Yasser Ashour Mohamed1, Mohamed Ahmed Negm2*, Ibrahim Ahmed Gamaan1, Sayed Ahmed Elhady1 and Mohamed Mohamed Shahin1
1Department of Pediatric Surgery, Al-Azhar University, Cairo, Egypt
2Pediatric Surgery Unit, Qena Faculty of Medicine, South Valley University, Qena, Egypt
*Corresponding Author: Mohamed Ahmed Negm, M.D, Pediatric Surgery Unit, Qena Faculty of Medicine, South Valley University, Qena, Egypt. E-mail: drmohamednegm@yahoo.com Official E-mail: drmohamednegm@med.svu.edu.eg
Received: January 07, 2020; Published: February 20, 2020
Citation: Mohamed Ahmed Negm., et al. “Preliminary Experience of Glove Single Port Laparoscopic Appendectomy in Children and Adolescents for Uncomplicated Appendicitis”. Acta Scientific Paediatrics 3.3 (2020):56-61.
Background: Laparoscopic appendectomy has been widely applied and became popular procedure for the surgical management of appendicitis. Glove single port laparoscopic appendectomy [GSPLA] is a new technical modification of single incision laparoscopic surgery [SILS]. By this approach the laparoscopic instruments introduced to the abdomen through a longitudinal one umbilical incision only.
Purpose: This study aimed to present two centres initial experiences using home-made glove single port for laparoscopic appendectomy [GSPLA] in children and adolescents.
Patients and Methods: This prospective study was conducted on patients of pediatric age with uncomplicated appendicitis using GSPLA. This was done through a 2 - cm trans-umbilical longitudinal incision. Then the inner flexible plastic ring (FPR) inside the out folded glove was inserted into the abdominal cavity using a curved artery forceps. The open end of the glove was passed through the rigid outer ring (ROR) where it was stretched and folded several times around the ROR for tightening over the anterior abdominal wall. The fingers of glove act as site for introduction of [laparoscopic instruments, ports and camera.
Results: Seventy-two children with acute uncomplicated appendicitis were surgically treated by GSPLA. Their mean age was 13 ± 2.8 years (ranged from 7-16 years). All procedures were completed laparoscopically without conversion. Only two cases were converted to multiport laparoscopic procedure. The operative time was ranged from 35 - 79 (mean = 45.24 ± 12.14 min). Post- operative ileus was seen in 2 patients (2.77%) and improved under conservative treatment. No report of umbilical infection or hernia after 6 months of follow up.
Conclusion: The GSPLA is a new procedure which is very cheap, easy to be done. In addition to high flexibility and wide range of movement of the instruments in comparison with the other single incision laparoscopic trocar (SILT) devices in the market.
Keywords: Glove Single Port; Endoscopic Appendectomy; Children; Laparoscopy; One Port Endosurgery open surgery or by laparoscopy. A further development in the minimally invasive appendectomy technique has been the introduction of single incision laparoscopic appendectomy (SILAP) [1,2].
AAP: Acute Appendicitis; CLA: Conventional Laparoscopic Appendectomy; FPR: Flexible Plastic Ring; LAP: Laparoscopic Appendectomy GSPLA: Glove Single Port Laparoscopic Appendectomy; ROR: Rigid Outer Ring; SILAP: Single Incision Laparoscopic Appendectomy; SILS: Single Incision Laparoscopic Surgery; SILT: Single Incision Laparoscopic Trocar.
Appendectomy is a well-established surgical procedure for the treatment of appendicitis. The operation can be performed as an open surgery or by laparoscopy. A further development in the minimally invasive appendectomy technique has been the introduction of single incision laparoscopic appendectomy (SILAP) [1,2].
Laparoscopic appendectomy (LAP) P has been considered the best surgical choice for the treatment of appendicitis [3-5].
Esposito was the first to report the technique of SILAP in pediatric age. But it is still not a well-established technique and not widely practiced because it is ergonomically challenging when compared with multi-port laparoscopic procedure. Moreover, SILT access decreases the range of movement for the surgeon and assistant with lack of triangulation [6-8]. The commercially available SILT in addition to its high cost needs special instruments with limited range of movements especially when performed in children [9].
This study aimed to present the outcome of initial experience of SILAP using a home-made surgical glove for uncomplicated appendicitis in children and adolescents.
This prospective study included all children and adolescents with non-complicated appendicitis. The study was done in two pediatric surgery centres of Al-Azhar, Qena University Hospitals and affiliated hospitals during the period from October 2016 to January 2019. All children were subjected to laparoscopic appendectomy with GSPLA technique.
Pelvi-abdominal ultrasound was done by a senior radiologist for all patients.
The study was approved for clinical study by Ethical Research Committee. Before enrolment of the patients in this study, the parents were agreed and signed a written consent.
After history taking and thorough clinical evaluation, abdominal U/S, CBC, CRP and urine analysis were carried out. Antibiotic in the form of 3rd generation Cephalosporins (100 mg/kg BW) and Metronidazole 7.5 mg/kg BW/dose were given to all cases.
General with endotracheal intubation.
Patient position: Supine with little tilting of the table to the left side and 30- degree Trendelenburg position. Before the skin drape, the umbilicus was cleaned thoroughly with alcohol swabs and Povidone Iodine solution which was applied also from the nipple to the mid-thigh.
The home-made surgical glove single port was prepared from FPR about 4-6 cm in diameter, a rigid outer ring (ROR) with a larger size and two surgical gloves No. 6.5. The fingers end of the glove was passed through the inner FPR and the open end turned around it in the middle of the glove so to become inside the out folded glove toward glove fingers (figure 1). After infiltration of local anaesthesia around the umbilicus, a longitudinal umbilical skin incision of about two cm was done and deepened to include the fascia and peritoneum. Then 4 stay sutures were inserted to the four corners of the fascia and peritoneum for traction during insertion of FPR inside the two layers of the glove (figure 2).
Insertion of the well lubricated inner FPR to the peritoneal cavity by using a curved artery forceps. The open end of the glove was passed through the outer ROR where it was stretched and turned several times around the ROR for tightening over the anterior abdominal wall (figure 3).

Figure 1: Materials and instruments used for construction of Home-Made Glove Single Port. (A) Laparoscopic conventional instrument. (B) Elastic soft and rigid ring. (C) Re-usable 5-mm. port. (D) surgical glove.
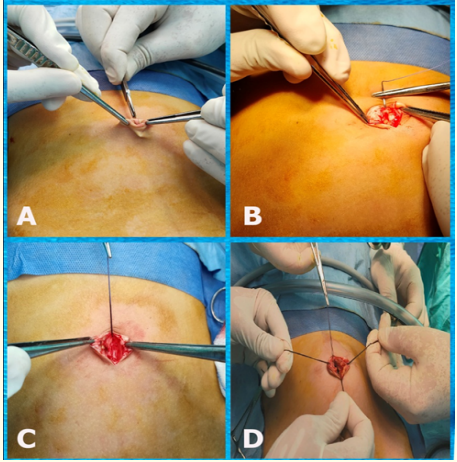
Figure 2: Steps of longitudinal umbilical incision and insertion of 4 stay sutures for traction and easy insertion of glove single port.
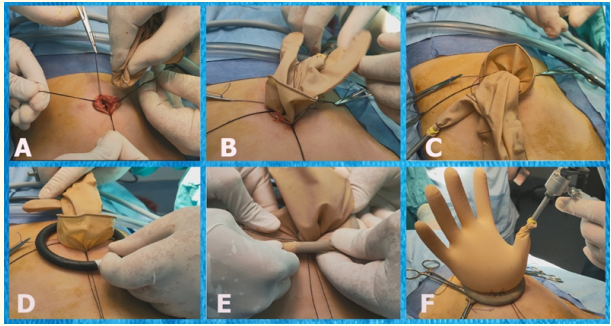
Figure 3: Insertion of home-made glove single port through umbilical incision. (A) Passing the inner ring through the umbilical incision aided by traction sutures. (B) Insertion completed (C) Insertion and fixation of the reusable working port. (D) Application of rigid outer ring. (E) Rolling of the glove over the outer ring. (F) The glove single port with complete fixation to the abdominal wall through the inner and outer ring and inflation of abdomen.
A 5-mm port was then passed inside the thumb and fixed with a piece of elastic rubber band from the tips of other glove to prevent dislodgement. This port was used for CO2 insufflation and passing the 5-mm scope into the peritoneal cavity (figure 4). Two conventional laparoscopic instruments [3-mm or 5-mm] were introduced in similar way as the scope into the fingertips of the glove without trocar (figure 4). After creation of pneumoperitoneum with pressure gradient from 8 – 12 mmHg according to child’s age, the peritoneal cavity was explored and the inflamed appendix was identified (figure 5). Then the whole peritoneal cavity was explored to exclude complicated appendicitis. The monopolar diathermy was used in heat coagulation of meso-appendix and in some cases Harmonic Scalpel was used. The base of the appendix was tied using extra corporeal Roader’s knot. One of the unused fingers of the glove was used to exteriorise the appendix. Lastly closure of umbilical wound was done after gradual deflation of the peritoneal cavity (figure 6).
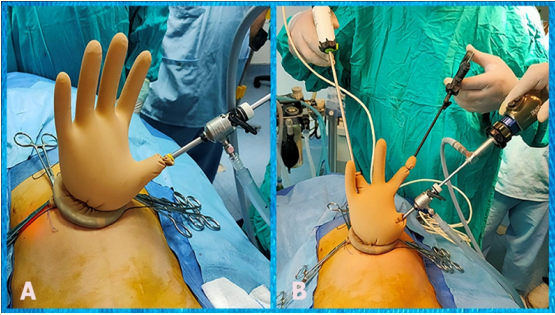
Figure 4: (A) Camera port was introduced through the thumb finger of the glove with pneumoperitoneum. (B) Position of the surgeon, camera man and the working instruments.
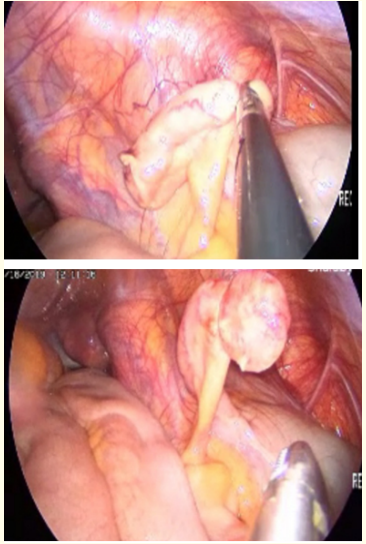
Figure 5: Intraoperative view of acute appendicitis.

Figure 6: Immediate post- operative photo of umbilical wound.
Good hydration by IV fluid, continue antibiotics as previously described, and NSAID for analgesia. All children were allowed to take clear liquid diet after returning of normal intestinal sounds and the diet was advanced gradually as tolerated. Patients were discharged home when tolerating a regular diet, usually at the morning of the second post-operative day. However, some patients were discharged home in the evening of the operative day. For more details of the technique see the following link:https://drive.google.com/open?id=1ildmUu-OGyx8jQcGoNLwvwLv-w-0jrd0
The patients were followed up at out -patient clinic weekly for the first month then monthly for 6 months.
Data were analysed using the statistical package for social sciences, version 24.0 (SPSS Inc., Chicago, Illinois, USA). Quantitative data were expressed as mean ± standard deviation (SD). Qualitative data were expressed as frequency and percentage.
Seventy-two children with AAP were included in this study. The demographic data of the patients is shown in Table 1. The appendix was accessible in 56 (77.8) cases and was challenging in [16 (22.2%)] patients. However, the majority of cases were completed by GSPLA. Five cases (6.9%) were converted to CLA due to retrocecal hidden appendix with difficult visualization of the appendix by GSPLA technique. Harmonic Scalpel was used to control the mesoappendix in 40 (58.3%) cases and by diathermy in 30 (41.7%) cases. The base of the appendix was controlled by extracorporeal knot in all patients. No cases needed conversion to open appendectomy. The operative time was ranged from 35 - 79 min. (Mean=45.24 ± 12.14 min).
Postoperative ileus was seen in 2 patients (2/72 = 2.77%) that improved conservatively. No other abdominal complications reported in this study. The mean postoperative hospital stay was 41.99 ± 6.53 hours. All patients were regularly attending the follow up for the first 3 visits and the majority were followed by telephone call only. No umbilical infection or hernia developed in the followup period which ranged from 2-6 months.
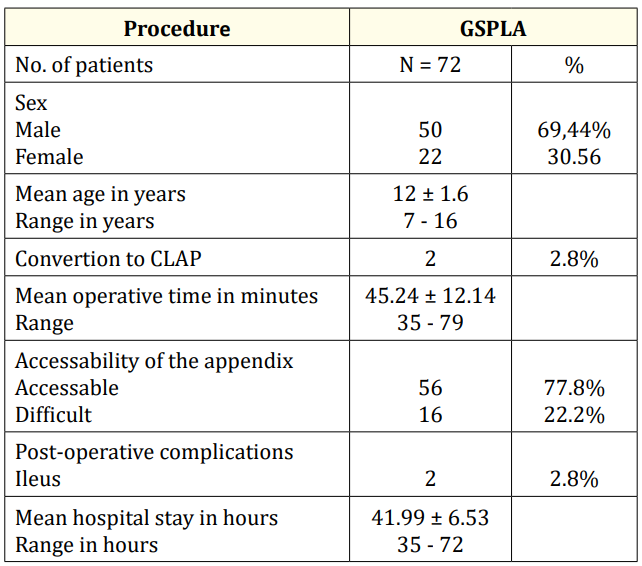
Table 1: Showing patients’ demography and the result of the study
It is well known that the surgical management of appendicitis is appendectomy. The first surgeon carried out appendectomy by laparoscopy was Kurt Semm in 1983 [10,11]. Conventional laparoscopic appendectomy (CLA) has been widely applied for the treatment of complicated and uncomplicated appendicitis [3-5].
Beside its role in confirmation of the diagnosis, laparoscopy has less postoperative pain and low doses of analgesics. It enables early activities and food intake and a short hospital stay. Thus, patients can return early to normal activities and also have fewer cosmetic problems after surgery. For these reasons, CLA is one of the most frequently performed emergency operations [12]. According to what documented in the literature by many authors, the procedure SILS has a lot of benefits to the patients as performing more than one procedure by the same approach, good patient compliance regarding post-operative pain and possibility for conversion to the classic multiport laparoscopic procedure [13-15].
In a recent study by Martynov and Lacher, they documented that there are a several shapes of SILT available in the market with curved laparoscopic instruments but, it is costly if compared with glove single port used in the current study and in country with low available resources [9]. This also agreed with Lee., et al. in their study using the same procedure with conventional laparoscopic instruments with low cost [16].
In a randomized controlled trial done by Lee., et al. comparing SILT with CLA they have documented that postoperative results were similar. However, the increased costs for SILT compared to CLA, especially when carried out by costly curved instruments is a limitation of SILT technique. However, the technique used in this study became popular and used by many authors. This may be due to its low costs and, the use of conventional laparoscopic equipment. Moreover, surgical glove port has been adopted for several minimal procedures, including cholecystectomies and appendectomies [8,17-20].
Martynov and Lacher [9] stated that the surgical equipments needed to perform SILT in children are very expensive and they added that the use of surgical glove port is not only cheap but allows a wide range of movement of the instruments without collisions”. In another study there was significant decrease of the time of surgery between SILT using conventional laparoscopic equipments compared with CLA [21].
In this study, the mean operative time of GSPLA procedure was 45.24 ± 12.14 min. (ranged from 35 to 79 mints.). The operative time for the first 2 patients was more than 64 minutes due to the early learning curve and because it took long time by the surgical team to get familiar with the technique. Then, the operative time was deceased gradually in the following cases.
Also, using the home-made surgical glove as a single port for the treatment of AAP in children and adolescents has benefits; it is easy to use and can be simply introduced into the abdominal cavity even in obese children. It permits the laparoscopic instruments to be passed through small incision. In addition, the glove acts as a barrier preventing the contact of the appendix to abdominal wall during retrieval of the appendix with no need for laparoscopic endobag especially low resource countries. The umbilical incision is small; this minimizes postoperative pain and the rate of development of infection or umbilical hernia due to the barrier effect of the glove.
Many commercial SILT have 3 or 4 ports, whereas the glove single port has ports for five instruments at the same time. Moreover, it is very cheap than the other SILT available in the market. The elasticity of the surgical glove single port permits a good range of movements of the instruments with enough triangulation with minimal collision. When additional instruments were needed, a small cut was made in the tip of the gloves port without using a trocar and tied with a previously prepared elastic strip [9,16].
According to the present study, the GSPLA technique has been shown to be not only feasible but also safe and effective, with a short learning curve. A team work between the surgeon and camera man is very important to carry out the technique smoothly and rapidly. Smoke that result from monopolar diathermy somewhat is another problem that may slow the procedure as there is no separate venting channel in cases of GSPLA.
In the current study, all cases were completed laparoscopically using GSPLA except 5 (6.9%) cases needed insertion of assassinating instrument [3 with multiple adhesions and 2 with retrocecal position of the appendix. No case needed conversion to open surgery and this agreed with Lee., et al. in their study comparing home–made port with conventional laparoscopic procedure [16]. Pittman-Waller., et al. earlier stated that in their study, a higher conversion rate was present with SILT due to technical difficulties where complicated appendicitis was present in 30% of their cases [22].
In this study, early mobilization was advised and the majority of patients were usually discharged on the second post-operative day. The mean postoperative hospital stay was ranged from 35 - 72 (Mean of 41.99 ± 6.53 Hours).
The clinical limitation of the present study is its application in only non-complicated appendicitis and the small number of cases. But this may be explained by our initial results with early learning curve to be familiar of this technique. Larger numbers together with long term follow up of cases are needed to support the idea of this technique in the future.
The glove single-port laparoscopic appendectomy is a new technique which is cheaper than the other SILT devices. According to the results of this study, laparoscopic appendectomy in pediatric age using the home-made glove single port is quite easy to be done for non-complicated appendicitis with short learning curve. This technique provides high flexibility and wide range of movements of laparoscopic instruments.
All authors would like to thank and appreciate Rafik Shalaby, Professor of Pediatric Surgery and innovator of laparoscopic surgery, Al-Azhar University, Cairo, Egypt for his encouragements and support for mastering this technique and meticulous revision of this article.
None.
None.
Copyright: © 2020 Mohamed Ahmed Negm., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.