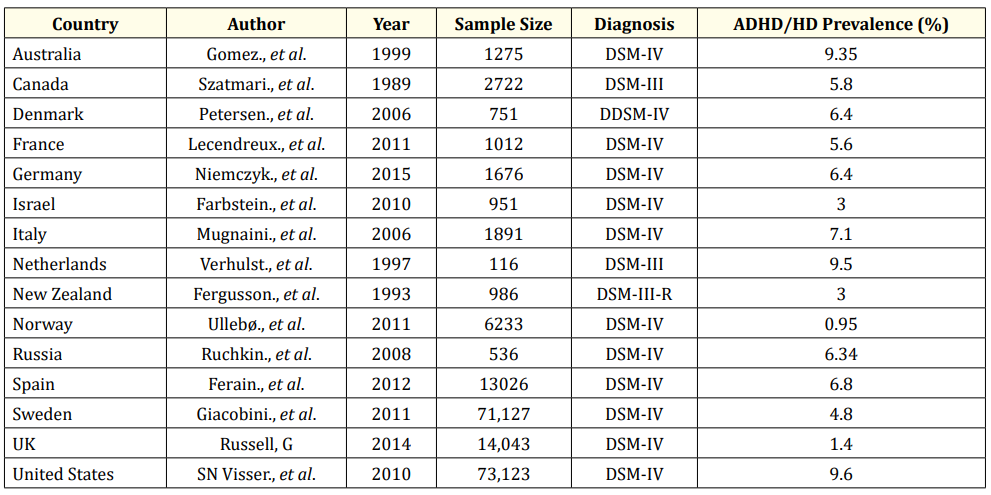
Table 1: Studies assessing the prevalence of ADHD/HD.
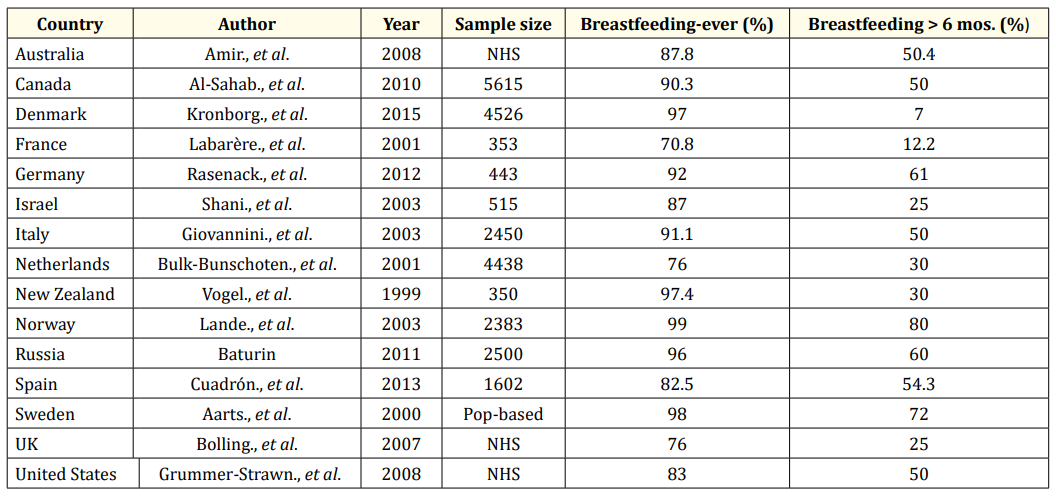
Table 2: Studies assessing breastfeeding rates. NHS: National Health Survey; Pop-based: Population-Based Survey.
Table 3 shows the number of weeks of paid leave allocated by each country. Sweden and Germany provided the most leave (47 weeks) and Australia and the United States the least (0).
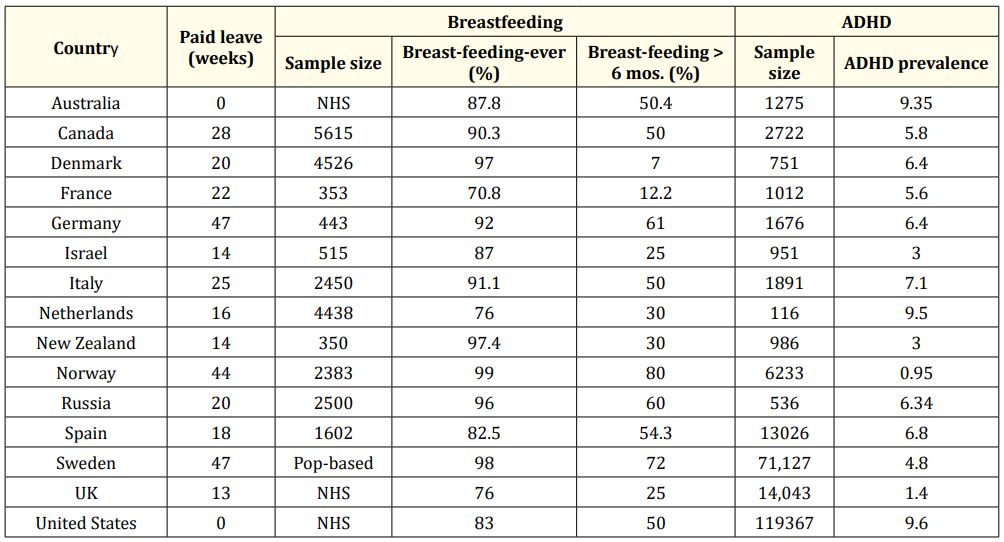
Table 3: Summary table showing paid leave, breastfeeding rates, and ADHD prevalence. NHS: National Health Survey; Pop-based: Population-Based Survey.
Spearman rank correlation test yielded a negative correlation between duration of paid leave and ADHD prevalence (Rs -0.54, p < 0.05) and between breastfeeding-ever and ADHD prevalence (Rs -0.57, p < 0.05). There was also a weak positive correlation between duration of paid leave and breastfeeding-ever (Rs = 0.4, p < 0.05). There was no correlation between breastfeeding for 6 months or longer and ADHD (Rs = -0.12, p < 0.05) and no correlation between unpaid maternal leave and breastfeeding (Rs = -0.07, p < 0.05).
We conducted a systematic review of studies investigating prevalence rates of ADHD breastfeeding, and maternity leave. We identified an inverse relationship between the duration of paid maternity leave and breastfeeding and between breastfeeding and ADHD. These findings suggest that paid maternity leave encourages breastfeeding which in turn might be connected to lower rate of ADHD in children.
The “developmental programming” is an important term in modern medical research [31]. This term describe the finding that at early development stages certain foods or nutrients, fed during limited sensitive periods, may determine developmental asset leading to clinical alterations that take place decades later and are capable of pre-programming brain development and be related to adult functional disturbances and diseases [31,32]. Given the wide heterogeneity and complex manifestations of ADHD, recent theoretical work has suggested the importance of a developmental perspective that views ADHD as a multi-factorial disorder with multiple, causal processes, and pathways through development [19,20]. The developmental perspective attempts to specify the developmental pathways that are associated with ADHD and to predict outcome of the disorder, by looking at the interaction of genetic and environmental risk factors [21]. Developmental programming has been defined as “either the induction, deletion, or impaired development of a permanent somatic structure or the “setting” of a physiological system by an early stimulus or insult operating at a “sensitive” period, resulting in long-term consequences for function” [31].
Evidence is mounting for programming effects of infant feeding. Studies have shown that mothers who experience financial problems during pregnancy are more likely to return to work more quickly after giving birth [16]. Therefore, paid maternity leave is important because it allows mothers the time to totally commit to the care of their newborn and develop a strong attachment to him/ her while free of distractions and financial constraints [14]. Since its inception in 1919, the International Labor Organization (ILO) has made the provision of child welfare and maternity protection a primary concern. The ILO Maternity Prevention Convention, 2000 (no. 183) and accompanying recommendations (no. 191) advise that women get 14 weeks’ paid maternity leave, covered by social insurance or public funds, and that “the cash benefit paid during maternity leave should be at least two-thirds of a woman’s previous earnings - or a comparable amount if other methods are used to determine cash benefits.” This should ensure “that the woman can maintain herself and her child in proper conditions of health and with a suitable standard of living” [33]. The results of the present study support these guidelines, showing that paid leave for new mothers may promote the health of their children in terms of a lesser risk of ADHD.
Today, nearly all countries have passed legislation for maternity protection at work. According to recent data reported by the ILO, of 185 countries and territories investigated, 34% follow its recommendations. This practice is supported in our results showing that ADHD occurs at high rates in almost all countries that provide less than 20 weeks’ paid leave. It is also in line with the lack of association found in the present study between unpaid maternal leave and breastfeeding. We speculate that providing leave without financial insurance is of little help to mothers from low- and middle-income families who cannot afford to take the time off [34].
In some cases, the adverse effect on breastfeeding caused by the need to leave a very young infant at home in order to return to work is compounded by separation anxiety [30], which may further exacerbate the deleterious health effects on the infant. Thus, it is noteworthy that despite the many advances in maternity leave, the large majority of female workers worldwide -some 830 million - still do not have adequate maternity protection [33].
The present review included a relatively large number of studies from many countries. We have found that ADHD has been well studied in North America and Europe but fewer studies are available from Africa and Asia. To reduce bias, we included only articles that based the diagnosis of ADHD on the DSM-IV, DSM-III or DSM-III-R. Additionally, two investigators independently selected the best reference for each country, and any disagreements were resolved by consulting a third investigator. However, the study was limited by our inability to perform a meta-analysis, which would have provided more robust information, because of variations in selected populations and methodologies among the included studies. Moreover, most of the studies derived from western countries, so the results may not be generalizable globally.
Length of paid maternity leave has a very strong negative correlation with ADHD. Thus, providing mothers with sufficient paid maternity leave may lead to closer attention given to the children and more time for breastfeeding, which may in turn lead to a decrease in incidence of ADHD.
The authors have no conflicts of interest.
No funding was received for this work.
Copyright: © 2020 Lucas Esuh Esong., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.