Noudamadjo A1, Assoklé J1*, Agossou J1, Adédémy JD1, Assoklé J1, Agbeille F2 and Akpona S1
1
Faculty of Medicine, University of Parakou, and Borgou-Alibori Departmental
Hospital, University Centre (CHUD-B/A), Benin
2 Borgou-Alibori Departmental Hospital, University Centre (CHUD-B/A), Benin
*Corresponding Author: Assoklé J, Faculty of Medicine, University of Parakou, and Borgou-Alibori Departmental Hospital, University Centre (CHUD-B/A), Benin.
Received: November 21, 2019; Published: December 30, 2019
Citation: Assoklé J., et al. “Hypovitaminose D Chez the Enfants of 6 to 59 Months Suffering Serious Paludisme in the Pediatria Service in CHUD-B/A in 2016”. Acta Scientific Paediatrics 3.1 (2020):47-50.
Objective: To calculate the frequency of hypovitaminosis D in children aged 6 to 59 months with severe malaria in the paediatricward ward at CHUD-B/A in 2016.
Frame and Methods: This is a descriptive and analytical cross-sectional study. The data collection was forward-looking. Included in the study were children aged 6 to 59 months hospitalized for severe malaria in the pediatric ward of CHUD-B/A; hiv-infected, eutrophic and who have not had vitamin D supplementation in the past 6 months. Vitamin D was boosted by the High Performance Liquid Chromatography (HPLC) technique.
Results: A total of 80 subjects are included in the survey. The average age was 26.08 months, the sex ratio was 0.8 and the average weight was 10.80 kg. The frequency of hypovitaminosis D was 83.8% (67 cases out of 80 children surveyed) with an average plasma concentration of vitamin D of 21.57 ng/ml - 7.34 with both extremes (11.24-42.32) ng/ml. The minimum parasitemia is 202 P/l and the maximum is 580,000 P/l.
Conclusion: Hypovitaminosis D is common in children with severe malaria. this result suggests that a large-scale community study should be conducted to decide whether vitamin D should be considered in national policies for supplementation and management of severe malaria.
Keywords: Vitamin D; Severe Malaria; Children
Hypovitaminosis, given the high sun in Africa in the Sub-Sahara should be exceptional. However, certain factors (dark skin colour, poor nutritional intake) may predispose children to vitamin D deficiency which, if any, may affect malaria morbidity and mortality given its role in the immune system [1-3].
The objective of this trava was to calculate the frequency of hypovitaminosis D in children aged 6 to 59 months hospitalized for severe malaria in the pediatricward ward of CHUD-B/A in 2016.
Calculate the frequency of hypovitaminosis D in children 6 to 59 months hospitalized for severe malaria in the pediatricward ward of CHUD-B/A in 2016.
This is a descriptive and analytical cross-sectional study. The data collection was forward-looking. Included in the study were children aged 6 to 59 months hospitalized for severe malaria in the pediatricward ward of CHUD-B/A; hiv-infected, eutrophic and who have not had vitamin D supplementation in the past 6 months. Vitamin D was boosted by the High Performance Liquid Chromatography (HPLC) technique.
From May 2016 to July 2016, eighty (80) hospitalized severe malaria cases meeting the inclusion criteria were recorded for this study. Among the eighty-eight children, sixty-seven (67) suffered from vitamin D deficiency, a frequency of 83.8% with IC [73.8- 91.1]. Thus: 3.8% of these children had a severe deficit; 47.5% a moderate deficit and 32.5% a small or insufficient deficit.
Figure 1 shows the distribution of hypovitaminosis D.
The average age of patients in our series was 26.08 - 13.16 months and ranging from 7 months to 59 months.

Figure 1: Distribution of hypovitaminosis D in children aged 6 to 59 months hospitalized for severe malaria in pediatrics in 2016.
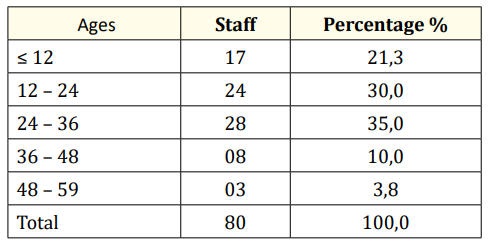
Table 1: Distribution of children aged 6 to 59 months hospitalized for severe malaria in the paediatric ward by age group in 2016.
Of the eighty (80) children, forty-four (44) children were female (55%) and thirty-six (36) male (45%) and the sex ratio between boys and girls (g/f) was 0.8.
The table shows that 37.5% of the children had the rank of siblings greater than three (03). In Table 2, the distribution of children according to their rank in the siblings is presented.

Table 2: Breakdown of children aged 6 to 59 months hospitalized for severe malaria in the paediatric ward according to their rank in the siblings in 2016.
The mothers of the children included resided in rural areas in 73.8% of cases, 57.5% lived in a monogamous household. 72.5% were uneducated women.
Table 3 shows the environment of residence, the type of family and the level of education.

Table 3: Breakdown of mothers or caregivers by setting of residence, family type and education.
Mothers or babysitters had corn or mil/sorghum or yam as their staple food in 47.5% of cases. Of the eighty (80) children, 92.5% were breastfed alone and 53.8% were exclusively breastfed for a period of less than six (6) months.
Table 4 shows the distribution of the basic food, the type of breastfeeding and the duration of breastfeeding (AM).
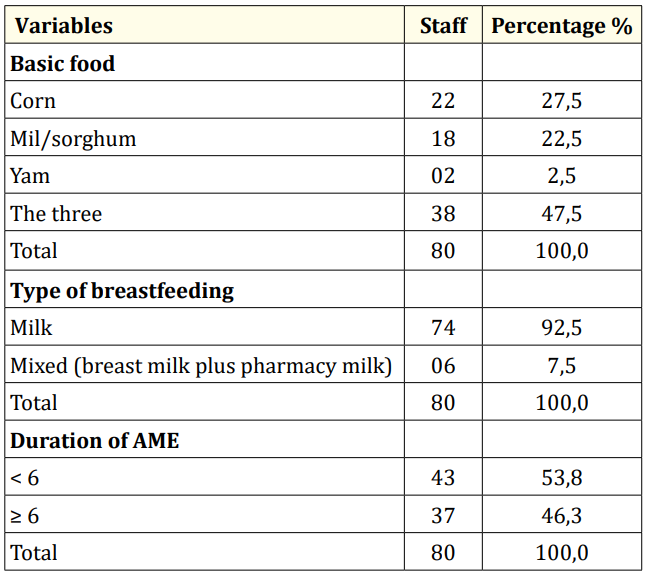
Table 4: Distribution of children aged 6 to 59 months hospitalized for severe malaria in paediatrics by basic food, type of breastfeeding and duration of exclusive breastfeeding in 2016.
Of the eighty (80) children included in the study, 75% of children were not breast-feeding early, 77.5% were subjected to the family dish and only 10% had a fruit juice snack.
Table 5 shows the distribution of children included in the study based on the time it takes to breastfeed after birth, the age of weaning, the type of complementary food and the type of snack.
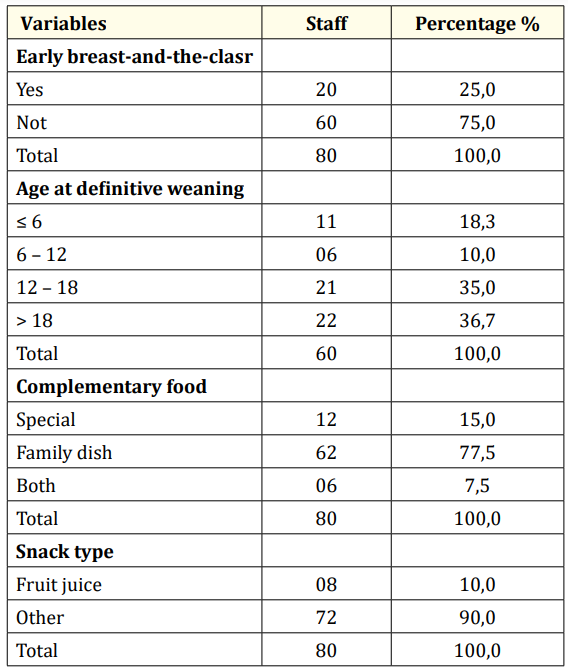
Table 5: Distribution of children aged 6 to 59 months hospitalized for severe malaria in paediatrics by delay in breast-feeding after birth, age of weaning, type of complementary food and type of snack in 2016.
At the end of the study, the frequency of hypovitaminosis D in the CHUD-B Pediatrics department was 83.8% in children aged 0659 months.
This frequency is similar to those reported (80%) Uganda by Sarah et al in their 2014 study of 18-month-old children with severe malaria [4].
This high frequency (83.8%) found in children in our study despite adequate sun exposure, highlighted by the average duration of sun exposure 2.34h versus 10 to 15 minutes recommended and the lack of relationship between vitamin D deficiency and duration of exposure can be explained by the combination of several factors such as:
Other studies in children suspected of rickets by Anath et al (83.3%) respectively in their study of 06-month-old children in 2013 in Tanzania [11], by Henry et al (80%) 2015 among children aged 06 to 24 months in Uganda [12] and by Timothy et al (60%) in Malawi in 2013 in children aged 24 months [13] showed lower frequencies than in our study. Similarly in Nigeria, in 2000, Tom et al [14] regained a frequency (37%) children aged 05 to 35 months with rickets.
Because the frequency of hypovitaminosis D is higher than that found in these different studies in children suspected of rickets, one would think that malaria is more a purveyor of hypovitaminosis D in children than rickets. But also one might think that the children included in the study were deficient in vitamin D without bone manifestation before having their malaria severe or that they had a normal plasma concentration of vitamin D but exhausted by the development of severe malaria. In all cases, this result suggests that a community study should be conducted on clinically healthy children.
At the end of this work, during which we are proposed to evaluate the frequency of hypovitaminosis D in children with severe malaria in the paediatric ward at CHUD-B/A in 2016, we can remember that hypovitaminosis D is common in children with severe malaria on the cob of high sunlight and is associated with an increased likelihood of severe malaria in children.
Copyright: © 2020 Assoklé J., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.