Monika Kasuhal1*, Mamta Bothra2 and Ayush Kaushal3
1Consultant Neonatologist, Consultant Paediatrician, Emirates Speciality Hospital, UAE
2Specialist in Pediatrician, Thumbay Hospital, UAE
3Trainee at Emirate Specialty Hospital, UAE
*Corresponding Author: Monika Kaushal, Consultant Neonatologist, Consultant Paediatrician, Emirates Speciality Hospital, UAE.
Received: February 04, 2020; Published: March 06, 2020
Citation: Monika Kasuhal., et al. “Early Suspicion of Haemophagocytic Lymphohistiocytosis Syndrome Following Influenza a Infection Complicated to ARDS Leading to Intact Survival”. Acta Scientific Paediatrics 3.4 (2020):09-12.
Haemophagocytic lymphohistiocytosis (HLH) is not rare but may be fatal. It may be complication that can progress when Influenza A confounds immunocompromised children [1]. We report a case of Haemophagocytic lymphohistiocytosis complicating an influenza A infection in a one year and 4 months old well thriving girl. The child had come with simple influenza infection which soon progressed to ARDS and multi organ failure when HLH was suspected and bone marrow was done which conformed and the other criteria were met for the diagnosis of HLH. The child was appropriately treated and supported by ECMO and could be discharged home.
Keywords: Haemophagocytic Lymphohistiocytosis (HLH); Children; Infection
Haemophagocytic Lymphohistiocytosis Syndrome (HLHS) can be primary which may have genetic predisposition or secondary that is acquired later [1]. Secondary HLHS may be secondary to either infections or malignancies. HLH complicating influenza A infection in well thriving children is quite rare. We report a one year and four-month old girl who presented with high fever, cough diagnosed to have influenza A infection later developed HLHS. Clinicians should be aware that HLHS may be a serious complication of influenza A infection.
One year four months old female child, second by order of birth, born of non-consanguineous marriage with family history of paratyphoid and Influenza A+ in sibling was brought with history of high grade fever, cough, vomiting, poor oral intake since 3 days.
On examination child was sick looking, febrile, dehydrated, and drowsy. Throat was congested and chest had bilateral crepitation and rhonchi.
Investigations at admission showed Hb 9.1, wbc 8590,N 45,L 53, platelets 3.4 lac and CRP of 6.5 Influenza A was positive. Repeat blood test showed decrease in Hb, WBC, and platelets (Table 1). Peripheral Smear showed microcytic hypochromic anemia, anisopoikilocytosis, elliptocytosis and pencil cells. MRI brain was normal and Lumbar Puncture showed RBC. Chest x-ray showed pleural effusion and later Acute respiratory distress syndrome picture. Pleural tapping revealed leucocytosis. 2DECHO revealed pulmonary hypertension. Ferritin was 5000, and high triglycerides. Bone marrow aspiration revieled marked increase in histiocytes, phagocytes suggestive of haemophagocytic lymphocytosis syndrome. HLA testing could not be done. Blood cultures were all sterile.
We considered possibility of superadded bacterial infection, encephalitis and ARDS.
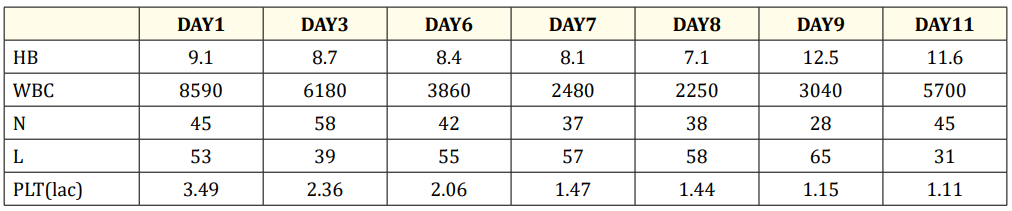
Table 1: Lab parametres.
Child was admitted and started on intravenous fluids, Tamiflu and nebulization. Fever spikes persisted. IV antibiotics Ceftriaxone was added. In view of drowsiness, MRI brain and Lumbar was done which were normal. Fever spikes persisted. Child developed generalised tonic clonic convulsions and was loaded with Phenytoin. In spite of these, fever persisted and developed respiratory distress and desaturation. Oxygen therapy started. Chest x-ray showed pleural effusion for which tapping was done. In view of increase in distress with suprasternal retractions and increased requirement of oxygen, she was intubated and put on ventilator. 2DECHO was done to rule out pulmonary hypertension. Ventilator settings had to be increased and chest X-ray showed ARDS. She had to be put on high frequency ventilator and nitic oxide therapy was started. For refractory hypotension Inotropes and hydrocortisone was added.
On ventilator she developed pneumothorax. ICD was inserted. Because of persistent fever, hepatosplenomegaly, anaemia, leukopenia along with thrombocytopenia with normal CRP we thought of haemophagocytic lymphohistiocytosis and hence ferritin and lipid profile was sent. Ferritin was 5000, and she had high triglycerides. Bone marrow aspiration confirmed the diagnosis. She was started on pulse methylprednisolone. She required ECMO, steroids.
The child was discharged uneventfully after 2 months of hospital stay.
Influenza A virus infection are generally mild and patients mostly recover completely [2]. Some H1N1 patients may have hematological findings like leucopenia, neutropenia, and idiopathic thrombocytopenic purpura [3,4]. Very rarely, HLH has been observed [3]. HLH presents as febrile disorder along with multiple organ involvement. Differential diagnosis are infections, prexia of unknown origin, liver failure, macrophage activation syndrome, or encephalitis.
In a study conducted on HLH patients 94 of 249 patients had prominent clinical signs like Hepatosplenomegaly (95%), Lymphadenopathy (33%), Neurologic symptoms (33%) and Rash (31%) [5].
Fever 38.5°C, Splenomegaly, Peripheral blood cytopenias with at least two of the following: Hb <9 g/dL, Platelets <100,000/microL, ANC <1000/microL, Hypertriglyceridemia fasting triglycerides liver, Low or absent NK cell activity, Ferritin >500 ng/mL only 80% specificity (ferritin >3000 ng/mL more indicative of HLH), Elevated soluble CD25 (soluble IL-2 receptor alpha) two SD above normal [6,7].
The differential diagnosis can include Macrophage activation syndrome, Infection/sepsis, Liver disease/liver failure - Multiple organ dysfunction syndrome, Auto-immune lymphoproliferative syndrome, Encephalitis, Drug reaction with eosinophilia and systemic symptoms, Kawasaki disease, Cytophagic histiocytic panniculitis, Thrombotic thrombocytopenic purpura, hemolytic uremic syndrome (HUS), or drug-induced thrombotic micro angiopathy, Transfusion-associated graft-versus-host disease [6-9].
Our patient had prolonged fever, fatigue, pneumonia, ARDS, pancytopenia, hepatosplenomegaly, hyperferritinemia, hypofibrinogenemia, and hemophagocytosis at bone marrow aspiration. Using criteria of HLH 2004 we could fit the diagnosis of HLH in our case [10,11].
A case in 17-year-old female patient with H1N1 influenza A related HLH who completely recovered with steroid and oseltamivir treatment was the first to be reported [12]. Following this report, 23 more patients were reported of various ages between 2 months and 61 years old [13-19]. In most of the cases, pancytopenia, hepatosplenomegaly, hyperferritinemia, hypofibrinogenemia and hemophagocytosis at bone marrow aspiration were detected [13-19].
Mc Clain., et al. had shown association of HLH with EBV virus in immune deficient children [20]. Harms., et al. confirmed in eight patients H1N1 association with HLH in autopsy [21].
Potter., et al. looked into deaths during epidemics of H1N1 in 2009 and speculated that those may be due to HLH and found 36% had developed HLH and 89% of them died [22].
As per our knowledge there is only two case report of influenza A infection complicated by HLH in a three-year-old girl [23,24]. But the survival was not possible in spite of ECMO.
One retrospective study which included 18 pediatric cases showed 88.9% cases were previously healthy and the case fatality rate was 61.1%, and all died within 2 months of disease onset. The infectious agents associated with HLH were identified in 11 cases (61.1%), and (82.7%) of them had evidence of Epstein-Barr virus (EBV) infection or reactivation [25].
Regarding specific management of HLH, intravenous immunoglobulin and steroids were the first-line agents and were administered in 16 cases and 11 cases, respectively, while etoposide was administered in 5 refractory cases during the late phase of disease [25]. We treated our patient with immunoglobulin and steroids.
As per our knowledge goes this is the only case, which survived after Influenza A, complicated by Haemophagocytic lymphohistiocytosis and ARDS. Most probably it could happen due to early suspicion and intervention.
High mortality has been reported in patients with HLH if diagnosis is delayed. Patients with early diagnosis and treatment have favorable outcomes. It also leads to prolonged viral load clearance and cytokine response.
Copyright: © 2020 Monika Kasuhal., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.